From the days of Wells and Morton, the profession of dentistry has been at the forefront of healthcare in the development of pain control. Today, many of the outpatient anesthesia techniques employed by our colleagues in medicine for procedures ranging from colonoscopies to plastic surgery are actually techniques developed by dentists and oral surgeons for third molar surgery.
Yet, despite our efforts at controlling (and often totally alleviating) pain, much of the public still fears dental treatment. Dental fear, along with the fear of heights and the fear of public speaking, rank among the public’s most common fears. Statistics vary depending on the criteria and questions used, but a significant percentage of the American population describes dental appointments as an anxiety-producing experience. One does not practice dentistry for very long before being confronted by a patient saying, “Nothing personal Doc, but I’d really rather not be seeing you today.”
WHY THE DICHOTOMY?
Like much of healthcare, dentistry approaches the control of pain and the control of anxiety as synonymous. “Big” procedures requiring big pain control, such as impacted third molar removal, are viewed as “deserving” big control of anxiety (ie, general anesthesia). Conversely, minor procedures requiring only a local anesthetic for pain control are viewed as “unworthy” of receiving apprehension management.
In reality, psychology has long established that pain and fear are not proportionately linked.
BASIC PRINCIPLES
 |
 |
|
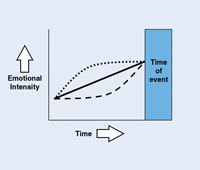
Figure 1. Emotions increase as event approaches. |
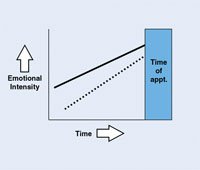
Figure 2. Successful approach/avoidance conflict. |
 |
|
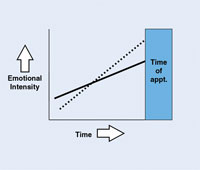
Figure 3. Distressed approach/avoidance conflict. |
Two basic psychological principles strongly influence dental patients’ behavior.
The first is that emotion intensifies as the time of an event approaches (Figure 1, solid line). Regardless of whether one is contemplating a positive or a negative experience, such as a vacation or a surgery, the emotion that is evoked from thinking about the event increases as the time of the event draws near.
It is noteworthy that not all individuals intensify their emotions linearly. Some patients experience strong emotional feelings about their upcoming dental appointments long before the actual time of the appointments (Figure 1, dotted line), and escalate even higher at the end. These individuals may dwell on their dental appointment for days or even weeks before the actual time they are to be seen by the dentist. Their emotional journey begins even before they call to schedule the initial appointment, as they work up the courage to phone the office.
Alternatively, other individuals are able to postpone their feelings about dental care (Figure 1, dashes) until they reach some arbitrary trigger (eg, driving to the office, entering the operatory, having the patient bib placed).
The second principle of human behavior is called the approach/avoidance conflict. Take a young boy joining organized baseball for the first time. He eagerly desires to play with his friends, be part of a team, hit a home run, and win the league championship. At the very same time, he dreads being hit by a pitch, dropping an easy pop-up, being embarrassed in front of his teammates, and finishing in last place. If potential benefits (approach) outweigh the risks (avoidance), he will endure spring training, develop better playing skills, and be a better athlete. However, if avoidance prevails, he will quit the team.
Dental patients behave exactly the same way (Figure 2). They desire to approach dentistry (solid line) because they perceive a positive benefit: relief of pain, improved health, enhanced aesthetics. Concurrently, they desire to avoid dentistry (dotted line) for a variety of reasons to be discussed later.
The key to managing a patient’s apprehension is simple. The dental team needs to keep the solid line consistently above the dotted line. If the 2 lines cross even briefly (Figure 3), appointments are cancelled, treatment plans are rejected, patients fail to appear for their appointments, or patients literally walk/run out of the office.
In order to avoid the situation in Figure 3, practice management experts have traditionally focused on elevating the solid line to keep consistently above the dotted line. They search for patient motivators and seek to satisfy them in order for the patient to have a stronger approach to dentistry than a desire to avoid it. While this approach works, it is limited. A patient’s positive emotions can only be elevated so far. Therefore, an equally important component in helping patients pursue treatment is to help them reduce the dotted line.
As part of verbally taking a traditional dental history, I explore a patient’s reservations about pursuing dental care. To help understand their barriers to treatment, it is important to know the answers to 3 questions:
• Why is the patient fearful of dentistry?
• How intense is the fear?
• What type of personality is this patient?
The answers to these 3 questions (avoidance), coupled with understanding the patient’s goals (approach) and an accurate diagnosis (comprehensive exam), will result in a treatment plan that best meets the needs and desires of the patient.
FOUR TYPES OF DENTAL FEAR
Given the frequency of dental fear in the population and the adverse effects on both patients and dentists, it is surprising that more research is not being done in this area of dentistry. However, some insights have emerged from the Dental Fear Clinic at the University of Washington by Milgrom, Weinstein, and Getz.1 They have categorized dental fear into 4 groups. Although these groups are not formal psychological or psychiatric classifications, they are a convenient system for dentists in clinical practice.
- Specific Fear. These individuals have one or 2 specific issues that bother them. Sometimes the problem is physical or procedural. Examples include fears of needles, forceps, rubber dams, root canals, extractions, and root planings. In other instances the specific fear is abstract. Separation anxiety (children) and fear of being criticized for negligence (adults) are examples of abstract fear.
Once identified, patients with specific fears are often the easiest to treat. Progressive desensitization works well if the fear is a repeatable procedure (eg, fear of scaling). In other instances, medications offer a better alternative. - Loss of Control. Milgrom, et al1 categorize these individuals as “distrustful patients.” I believe, however, this description is far too confining and begs the question, “Why are they distrustful?”
Some individuals have an innate need to always control a situation. Others, sexual abuse victims for example, have experienced significant events that have taught them it is in their best interest to preserve a sense of control. Recently, during her initial interview, a new 30-something patient used the words “smothering,” “trapped,” and “claustrophobic” in her description of past dental appointments. Upon further questioning, it was learned that as a young teen she had been trapped in an overturned automobile that fell into a shallow river. She had been suspended upside down by her seatbelt with her head inches above the water until rescue personnel arrived. She never realized that it was about the same time she began to fear being in a reclined dental chair with dental team members hovering with instruments around her mouth and nose for an arbitrary period of time.
Loss of control patients rarely do well with minimal sedation such as nitrous oxide, as this merely elevates their anxiety. When cognitive approaches fail, stronger levels of sedation are required. - Catastrophe. A relatively small percentage of dental fear patients do not actually fear dentistry. Rather, they fear the consequence of dental care. These individuals fear that some catastrophic event will occur at or as a result of their dental appointment. In some instances the fear may be rational. An older patient who takes a morning diuretic and also has bladder control problems may fear that a long, late morning appointment could develop into an accident. Far more frequently, however, the patient’s catastrophic-fear concerns are irrational. A case in point would be the patient who has previously experienced a transient tachycarida due to a response from an anesthetic vasoconstrictor. Now the patient fears that administration will lead to a fatal heart attack and that the dentist would be incompetent to address the problem.
A hallmark of these individuals is that they feel their bodies are out of control. A cognitive approach can be helpful when this problem is present. However, identifying these patients is a major challenge. Many of these people, who sense their fear is irrationally based, are hesitant to reveal their feelings and discuss them openly. - General Anxiety Disorder (GAD). According to Milgrom, et al1 this is the most common underlying cause of dental fear. Unlike the other groups, GAD is a recognized medical disorder. Simply stated, these individuals have difficulty coping with the stress of everyday life. These patients do not have an issue with dentistry per se. Rather, a dental appointment is nothing more than one more problem in a day already crowded with problems. Although they are different conditions, on some occasions these individuals may be clinically depressed as well as anxious. This is reasonable to expect because many of these patients are frustrated that they cannot cope with the strains of life as efficiently as everyone else appears to do.
To tolerate the stress of dental care, minimal to moderate sedation may be required because there is little the dentist can do to address the underlying cause. Consideration should be given to a medical referral to help the patient with their fundamental problem.
INTENSITY
Sadly, one important consideration that has not been thoroughly examined academically involves the intensity of a patient’s fear. Two patients might be fearful of injections, but if one is mildly anxious and the other is truly phobic, the clinical approach should be different. Although there are a limited number of written self-assessment tests that include fear intensity, they were developed for academic settings. I have found these are considered too intrusive by patients for use in a private office setting.
One simple yet surprisingly effective technique to assess the intensity of dental fear is to simply ask the patient. I ask the patient to describe the intensity of their fear on a scale of 1 to 5, with 5 representing “sheer terror.” I do not offer zero as a possible answer, nor do I define what number “1” means.
During the balance of the patient’s appointment my staff and I determine whether the patient’s behavior is consistent with their self-assessment. Although some patients clearly behave differently from their self-assessment, most patients are remarkably accurate and open about their fear issues.
UNDERLYING PERSONALITY
Despite similarities in the cause and intensity of their dental fear, seemingly comparable patients will behave differently. A simple yet highly effective technique to understand an individual’s personality is called DISC profiling (a trademarked term). Although a detailed description of this system is beyond the scope of this article, the premise revolves around assessing a person’s disposition toward being logical versus intuitive, and introversion versus extroversion. For further insights, please visit the Web site at discprofile.com.
SUMMARY
Collecting the answer to the 3 basic questions discussed above is both an art and a science that takes practice on the part of the doctor. Yet, by doing so, a treatment plan can be tailored that not only addresses the patient’s motivators, but also considers their barriers to treatment.
Patients who present with dental fear need not be viewed as challenging or difficult. Instead, they often represent the ideal patient (only in disguise). They often need extensive dental care. They are loyal, staying with a dentist despite changes in dental insurance coverage or moving away from the office. They are proud of their success and are genuinely most outgoing in serving as referrals. And finally, they are deserving of the very best care we have to offer.
Reference
- Milgrom P, Weinstein P, Getz T. Treating Fearful Dental Patients: A Patient Management Handbook. 2nd ed. Seattle, WA: University of Washington, Continuing Dental Education; 1995.
Suggested Reading
Egan G. The Skilled Helper. A Problem-Management And Opportunity-Development Approach To Helping. 7th ed. Pacific Grove, CA: Brooks/Cole (an imprint of the Wadsworth Group, a division of Thomson Learning); 2002.
Dr. Sangrik is a 1979 graduate of The Ohio State University College of Dentistry. He is a nationally known lecturer on the topics of dental fear, medical emergencies, vital signs, and sedation techniques in dentistry. He maintains a full-time general dental practice in Chardon, Ohio, with an emphasis on the treatment of apprehensive patients with IV sedation. He can be reached at (440) 286-7138.