 |
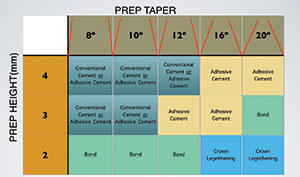
| Figure 1. A cement decision chart, advising which cement to use, depending on the height and taper of the prepared tooth. |
Indirect restorations have taken on an interesting and dynamic edge in recent years, resulting in a consumer-driven evolution of dental prosthetics. Patients demanded a more aesthetic restorative material with a metal-free substructure, and the market has delivered. But the introduction of new substrate materials, bonding agents, and cements has complicated the application of the indirect-restoration process. The aim of this article is to clarify the available luting and adhesive options and to provide insight into how one might best utilize those options.
Cementation or Adhesion: Which Is It?
While most clinicians use the terms “cementation” and “adhesion” interchangeably when referring to placing indirect restorations, the difference between these 2 approaches could not be more different. Cementation refers to the process in which a substance that hardens is used to bind 2 bodies together, purely on a mechanical basis. On the other hand, adhesion is defined as a force of attraction between unlike bodies that acts to hold them together chemically and mechanically. Bonding is the technique that adheres the bodies. This distinction is made only to clarify that adhesion is superior to cementation in terms of force of attraction between unlike bodies (eg, tooth and crown substrate).
For many years, metal was the only substrate available in the dental market, and only one cement type and one technique were required for the successful placement of crowns. With the introduction and wide acceptance of zirconia-based restorations (Lava [3M]) and lithium disilicate (IPS e.max [Ivoclar Vivadent]) in 2001 and 2005, respectively, different luting materials and techniques were required. Soon, it became apparent that, while dentists adopted both substrates, conventional cementation techniques were often inappropriately used during their placement. The chemical compositions of lithium disilicate and zirconia are so unlike metal and metal-based crowns that they necessitate the use of different adhesive steps and materials. For example, lithium disilicate and zirconia inherently possess high-energy and hydrophilic surfaces that are not conducive to adhesion. A priming step is needed to create a lower-energy, hydrophobic surface that can then reliably adhere to a cement.1 This is accomplished by coating the inside of the crown with its intended primer and allowing it to dry before final placement. Typically, lithium disilicate crowns are primed with silane, while zirconia crowns are treated with zirconia-specific primers (such as Z-PRIME Plus [BISCO Dental Products]) available from a variety of manufacturers. In recent years, a universal primer (Monobond Plus [Ivoclar Vivadent]) was introduced that can be used on metal, metal-based (PFM), and all-ceramic substrates, including leucite-reinforced porcelains (such as IPS Empress Esthetic [Ivoclar Vivadent]) and other high-strength ceramics, like lithium disilicate (such as IPS e.max or Initial LiSi Press [GC America]) and high-strength polycrystalline all-ceramics, such as zirconia.
Current adhesive protocol for an indirect all-porcelain restoration requires the tooth to be prepared, etched, and treated with a suitable adhesive. Regardless of the cement used, the substrate must be treated separately with its own primer, and a cement can then act to hold the tooth and substrate together. While this is a seemingly simple concept, final tooth resistance/retention form, multiple substrate options, and a variety of luting materials can obscure the process for even the most astute clinicians.
 |
 |
| Figure 2. A prepared short-nonretentive tooth. The crown was ready to be cemented using a total-etch technique with a dual-cure resin cement (Calibra Ceram [Dentsply Sirona]). | Figure 3. Uni-Etch W/BAC 32% Phosphoric Acid etch (BISCO Dental Products). |
 |
 |
| Figure 4. Bonding adhesive was applied (Prime & Bond [Dentsply Sirona]). | Figure 5. Primer was applied to the all-ceramic (BruxZir Zirconia [Glidewell Laboratories]) crown. |
 |
 |
| Figure 6. Placing Calibra Ceram in the crown. | Figure 7. The crown was seated on the tooth. |
Other Factors Important to Restorative Longevity
The clinician should also keep in mind that, when adhering modern crown substrates to tooth structure, the design and execution of tooth preparation is an equally important part of the restoration process. The long-term success of a restorative material depends as much upon attaining proper resistance and retention form in the preparation as on the luting cement used in the placement. The height and taper of the prepared tooth will govern how the cement resists oblique forces for the lifetime of the restoration.
Proper isolation of the operative field using a rubber dam or other appropriate isolation techniques (such as Isolite [Isolite Systems]) plays a key role in long-term restorative success because moisture compromises the physical properties of both adhesives and cements.
Choosing a Cement
After the tooth and substrate have been properly prepared, the final step in the process is to apply an appropriate cement to the restoration. The primary purpose of the cement is to fill the micro-gap between the tooth and substrate.2 The secondary role of a cement is to assist in retention of the restoration. From mechanically retentive luting cements to adhesive cements, which are both mechanically and chemically retentive, there are many selections available to clinicians today. This can understandably cause confusion regarding which cement will be best suited for a given clinical situation and how best to proceed once a decision has been made. The choice ultimately depends on the resistance and retention of the crown preparation (Figure 1), the clinical situation, and the operators’ preferences. It should be noted that despite the numerous options, no cement can compensate for poor tooth preparation.
Let’s now review some of the available luting options.
Glass Ionomer Cements
Glass ionomer cements (GICs) were first introduced to the dental market in the 1970s. Classified as conventional luting cements, GICs boast thin film thickness, moisture tolerance, and anticariogenic properties via their ability to release fluoride. They are self-curing and are indicated for metallic, PFM, and all-porcelain restorations, provided that both the retention and resistance forms of the tooth are suitable. Because GICs have been around so long, they are well understood and can be an exemplary and reliable cement choice if used properly.
Resin-Modified Glass Ionomer Luting Cements
Resin-modified glass ionomer (RMGI) luting cements made their market debut in the 1990s as a hybrid between GICs and resin cements (RCs). An RMGI retains many of the benefits of a GIC but features improved strength and handling due to its resin-reinforced matrix. RMGIs are insoluble in oral fluids and able to be light-cured. They are indicated for metal and metal-based (PFM) restorations, as well as lithium disilicate and zirconia restorations where moisture control is difficult. However, in practice, they are only recommended for retentive preparations because even the newer RMGIs cannot match the strength of a resin cement.
 |
 |
| Figure 8. Excess cement was cleaned after tack curing with the light-curing unit. | Figure 9. The prepared retentive tooth. The crown was ready for cementing with a self-etch, dual-cure resin cement (Calibra Universal [Dentsply Sirona]). |
 |
 |
| Figure 10. A primer (Z-PRIME Plus [BISCO Dental Products]) had been applied to the zirconia (BruxZir) crown. | Figure 11. The crown was filled with a self-adhesive resin cement (Calibra Universal). |
 |
 |
| Figure 12. The seated crown was tack cured using the light-curing unit for 3 seconds from the buccal direction and 3 seconds from the lingual direction. | Figure 13. Note the easy cleanup carried out at the margin after the tack curing. |
Resin Cements
Resin cements were commercially launched in the 1980s, but a torrent of advancements has broadened the category in recent years. Classified as adhesive cements, their versatility and high-bond strength make them among the best cement options available in today’s market. However, the clinician must be exacting in the utilization of an RC in a given clinical situation or else their effectiveness can be limited. RCs can be grouped into 3 general subtypes: self-cure, light-cure, and dual-cure formulations. Note that many RCs are touted as being “universal,” but this term is little more than an affectation. Each manufacturer prescribes its own meaning to the word “universal,” so it is always best to scrutinize the indications of any product before use.
Total-Etch Light-Cure RCs
Total-etch light-cure RCs require the clinician to independently etch, rinse, and apply a bonding agent to the tooth before proceeding with the cementation of the crown. They are available in a variety of shades and are generally sold as 2-part systems: one syringe contains the catalyst, and a second syringe contains the base. The base can be used independently and can only be cured by light when used in this fashion. When mixed together with the catalyst, the 2 will react to create a dual-cure material. This RC type should be used only when adequate light energy can be attained. The placement of anterior veneers is a typical clinical situation where the total-etch light-cure RC is used in conjunction with the more translucent glassy ceramics (such as lithium disilicate).
Total-Etch Dual-Cure RCs
Total-etch dual-cure RCs are administered from a dual-barrel syringe. With these systems, the base and catalyst components combine as they are expressed from the syringe. They are available in a range of shades and are made by many manufacturers. The total-etch dual-cure RC shown as an example in this article is Calibra Ceram (Dentsply Sirona) (Figures 2 to 8). These cements still require independent etching, rinsing, and adhesive steps on the tooth side because of their total-etch formulation. Total-etch dual-cure RC luting cements are excellent options when the crown is less than retentive and in areas of the mouth where light is restricted.
Self-Etch RCs
The most recent category of RCs is self-etching RCs (Figures 9 to 13). This type incorporates the etchant and bonding agent into the cement itself. This classification is sometimes referred to as self-adhesive RCs. A built-in adhesive primer that penetrates the smear layer of the tooth differentiates this cement from other RCs. They are dual-cured, and the excess material can be easily cleaned up after seating the crown, pending an initial 5- to 10-second tack cure at the margins. Self-etch RCs are viable candidates for all retentive and some non-retentive preparations and can be paired with lithium disilicate and zirconia all-ceramic materials.
Generally, the clinician should consider using a total-etch approach when (a) little dentin is present, (b) the tooth can be properly isolated to allow for a dry bonding field, and (c) the preparation is retentive or mostly retentive. A self-etch approach may be considered when (a) little enamel is present, and (b) the tooth preparation is mostly retentive. When dealing with cut enamel, a short 3- to 5-second phosphoric acid etching followed by a self-etch RC is ideal. It is important to remember that over-etching or under-etching may reduce the strength of the final bonded restoration, so a precise balance must be emphasized during etching in any bonding situation.3
Closing Comments
The last decade has yielded much advancement in the area of indirect restoration materials, giving way to the more efficient final delivery of lab-fabricated restorations with increased longevity. With so many beneficial cement options available in today’s market, it is prudent for clinicians to remain aware of the specifications of each crown preparation and recognize how that ultimately dictates the choice of cement. The retentive or nonretentive nature of the preparation and each individual clinical scenario are the determining factors that must guide the path forward. Gone are the days when a singular cement system could serve all indirect restoration applications. Wise clinicians will stock multiple cements in their practices and maintain clear decision trees regarding when to use a specific restorative material and how to tackle any clinical situation that presents.
References
- Kim BK, Bae HE, Shim JS, et al. The influence of ceramic surface treatments on the tensile bond strength of composite resin to all-ceramic coping materials. J Prosthet Dent. 2005;94:357-362.
- Infodentis. Dental cement. Permanent and temporary cementation. http://www.infodentis.com/
fixed-prosthodontics/dental-cement.php. Accessed January 17, 2018. - Alex G. Preparing porcelain surfaces for optimal bonding. Compend Contin Educ Dent. 2008;29:324-335.
Dr. Simos maintains private practices in Bolingbrook and Ottawa, Ill. He received his DDS degree from Chicago’s Loyola University and is the founder and president of the Allstar Smiles Learning Center and client facility in Bolingbrook, where he teaches postgraduate courses to practicing dentists on cosmetic dentistry, occlusion, and comprehensive restorative dentistry. He is an internationally recognized lecturer and leader in cosmetic and restorative dentistry. He can be reached via the website allstarsmiles.com, via the email address cmesmile50@gmail.com, or via the Twitter handle @allstarlc1.
Disclosure: Dr. Simos reports no disclosures.
Related Articles
Anterior Tooth Replacement Made Easy: A Conservative and Predictable Direct Technique
Three Impression Material Classifications: A Comparison











