INTRODUCTION
Caries treatment at the cervical area of the tooth frequently requires some excision of gingival tissue to expose the decay, allowing for preparation of the tooth and then the placement of an adhesive restoration. The presence of cervical caries often presents with marginal inflammation that makes restoration placement challenging if there is hemorrhaging into the site during placement that leads to compromised bond strength and discoloration of the resin marginally.
Various methods have been advocated for gingival modification, including dissection with a scalpel, electrosurgery, modification with a rotary instrument (bur or diamond), and the use of lasers. The use of these methods present some clinical challenges that may affect the clinical results sought by the practitioner. Rotary instruments and scalpels yield a bleeding edge that may affect a restoration’s final results, especially when moderate inflammation is present at the gingiva prior to excision. Electrosurgery, although having hemostatic properties, has been associated with gingival recession following healing of the cut area, which may have negative effects on aesthetics.1 On the other hand, soft tissue accepts laser modification without resulting inflammation or tissue shrinkage during healing and, in addition, demonstrates quicker healing than with electrosurgery.2,3
 |
 |
| Figure 1. Initial presentation of tooth No. 6 with cervical caries that extended subgingivally. | Figure 2. A periapical radiograph demonstrated poor marginal adaption with recurrent caries involving the previously placed crowns on teeth Nos. 5 and 7. |
Benefits of Using a Laser
The benefit of the laser for gingivectomy is that the cut edge is nonbleeding due to the hemostasis properties of the laser.4 Lasers, depending on their wavelengths, have varying depths of hemostasis, with the Er:YAG having a thin coagulation layer and lack of in-depth hemostasis and the diode laser having the widest coagulation layer.5 This is of particular benefit when placing a restoration adjacent to the altered tissue at the same appointment due to the elimination of any hemorrhaging that can affect the bond strength of the resin restoration being placed and the resulting shade of the restoration. This also applies to gingivectomies and sulcus alterations related to crowns and bridges, where hemorrhage can hamper the impression capture at the margins of the preparation. Additionally, unlike the other methods mentioned, laser gingivectomy may be done without the need for local anesthesia. However, the use of a topical anesthetic may be indicated in some patients who may exhibit a higher degree of sensitivity.
The cervical tooth structure also requires preparation to remove any affected enamel and dentin. This is typically done using a rotary instrument with a local anesthetic. The Er:YAG laser permits the removal of affected tooth structure without the need for a local anesthetic in most patients.6,7 Wong7 reported that, when considering the need for local anesthesia for the management of treatment discomfort during tooth preparation, there was less discomfort with the laser than was experienced with traditional handpieces. This matches the clinical observations found by the authors. The hard-tissue laser has a selective removal effect on the tooth structure being prepared. As the laser has an affinity for water, the higher the water content, the more energy is absorbed and the greater the ablation of that tissue. Carious dentin has a higher water content then unaffected dentin; thus, the Er:YAG laser selectively removes the affected dentin and leaves the unaffected dentin with an increased microhardness of residual caries-affected dentin, changing its surface morphology and chemical composition.8,9 It has been reported that the Er:YAG laser influences the acid resistance of an irradiated substrate, providing control over the development of recurrent caries around composite resin restorations.10,11
 |
 |
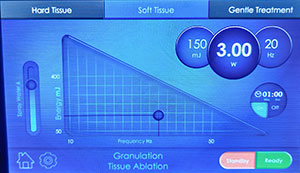
| Figure 3. The LiteTouch Er:YAG laser (integrated dental systems [ids]) was set to Granulation Tissue Ablation under the Soft Tissue setting in preparation for removal of the gingival tissue overlaying the cervical caries. | Figure 4. The LiteTouch Er:YAG laser tip was placed at the mesial with the tip contacting the tooth. The tip was then initiated and moved to the distal of the tooth to trim the gingival tissue. |
 |
 |
| Figure 5. Gingival tissue removal was continued with the LiteTouch Er:YAG laser to fully expose the cervical caries. | Figure 6. The LiteTouch Er:YAG laser was set to Enamel (under the Hard Tissue setting) to begin caries removal marginally around the affected tooth structure. |
 |
 |
| Figure 7. The LiteTouch Er:YAG laser tip was utilized at the gingiva to produce a preparation margin on nonaffected tooth structure. | Figure 8. The LiteTouch Er:YAG laser was then set to Dentin (under the Hard Tissue setting). |
The Er:YAG laser, when used for enamel surface preparation, produces irregular and indistinct morphologic changes that are different from those produced after acid etching.12 Thus, pre-conditioning with the laser was reported to significantly decrease microleakage of the enamel margins, reducing dye penetration irrespective of whether the enamel surfaces were moist or dry.13 Microleakage of water-contaminated, acid-etched teeth was significantly greater. Clinically, this will prevent stain penetration at the restoration margins over time. Based on reported results, the application of an Er:YAG laser on the enamel and dentin during restoration preparation for the placement of bonded materials (ie, a resin composite or resin fissure sealant) or resin-modified glass ionomers may be an alternative etching method to conventional acid etching.14
CASE REPORT
Diagnosis and Treatment Planning
A 76-year-old female patient presented complaining about a “dark spot” on her “front tooth.” The medical history was reviewed, and no past contraindications for treatment were found. Examination noted caries on the facial surface of the right maxillary canine (tooth No. 6) that extended subgingivally (Figure 1). Old resin composite was noted on the mesial of the crown on the right first premolar, and crowns were present on teeth Nos. 5 and 7. There was no sensitivity in tooth No. 6. The gingival tissue was non-inflamed and did not bleed upon probing. A periapical radiograph was taken to evaluate the extent of caries (Figure 2). Caries were noted at the margins on the first premolar and lateral incisor, likely related to the poor fit and open margins of the previously placed crowns. No apical pathology was noted on teeth Nos. 5 to 7. It was recommended that the defective crowns on the first premolar and lateral incisor be replaced and that a direct composite restoration be done on the canine. After discussing with the patient, she accepted the treatment recommendations and wished to start with the repair of the “dark spot” on tooth No. 6 first.
Clinical Protocol
No topical or local anesthetic was utilized. Since the caries on the facial of the canine extended below the soft tissue, some gingiva would be excised to improve operative access to remove the carious tooth structure and place the composite restoration. The wide band of keratinized tissue present would allow minimal gingival recontouring without compromising long-term periodontal health. It should be noted that when an insufficient band of keratinized tissue is present, gingival recontouring compromises long-term periodontal health, and flap elevation or gingival repositioning is required to access the root caries.
The LiteTouch Er:YAG laser (integrated dental systems [ids]) was set to Granulation Tissue Ablation (under the Soft Tissue setting) in preparation to remove the gingival tissue overlying the cervical caries using a 1.0-mm-wide Sapphire cylindrical tip (Figure 3). Gingival tissue was excised (150 millijoules [mj], 3.0 W at 20 Hz) using water to (1) cool the tissue, (2) flush any debris during cutting, and (3) eliminate any odors during the procedure. The laser tip was placed at the mesial with the tip contacting the tooth at the distal aspect of the gingival papilla to spare the papilla and to avoid the creation of a “black triangle” following tissue removal. When used in the Soft Tissue setting, the energy will allow ablation (cutting) of soft tissue with no alteration of the hard tissue; this is the case even when the tip is in direct contact with hard tissue, such as bone or tooth structure. The laser was initiated, and then gingival tissue was excised by moving the tip to the distal across the cervical part of the tooth to expose the affected cervical tooth structure (Figure 4). It is recommended to be conservative in gingival tissue removal and realize that it may require several passes to fully expose the root caries (Figure 5).
 |
 |
| Figure 9. The remaining decay was removed on the dentin aspect of the preparation with the tip of the LiteTouch Er:YAG laser. | Figure 10. The LiteTouch Er:YAG laser was set to Enamel Conditioning (under the Gentle setting) to condition the enamel margins. |
 |
 |
| Figure 11. The LiteTouch Er:YAG laser tip was utilized to condition the enamel at the preparation margins in place of acid etching to improve bonding to this aspect of the preparation. | Figure 12. The completed preparation was then ready for placement of the composite restoration. Note the lack of bleeding gingivally that would otherwise have adversely affected the final color of the composite and the resin-to-tooth bond strength. |
 |
 |
| Figure 13. The adhesive (G-Premio BOND [GC America]) was applied to the enamel and dentin aspects of the preparation, air-thinned, and light-cured. | Figure 14. A nanohybrid composite (G-ænial Sculpt [GC America]) was placed into the preparation to full contour and then light-cured. |
 |
 |
| Figure 15. The completed direct resin restoration immediately following polishing and finishing. | Figure 16. Postoperative photo at 2 weeks following the gingival recontouring and composite restoration placement. Note the healthy gingival tissue and absence of inflammation. |
The LiteTouch Er:YAG laser was then set to Enamel under the Hard Tissue setting to use 300 mj, 7.5 W at 25 Hz with water to begin caries removal marginally around the affected tooth structure utilizing the same tip as was used for the gingival tissue removal (Figure 6). The laser tip was utilized at the gingival aspect of the affected tooth structure to produce a preparation margin on non-affected tooth structure (Figure 7). Then the superior aspect was prepared under the Enamel setting, creating an area of unaffected enamel that the restoration will be bonded to when it is placed. When the inferior aspect of the area to be prepared is apical to enamel, it will be prepared using the Dentin setting (under the Hard Tissue setting).
The laser was then set to Dentin to use 250 mj, 5.0 W at 20 Hz with water (Figure 8). This lower wattage and higher millijoules setting takes advantage of the higher water content of the dentin, allowing removal of tooth structure without initiating a pulpal response. In this way, the preparation can be accomplished without the need for anesthetic, and the patient will remain comfortable during the procedure. All discolored and affected dentin was removed to complete the preparation in anticipation of the placement of a direct bonded restoration (Figure 9). The laser eliminates the need for acid etching the enamel surfaces, providing a bondable surface that is equal or superior to those traditional methods. The laser was then set to Enamel Conditioning under the Gentle setting to condition the enamel margins using 20 mj, 0.4 W at 20 Hz with water (Figure 10). Then the tip was moved over the enamel margins (using a selective-etch approach) to leave a frosted appearance once completed (Figure 11). The preparation was then ready for placement of the direct composite restoration (Figure 12).
The area was isolated with cotton rolls and dried with oil-free air in preparation for placement of the composite resin. A universal, eighth-generation bonding agent (compatible with total-etch, self-etch, and selective-etch techniques) (G-Premio BOND [GC America]) was applied to the enamel and dentin aspects of the preparation, air-thinned, and then light-cured for 20 seconds (Figure 13). Next, a nanohybrid composite (G-ænial Sculpt [GC America]) was placed into the preparation to full contour and light-cured for 20 seconds (Figure 14). Finishing and polishing was done using finishing carbide burs and diamonds (Henry Schein Dental) in a high-speed handpiece, along with water. The completed restoration can be seen in Figure 15. Note that, although the gingival edge presents with a raw cut, no active hemorrhaging was present.
The patient returned 2 weeks later for initiation of the other planned dental treatment on teeth Nos. 5 and 7. Examination of the previously placed restoration on tooth No. 6 revealed that the gingival area that had been modified with the Er:YAG laser demonstrated no inflammation and with a healthy periodontal appearance (Figure 16). She reported that she experienced no postoperative sensitivity in the soft tissue or tooth immediately following treatment or over the subsequent period of time. Further, she indicated that, other than knowing that the area had been treated, she felt that nothing had been done to the area due to the lack of any sensation both during and after treatment, and a pain-free experience resulted. The chronically inflamed papilla between the canine and first premolar, which was present at the outset of treatment and due to the previously placed adjacent restoration, was expected to improve with the replacement of the faulty crown on the first premolar.
CLOSING COMMENTS
Caries in the cervical region of the tooth can frequently involve subgingival extension of the lesion. This often requires some gingival modification to properly access the caries and accurately prepare the tooth for restoration placement. As demonstrated in this case presentation, the Er:YAG all-tissue laser can be used for gingival modification to access the carious root structure and for the preparation of the enamel and dentin prior to placement of a composite resin restoration. This can frequently be done without the need for local anesthetic, thus improving the treatment experience for the patient.
References
- Hall HD, Williams VD. Exaggerated tissue response to electrosurgery. Gen Dent. 1988;36:303-305.
- Monteiro L, Delgado ML, Garcês F, et al. A histological evaluation of the surgical margins from human oral fibrous-epithelial lesions excised with CO2 laser, diode laser, Er:YAG laser, Nd:YAG laser, electrosurgical scalpel and cold scalpel. Med Oral Patol Oral Cir Bucal. 2019;24:e271-e280.
- Yoshino T, Aoki A, Oda S, et al. Long-term histologic analysis of bone tissue alteration and healing following Er:YAG laser irradiation compared to electrosurgery. J Periodontol. 2009;80:82-92.
- Onisor I, Pecie R, Chaskelis I, et al. Cutting and coagulation during intraoral soft tissue surgery using Er:YAG laser. Eur J Paediatr Dent. 2013;14:140-145.
- Kazakova RT, Tomov GT, Kissov CK, et al. Histological gingival assessment after conventional and laser gingivectomy. Folia Med (Plovdiv). 2018;60:610-616.
- Li T, Zhang X, Shi H, et al. Er:YAG laser application in caries removal and cavity preparation in children: a meta-analysis. Lasers Med Sci. 2019;34:273-280.
- Wong YJ. Caries removal using lasers. Evid Based Dent. 2018;19:45.
- Valério RA, Galo R, Galafassi D, et al. Four-year clinical prospective follow-up of resin composite restoration after selective caries removal using Er:YAG laser. Clin Oral Investig. 2019 Nov 4. [Epub ahead of print]
- Polizeli SAF, Curylofo-Zotti FA, Valério RA, et al. Selective removal of necrotic dentin in primary teeth using laser irradiation: one-year clinical evaluation of composite restorations. J Lasers Med Sci. 2019;10:108-116.
- Colucci V, de Souza Gabriel AE, Scatolin RS, et al. Effect of Er:YAG laser on enamel demineralization around restorations. Lasers Med Sci. 2015;30:1175-1181.
- Al-Maliky MA, Frentzen M, Meister J. Laser-assisted prevention of enamel caries: a 10-year review of the literature. Lasers Med Sci. 2020;35:13-30.
- Akhoundi MSA, Etemadi A, Nasiri M, et al. Comparison of enamel morphologic characteristics after conditioning with various combinations of acid etchant and Er:YAG laser in bonding and rebonding procedures: a SEM analysis. J Dent (Tehran). 2017;14:144-152.
- Güçlü ZA, Hurt AP, Dönmez N, et al. Effect of Er:YAG laser enamel conditioning and moisture on the microleakage of a hydrophilic sealant. Odontology. 2018;106:225-231.
- Luong E, Shayegan A. Assessment of microleakage of class V restored by resin composite and resin-modified glass ionomer and pit and fissure resin-based sealants following Er:YAG laser conditioning and acid etching: in vitro study. Clin Cosmet Investig Dent. 2018;10:83-92.
Dr. Kurtzman is in private general dental practice in Silver Spring, Md, and a former assistant clinical professor at the University of Maryland in the departments of restorative dentistry and endodontics and a former American Academy of Implant Dentistry (AAID) Implant MaxiCourse assistant program director at the Howard University College of Dentistry. He has lectured internationally on the topics of restorative dentistry; endodontics, implant surgery, and prosthetics; removable and fixed prosthetics; and periodontics and has more than 700 published articles globally, as well as several e-books and textbook chapters. He has earned Fellowship in the AGD, the American College of Dentists, the International Congress of Oral Implantology (ICOI), the Pierre Fauchard Academy, and the Academy of Dentistry International; mastership in the AGD and ICOI; and Diplomate status in the ICOI, the American Dental Implant Association, and the International Dental Implant Association. Dr. Kurtzman serves on Dentistry Today’s editorial advisory board and is listed as one of its Leaders in Continuing Education. He can be reached at dr_kurtzman@maryland-implants.com.
Disclosure: Dr. Kurtzman has received honoraria from integrated dental systems for speaking and writing.
Dr. Favia is in private general practice in Arlington Heights, Ill, and a 1993 graduate of the Loyola University School of Dentistry. He has studied at the Pankey Institute and the Dawson Academy. He is a member of the ADA, the Illinois State Dental Society, the Chicago Dental Society, the American Equilibration Society, the Stuart Dental Study Club, and the AAID. He can be reached via email at molrman@sbcglobal.net.
Disclosure: Dr. Favia reports no disclosures.
Related Articles
Hard-Tissue Laser Applications: Optimizing Restorative Treatment
Management of Oral Viral Lesions With a Diode Laser
Know the Risks Before Adding Phlebotomy to Your Dental Practice











