INTRODUCTION
Stratified resin-modified glass ionomer/resin-based composite Class I and Class II permanent molar restorations have been described as adhesive, biomimetic tooth repairs.1,2 The concept is based on the idea that certain hydrophilic glass polyalkenoate (glass ionomer) systems are the best direct-application dentin replacement materials and hydrophobic resin-based composites are the best direct-application enamel replacements. When these materials are adhesively bonded to tooth structure and each other, a tooth repair that closely mimics biological form and function is achieved.
A dental restorative material called ACTIVA BioACTIVE-RESTORATIVE (Pulpdent) (hereafter referred to as ACTIVA in this article) is a proprietary formulation incorporating components of both glass ionomer systems and resin-based composites. After observations of 300 dental restorations, Croll, Berg, and Donly3 called this tooth-repair material “a resin-modified glass-ionomer bioactive ionic resin-based composite” and described methods for its use. With 12 examples, Croll and Lawson4 documented the diversity of the material after almost 4 years of use. Research regarding strength, wear resistance, adhesion dynamics, ion release, and other properties have supported 5 years of clinical observations in the senior author’s pediatric dentistry practice (3,761 tooth restorations from February 2014 to November 2019) concluding that ACTIVA functions well as a Class I and II dental restorative material for both primary and permanent teeth.5-14
 |
 |
| Figure 1. A 16-year-old with Class I and II caries lesions. | Figure 2. After local anesthesia and “split” rubber dam placement,15 mesial caries lesions were revealed. |
 |
 |
| Figure 3. The carious substance was debrided, and 2 occlusal preparations and mesio-occlusal preparations were completed. There was no evidence of distal surface caries lesions on the second premolar. | Figure 4. Preparations were disinfected with 2 glutaraldehyde/HEMA 60-second washes.16 |
 |
 |
| Figure 5. After TheraCal LC (BISCO Dental Products) resin containing calcium silicate/MTA liner was placed and light-hardened in regions of deep dentinal penetration,17,18 a custom-contoured, 0.0015-in (0.0381-mm) stainless steel matrix strip (Strip-T [DENOVO Dental]) was placed and stabilized with a wooden wedge. | Figure 6. Enamel surfaces peripheral to cavosurface margins were roughened with a slow-speed diamond bur. |
 |
 |
| Figure 7. Self-etching bonding agent (Prompt L-Pop [3M]) was applied and agitated for 20 to 30 seconds (standard phosphoric acid etch/rinse/dry and resin bonding agent can also be used for this bonding step). | Figure 8. The bonding agent was light cured. |
 |
 |
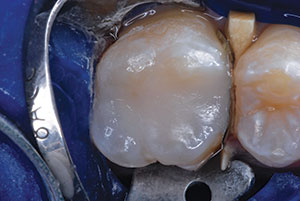
| Figure 9. ACTIVA BioACTIVE-RESTORATIVE (Pulpdent) was injected carefully to overfill, avoiding air incorporation, using an AccuDose Syringe (Centrix). (An ACTIVA SPENSER [Pulpdent] mixer/dispenser can also be used for this step). Two layers, each light-hardened separately, can be used in very deep preparations. | Figure 10. Uncured ACTIVA was spread and extended over roughened, etched, and coated cavosurface margins. |
This report serves as a step-by-step pictorial essay documenting Class I and II restorations of a maxillary permanent first molar and subsequent Class II repair of the adjacent premolar using this unique repair material in a teenager. We consider these restorations typical of ACTIVA tooth repair of permanent posterior teeth.
CASE REPORT
Figures 1 to 25 document Class I and II restorations of a maxillary first molar and subsequent repair of the adjacent second premolar using ACTIVA RESTORATIVE material. The initial caries lesions in the molar were diagnosed in November 2016. Twenty-six months later, with continued flossing neglect and regardless of efforts to educate and encourage routine flossing, the adjacent second premolar had also developed a disto-occlusal caries lesion. Repair of that tooth is also documented. The 2 repair procedures and followup in the 31-month time frame are shown and described.
DISCUSSION
We recommend that standard enamel-roughening, phosphoric acid etching (whether it be with a self-etching bonding agent or the etch/rinse/dry/apply method) be done when placing ACTIVA. However, when restoring primary teeth, the lead author does not use a bonding agent; the material is syringed into the tooth preparation, followed by a 20- to 30-second hiatus until the light beam is applied. Retention is gained by mechanical undercutting in preparation design. The acid component of the material might have some role in retention and also influences bonding. In permanent tooth ACTIVA repair, etching and bonding agents are always used, along with any mechanical undercutting that occurs in typical preparation design. The excess material that is peripherally spread over the enamel to the cavosurface margins serves as a marginal sealant in both primary and permanent tooth restorations. We recommend a calcium silicate/mineral trioxide aggregate liner in deeper regions of a preparation (Figures 5 and 22). The liner not only supplies calcium for pulpal healing but also virtually eliminates postoperative tooth sensitivity in our experience.17,18
 |
 |
| Figure 11. After 20 seconds of light application, the overfilled restoration was ready for finishing steps. Note that ACTIVA has a chemical resin polymerization reaction along with its light-curing feature, so deep hardening of the material is ensured. | Figure 12. A large round diamond bur was used to sculpt the occlusal surface. |
 |
 |
| Figure 13. Excess ACTIVA remains over the cavosurface margins, serving as marginal sealant. | Figure 14. The marginal ridge was sculpted with a Fissurotomy Bur (SS White Dental). |
 |
 |
| Figure 15. A finishing/polishing disc (Sof-Lex [3M]) was used to shape and smooth the marginal ridge. | Figure 16. A resin-based adhesive (Prompt L-Pop) was applied as finishing glaze. |
 |
 |
| Figure 17. The resin glaze was light cured for 10 seconds for full polymerization. | Figure 18. The occlusion was then evaluated, and adjustments made as needed. |
 |
 |
| Figure 19. August 2017, 7-months postoperatively. | Figure 20. In January 2018, the adjacent second premolar had developed a distal caries lesion. |
A recent research report showed how ACTIVA restorations can perform poorly when placed using minimal acid etching with no bonding agent, as compared to a resin-based composite placed with both acid etching and an adhesive bonding agent.21 For complete comparisons, we do not understand why that study did not include ACTIVA being placed with acid etching and a bonding agent and why the resin-based composite was placed with only acid etching (ie, no bonding agent). In addition, there was no glutaraldehyde/HEMA disinfection of the cavity preparations and no calcium-containing liner (such as TheraCal LC [BISCO Dental Products]) placed in deep regions of either the ACTIVA or the comparison resin-based composite restoration preparations. Predictably, when bonding procedures and usual restorative protocols are not accomplished ideally, any resin adhesive restorative system will be compromised. We agree strongly with the researchers’ last statement, “Further studies should be conducted using a bonding agent,”21 but would add “and a restructured clinical technique.” Some new laboratory research from Dr. Lawson (submitted as an abstract for the IADR in March 2020) suggests that ion release from ACTIVA has some protective effect on the surrounding tooth structure, even when an adhesive is used.
 |
 |
| Figure 21. The premolar required disto-occlusal ACTIVA repair in the same manner as the first molar. | Figure 22. TheraCal LC liner was placed and light cured in the deep area of the preparation. (This view gave an ideal opportunity to visualize the mesial aspect of the mesio-occlusal ACTIVA restoration of the first molar.) |
 |
 |
| Figure 23. Premolar repair was completed. | Figure 24. The restored first molar and the premolar are shown at 31-months and 16-months post-op, respectively. |
 |
| Figure 25. This bite-wing radiograph was recorded when Figure 24 was photographed. A beginning distal-surface caries lesion on the mandibular second premolar was treated with silver diamine fluoride (SDF) and inserted using a soft dental pick.19 Other posterior proximal surfaces were similarly treated with SDF as a preventive measure.20 |
IN SUMMARY
Although there has been no clinical study on this subject, we consider these 2 dental restorations typical of what is achieved when using ACTIVA BioACTIVE-RESTORATIVE for Class I and II restorations of permanent posterior teeth. Having characteristics of both resin-based composites and glass ionomers may allow ACTIVA to benefit from advantageous properties of both restorative systems. Continuing experiences will tell how stratified adhesively bonded posterior tooth repair1,2 compares with the durability and reliability of ACTIVA when facing the same clinical challenges in the long term.
References
- Croll TP, Cavanaugh RR. Posterior resin-based composite restorations: a second opinion. J Esthet Restor Dent. 2002;14:303-312.
- Croll TP, Cavanaugh RR. Tissue-specific, direct-application class II tooth repair: a case report. Compend Contin Educ Dent. 2009;30:608-614.
- Croll TP, Berg JH, Donly KJ. Dental repair material: a resin-modified glass-ionomer bioactive ionic resin-based composite. Compend Contin Educ Dent. 2015;36:60-65.
- Croll TP, Lawson NC. Activa bioactive restorative material in children and teens [white paper]. Inside Dentistry. 2018;14:1-8.
- Garcia-Godoy F, Morrow BR, Pameijer CH. Flexural strength and fatigue of new Activa RMGICs. J Dent Res. 2014;93(special issue A). Abstract 254.
- Girn VS, Chao W, Harsono M, et al. Comparison of mechanical properties of dental restorative material. J Dent Res. 2014;93(special issue A). Abstract 1163.
- Pameijer CH, Garcia-Godoy F, Morrow BR, et al. Flexural strength and flexural fatigue properties of resin-modified glass ionomers. J Clin Dent. 2015;26:23-27.
- Garcia-Godoy F, Morrow BR. Wear resistance of new Activa compared to other restorative materials. J Dent Res. 2015;94(special issue A). Abstract 3522.
- Bansal R, Burgess J, Lawson NC. Wear of an enhanced resin-modified glass-ionomer restorative material. Am J Dent. 2016;29:171-174.
- Chao W, Girn V, Harsono M, et al. Deflection at break of restorative materials. J Dent Res. 2015;94(special issue A). Abstract 2375.
- Daddona J, Pagni S, Kugel G. Compressive strength and deflection at break of four cements. J Dent Res. 2016;95(special issue A). Abstract 0658.
- Alrahlah A. Diametral tensile strength, flexural strength, and surface microhardness of bioactive bulk fill restorative. J Contemp Dent Pract. 2018;19:13-19.
- Roulet JF, Hussein H, Abdulhameed NF, et al. In vitro wear of two bioactive composites and a glass ionomer cement. DZZ International. 2019;1:24-30.
- Bhadra D, Shah NC, Rao AS, et al. A 1-year comparative evaluation of clinical performance of nanohybrid composite with Activa bioactive composite in class II carious lesion: a randomized control study. J Conserv Dent. 2019;22:92-96.
- Croll TP. Alternative methods for use of the rubber dam. Quintessence Int.1985;16:387-392.
- Christensen GJ. Disinfection of tooth preparations—why and how? Clinicians Report. 2009;2:1-2.
- Gandolfi MG, Siboni F, Taddei P, et al. Apatite-forming ability of TheraCal pulp-capping material. J Dent Res. 2011;90(special issue A). Abstract 2520.
- Gandolfi MG, Siboni F, Prati C. Chemical-physical properties of TheraCal, a novel light-curable MTA-like material for pulp capping. Int Endod J. 2012;45:571-579.
- Croll TP, Berg JH. Delivery methods of silver diamine fluoride to proximal tooth surfaces for attenuation and prevention of dental caries lesions. Compend Contin Educ Dent. Feb 2020. In press.
- Horst JA, Heima M. Prevention of dental caries by silver diamine fluoride.Compend Contin Educ Dent. 2019;40:158-164.
- van Dijken JWV, Pallesen U, Benetti A. A randomized controlled evaluation of posterior resin restorations of an altered resin modified glass-ionomer cement with claimed bioactivity. Dent Mater. 2019;35:335-343.
Dr. Croll received his degree from the Temple University School of Dentistry and completed pediatric dentistry specialty training at the University of Connecticut. He is in private practice, specializing in pediatric dentistry in Doylestown, Pa. He is an adjunct professor of pediatric dentistry at the University of Texas Health Science Center at San Antonio Dental School and a clinical professor of pediatric dentistry at the Case Western Reserve School of Dental Medicine. He can be reached via email at willipus@comcast.net.
Dr. Lawson received his DMD degree from the University of Alabama at Birmingham (UAB) School of Dentistry and his PhD in biomedical engineering from UAB. He is currently an assistant professor and division director of biomaterials at UAB. Dr. Lawson has published more than 150 articles, abstracts, book chapters, and periodicals related to dental materials. He can be reached via email at nlawson@uab.edu.
Disclosures: Dr. Croll receives royalties for sales of Strip T Matrices by virtue of a business agreement with DENOVO Dental. Dr. Lawson has received grants from Pulpdent for research involving their products. Neither author received compensation for this article.
Related Articles
Universal-Size Mouthguards: An Affordable Alternative for the Young Athlete
Long-Span Fixed Partial Denture Repair: A Conservative Modern Material Solution
Resin Restorations Provide Alternatives to Drilling and Filling











