INTRODUCTION
Dental phobia is a common occurrence in all patients. Adults may avoid dental care due to the fear of pain that they perceive will occur related to either the local anesthetic injection or during caries removal. This can be especially traumatic for pediatric patients, who can be uncooperative following the sensation of an injection.1 The need to use local anesthetic may be required prior to use of a drill and can be traumatic for many patients. When we add the sound of the drill, along with its vibration on the tooth, this can make for a stressful appointment for not only the patient but also the doctor and staff. Additionally, few patients like the lingering anesthetic effect lasting for an hour or longer after the treatment appointment.
Technology, in the form of hard-tissue lasers, frequently allows treatment without the need for local anesthetic administration. The vibration associated with the dental handpiece during tooth preparation and caries removal is eliminated as the laser vaporizes the tooth structure it’s focused on without the need for physical contact and the associated transmitted vibration of the tooth. Additionally, the “whine” of the handpiece is also eliminated and replaced with a cyclic, low click-like sound, which patients report to be better accepted. When patient stress is decreased, patients are less likely to avoid treatment and seek care before the actual intraoral pain surpasses the feared pain of treatment. Thus, providing a more comfortable experience for patients aids in their accepting and following through on dental care at earlier stages. Using a laser for tooth preparation is slower than handpiece preparation but does not require an appreciable increase in preparation time. As with the handpiece, when water is not used for tooth preparation with the laser, some odors may arise that the patient finds objectionable. However, the laser does have a water spray that, in addition to eliminating any odors, also cools the tooth and flushes debris from the area being prepared. A study found that even with the increase in preparation time, adolescent patients preferred a laser to a traditional handpiece.2
Laser Tooth Preparation
Adhesive dentistry (direct restorations) dictates that the more native tooth structure that can be preserved, the better the long-term prognosis. The Er:YAG laser allows the practitioner to selectively remove carious tooth structure while preserving healthy enamel and dentin for truly minimal invasive dentistry. The harder the substance that is being cut, the slower the cutting and the higher the energy required will be. This works to the practitioner’s benefit as demineralized dentin and enamel are less hard than the surrounding unaffected tooth structure and tooth structure is preserved during preparation.
 |
| Figure 1. The LiteTouch (ids) Er:YAG laser offers compact design and is easily portable between operatories. |
What may be confusing with the Er:YAG laser is power vs energy. Power output is measured in watts (W), which ranges between 1.0 and a peak output of 8.4 W Energy is measured between 100 to 700 millijoules (mJ) when doing hard-tissue applications, indicating the power at each pulse of the laser. The laser output is pulsed energy and is measured in hertz (Hz) with a range of 10 to 50 Hz which signifies the rate of pulse (on vs off). The faster the pulse rate (higher hertz) the more “on/off” cycles occur and the shorter the energy at the surface is. Conversely, the shorter the pulse rate (lower hertz), the longer the energy is on the surface at each pulse. When cutting harder materials (eg, enamel), a lower hertz is required to have more energy at each pulse. Softer materials (eg, carious dentin) require less energy to cut, so a higher hertz rate is used so that less energy contacts the surface at each pulse. These 3 factors can be adjusted by the practitioner. Tooth structure comprises enamel and dentin, and these require different laser settings for efficient cutting. Enamel preparation is set at 300 mJ and a pulse frequency of 20 to 25 Hz, whereas dentin being less hard than enamel requires 200 to 300 mJ and 20 to 25 Hz. When deeper caries are encountered, decreasing laser energy is advised to decrease accidental pulp exposure and avoid pulpal irritation, thereby giving more cutting control to the practitioner. When preparing pits and fissures for minimal caries removal and sealing, less energy is required so that the laser does not prepare deep into the tooth. The laser is set at 50 to 100 mJ and 20 Hz.
There has been concern around the pulpal effects of laser energy, especially given the larger pulps of deciduous teeth, in that the use of hard-tissue laser energy may cause pulpal changes that can ultimately require endodontic treatment. Several studies have demonstrated that the Er:YAG hard-tissue laser is appropriate for caries removal in primary teeth.3-5 As lower energy is required for the photoablation of primary enamel and dentin (compared to permanent enamel and dentin) due to a higher presence of water and lower presence of minerals, adverse pulpal changes have not been reported.6 The higher the water content of the tissue and the lower the mineralization, the less energy for cutting is required.7 Thus, dentin that is less mineralized and has higher water content than enamel needs less energy for preparation. Carious dentin has less mineralization and typically higher water content than unaffected dentin and cuts faster at lower energy. Additionally, deciduous teeth have less mineralization than permanent teeth and will also require less energy for preparation. This should be taken into consideration when setting the laser. The authors advise that the lowest power output to prepare the hard tissue to achieve ablation (cutting) be used. When that output is not cutting efficiently, the energy is increased until efficient cutting occurs.
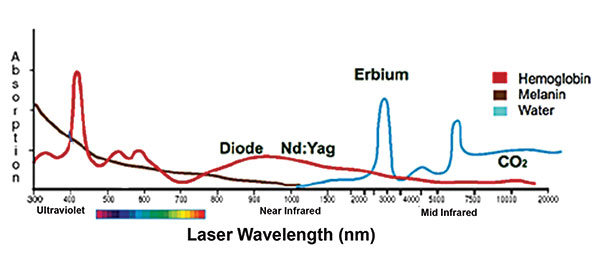 |
| Figure 2. Lasers used in dentistry, and their affinity for oral materials. |
One study reported that Er:YAG laser irradiation resulted in a 56% reduction in primary enamel surface lesion depth compared to an acid-etched group as well as a 39% decrease in root surface lesion depth.8 This appears to be related to the laser’s bactericidal effects in the caries-affected dentin and beyond.9 Er:YAG laser irradiation has bactericidal and dentin conditioning effects.10 There is also less post-treatment sensitivity in teeth treated with the Er:YAG laser vs traditional cavity preparation methods. Lasers can also treat hypersensitive root surfaces with minimum invasiveness, demonstrating effective results.11,12 Additionally, lasers have a bactericidal effect on the dentin, leaving a decontaminated surface for the bonded restoration, improving bond strength. This decreases the pulpal flare-ups that can cause tooth sensitivity and the possible need for endodontic treatment.
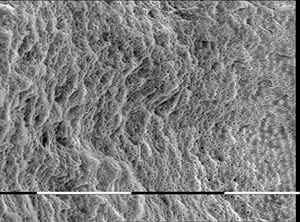 |
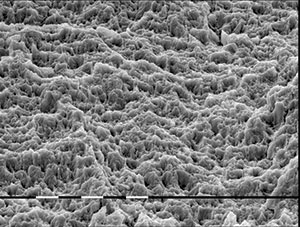 |
| Figure 3. Dentin surface following caries removal with the LiteTouch Er:YAG laser demonstrating a lack of smear layer. (Image courtesy of Prof Georgi Tomov, Medical University of Plovdiv, Bulgaria.) | Figure 4. Enamel surface following treatment with the LiteTouch Er:YAG laser, showing an enhanced bondable surface with a uniform, roughened surface. (Image courtesy of Prof Tomov.) |
 |
 |
| Figure 5. Caries were noted in the distal pit and fissures of the first molar. | Figure 6. The LiteTouch laser is utilized to remove the caries and prepare the tooth for restoration. |
 |
 |
| Figure 7. Preparation has been completed without the need for local anesthetic via conditioning of the enamel margins to improve bonding at the interface. | Figure 8. The composite restoration was completed, and polishing was finished. |
Enamel needs to be roughened to achieve ideal bonding when placing either a direct restoration or sealant. This can be performed by the traditional method of acid etching or by abrasion with air-driven particles or a diamond bur. The Er:YAG laser also may be used during preparation to condition the enamel margins to ensure a good bond at this interface. There has been no statistical significant difference reported between laser enamel conditioning and acid etching.13 The irradiation of enamel with an Er:YAG laser does not interfere with the performance of simplified 2-step etch-and-rinse and universal adhesive systems.14
Er:YAG lasers such as the LiteTouch (ids) (Figure 1), with a wavelength of 2,940 nm, has an affinity for hydroxyapatite and water (Figure 2). The laser is used in a noncontact mode when preparing tooth structure and desensitizes the odontoblastic fibers in the dentin, eliminating sensitivity normally reported via preparation with a bur. Laser tooth preparation is unique as there is no vibrating bur and no resulting micro-fracturing of the surrounding enamel. Additionally, the smear layer left by rotary burs on the treated dentin surface is removed as the laser ablates both dentin and enamel without leaving a carbonized surface behind15 (Figure 3). As self-etch adhesives require that the smear layer remains, removal with some of these adhesives may decrease bond strength. So, if lasers are utilized for caries removal, it is recommended that a dentin bonding agent containing MDP be used due to its property of increasing bonding strength to dentin.16 Treatment of the enamel margins with the LiteTouch laser yields a surface with an enhanced bonding surface (no need for acid etching). The Er:YAG laser removes the prismatic substance around the rods (Figure 4). Increased retention has been found when demineralized enamel was prepared with a laser, as compared to acid etching.17 Er:YAG lasers are effective for ablation of hard tissues, creating an irregular and microretentive morphological pattern without hard-tissue damage.18
 |
 |
| Figure 9. A radiograph, demonstrating interproximal caries and some residual old composite. | Figure 10. Clinical presentation of interproximal caries on the incisors. |
 |
 |
| Figure 11. Laser removal of the caries and affected old composite with the LiteTouch Er:YAG laser and enamel margin conditioning. | Figure 12. Completion of the interproximal composites into the laser tooth preparations. |
Other Uses of Lasers in Preventative and Restorative Dentistry
The use of an Er:YAG laser during sealant application has been reported to not provoke anxiety and is well accepted by children compared to the use of an acid-etching gel and the need to allow it to sit on the tooth and then be rinsed off.19 Prior to using sealants, the laser conditions the enamel for better bonding and to eliminate the less-than-pleasant-tasting etching gel.20 The laser eliminates bacteria within the pits and fissures, decreasing the potential for recurrent decay under the sealant. Laser enamel conditioning before sealant application appears to reduce sealant fracture and loss, possibly related to the micromorphological changes that the laser leaves on the enamel surface.21
The Er:YAG laser removes old composite restorations as effectively as it removes tooth structure.22 Although the laser is slower than a bur at the removal of composite resin in the tooth, it leaves a rougher surface for adhesion to place the new resin.23 Amalgam removal is better addressed by a handpiece and bur as the material does not ablate with the bur and is reflective in nature. The laser may then be utilized to cleanse the preparation surface, sterilizing the dentin and conditioning both the enamel and dentin for the adhesive restoration.
 |
 |
| Figure 13. Clinical presentation of defective cervical composite with associated root sensitivity. | Figure 14. A tooth following LiteTouch Er:YAG laser removal of the defective composite and desensitization of the exposed roots on the teeth in the quadrant. |
 |
| Figure 15. Placement of new composite into the laser-prepared tooth. |
Dentin hypersensitivity is frequently reported by patients, specifically on exposed roots, which can cause discomfort and even severe pain. A 2-minute Er:YAG laser application to exposed cervical root areas has been found to provide lasting desensitization of hypersensitive dentin, with no detrimental pulpal effects. Laser treatment has been shown to be efficacious and typically demonstrates relief at the first appointment.12
CASE REPORTS
Examples of Clinical Applications in Restorative Dentistry
Caries identified in pits and fissures are ideally treated with the laser (Figure 5). Conservative removal of caries can be performed without the need for local anesthetic (Figure 6). The enamel was conditioned during laser ablation of the caries and was ready for adhesive application (Figure 7). The direct composite was placed (Gradia Direct [GC America]), and then the restoration was finished and polished (Figure 8).
Interproximal caries can be effectively removed with the LiteTouch laser while maintaining conservative tooth removal without the need for local anesthetic administration. A radiograph demonstrated interproximal caries with close proximity to the tooth’s pulp (Figure 9). Clinically, although root exposure was present, the patient reported no history of sensitivity (Figure 10). The patient chose to only treat the caries and indicated aesthetics were not a concern in treatment of the discolored root exposures. Caries and residual composite were removed with the laser without pulpal exposure noted. The laser was used to condition the enamel margins to improve bonding of the restoration to be placed (Figure 11). Adhesive (Adhese Universal [Ivoclar Vivadent]) was placed and light-cured, followed by placement of the composite (Nuance Universal [DenMat]), and then the restorations were finished and polished (Figure 12).
Cervical sensitivity can result due to root exposure, caries, defective old restorations, or combinations thereof (Figure 13). The laser was utilized to remove any caries and old restorative material while conditioning the surrounding enamel margins in preparation for the new restoration (Figure 14). Prior to initiating the restoration placement, the LiteTouch laser was reset and used on any exposed root exposures in the quadrant to eliminate sensitivity that was reported by the patient prior to treatment. The prepared tooth was then restored with a bonded composite (Nuance Flow [DenMat]) and finished and polished (Figure 15).
CLOSING COMMENTS
Er:YAG lasers, such as the LiteTouch, have many clinical applications, including anesthetic-free caries removal and the conservative removal of old composite. In regard to pediatric patients, the experiences they are exposed to that have negative connections (local anesthetic injections and sounds and vibrations from the drill) will adversely impact their dental experiences for their lifetimes. However, with the laser, we can change those lifelong perceptions to create positive dental experiences that can last a lifetime by providing more comfortable experiences. Adults will often avoid dental treatment due to the perceived pain from local anesthetic injections and the sounds/sensations of dental drills. The laser eliminates local anesthetic use in many cases and removes the sound/sensation that causes many adults to tense up during treatment, making it a more pleasurable experience. This can also be a significant practice builder. As the laser provides selective ablation, it aids in preserving more natural tooth structure, which has been shown to increase the long-term prognosis of a tooth.
References
- Prathima GS, Bhadrashetty D, Babu SB, et al. Microdentistry with lasers. J Int Oral Health. 2015;7:134-137.
- Mosskull Hjertton P, Bågesund M. Er:YAG laser or high-speed bur for cavity preparation in adolescents. Acta Odontol Scand. 2013;71(3-4):610-615.
- Valério RA, Borsatto MC, Serra MC, et al. Caries removal in deciduous teeth using an Er:YAG laser: a randomized split-mouth clinical trial. Clin Oral Investig. 2016;20:65-73.
- Al-Batayneh OB, Seow WK, Walsh LJ. Assessment of Er:YAG laser for cavity preparation in primary and permanent teeth: a scanning electron microscopy and thermographic study. Pediatr Dent. 2014;36:90-94.
- Baraba A, Kqiku L, Gabri D, et al. Efficacy of removal of cariogenic bacteria and carious dentin by ablation using different modes of Er:YAG lasers. Braz J Med Biol Res. 2018;51:e6872.
- Zhegova G, Rashkova M, Rocca JP. Minimally invasive treatment of dental caries in primary teeth using an Er:YAG laser. Laser Ther. 2014;23:249-254.
- Rizcalla N, Bader C, Bortolotto T, et al. Improving the efficiency of an Er:YAG laser on enamel and dentin. Quintessence Int. 2012;43:153-160.
- Ceballos L, Toledano M, Osorio R, et al. ER-YAG laser pretreatment effect on in vitro secondary caries formation around composite restorations. Am J Dent. 2001;14:46-49.
- Folwaczny M, Aggstaller H, Mehl A, et al. Removal of bacterial endotoxin from root surface with Er:YAG laser. Am J Dent. 2003;16:3-5.
- Du Q, Ge L, Zhang S, et al. Effects of erbium:yttrium-aluminum-garnet laser irradiation on bovine dentin contaminated by cariogenic bacteria. Photobiomodul Photomed Laser Surg. 2019;37:305-311.
- Yu CH, Chang YC. Clinical efficacy of the Er:YAG laser treatment on hypersensitive dentin. J Formos Med Assoc. 2014;113:388-391.
- Sgolastra F, Petrucci A, Severino M, et al. Lasers for the treatment of dentin hypersensitivity: a meta-analysis. J Dent Res. 2013;92:492-499.
- Topaloglu-Ak A, Onçağ O, Gökçe B, et al. The effect of different enamel surface treatments on microleakage of fissure sealants. Acta Med Acad. 2013;42:223-228.
- De Jesus Tavarez RR, Rodrigues LL, Diniz AC, et al. Does erbium:yttrium-aluminum-garnet laser to enamel improve the performance of etch-and-rinse and universal adhesives? J Contemp Dent Pract. 2018;19:278-282.
- Lima DM, Tonetto MR, de Mendonça AA, et al. Human dental enamel and dentin structural effects after Er:YAG laser irradiation. J Contemp Dent Pract. 2014;15:283-287.
- Dönmez N, Güngör AS, Karabulut B, et al. Comparison of the micro-tensile bond strengths of four different universal adhesives to caries-affected dentin after ER:YAG laser irradiation. Dent Mater J. 2019;38:218-225.
- Guedes SF, Melo MA, Lima JP, et al. Acid etching concentration as a strategy to improve the adhesive performance on Er:YAG laser and bur-prepared demineralized enamel. Photomed Laser Surg. 2014;32:379-385.
- Freitas PM, Navarro RS, Barros JA, et al. The use of Er:YAG laser for cavity preparation: an SEM evaluation. Microsc Res Tech. 2007;70:803-808.
- Shindova MP, Belcheva AB, Mateva NG. Influence of Er:YAG laser on objective and subjective parameters of stress during sealant application in children. Folia Med (Plovdiv). 2018;60:275-282.
- Unal M, Hubbezoglu I, Zan R, et al. The effect of Er:YAG laser and different surface conditioning procedures on microtensile bond strength of the fissure sealant containing amorphous calcium phosphate after artificial aging. Dent Mater J. 2014;33:21-26.
- Maddalone M, Ferrari M, Barilla S, et al. Enamel laser conditioning before sealant application [in Russian]. Stomatologiia (Mosk). 2012;91:25-27.
- Yassaei S, Aghili H, Joshan N. Effects of removing adhesive from tooth surfaces by Er:YAG laser and a composite bur on enamel surface roughness and pulp chamber temperature. Dent Res J (Isfahan). 2015;12:254-259.
- Correa-Afonso AM, Pécora JD, Palma-Dibb RG. Influence of pulse repetition rate on temperature rise and working time during composite filling removal with the Er:YAG laser. Photomed Laser Surg. 2008;26:221-225.
Dr. Kurtzman is in private general practice in Silver Spring, Md, and is a former assistant clinical professor in the University of Maryland School of Dentistry’s Department of Endodontics, Prosthetics, and Operative Dentistry. He has lectured both nationally and internationally on the topics of restorative dentistry, endodontics, implant surgery and prosthetics, removable and fixed prosthetics, and periodontics and has published more than 650 articles. He is privileged to be on the editorial board of numerous dental publications, a consultant for multiple dental companies, and a former assistant program director for a university-based implant maxi-course. He has earned Fellowships in the AGD, the American Academy of Implant Prosthodontics, the American College of Dentists, the International Congress of Oral Implantologists (ICOI), the Pierre Fauchard Academy, and the Academy of Dentistry International. He also has earned Masterships in the AGD and ICOI and Diplomate status in the ICOI and the American Dental Implant Association. Dr. Kurtzman has been honored to be included in Dentistry Today’s “Leaders in Continuing Education” annually since 2006. He can be reached at dr_kurtzman@maryland-implants.com.
Disclosure: Dr. Kurtzman receives an honoraria from Lite Instruments for lectures.
Dr. Koceja graduated from the Marquette University School of Dentistry in 1986. He served 8 years in the United States Navy Dental Corp, where he completed a 1-year periodontal Fellowship and received the Navy Commendation medal for outstanding service. He received his laser proficiency certificate with the Academy of Laser Dentistry in 2001 and Mastership in the World Clinical Laser Institute in 2003. Dr. Koceja has been in private practice since 1994 and has actively incorporated lasers into his practice since 1999. His focus is to incorporate lasers into the “everyday practice” of dentistry and provide a less invasive, high-tech standard of care for his patients. He has lectured throughout the world on dental lasers, trained thousands of doctors and hygienists, and has been actively involved in laser product development and the testing of dental lasers for over 18 years. He can be reached at mkoceja@comcast.net.
Disclosure: Dr. Koceja reports no disclosures.
Related Articles
Management of Oral Viral Lesions With a Diode Laser
Know the Risks Before Adding Phlebotomy to Your Dental Practice
6-Part Series Explores the Evolution of Comprehensive Care











