INTRODUCTION
Either you see it, or you don’t! Some people never see it, while others see it immediately. It will drive you absolutely crazy if what you see does not match your aesthetic vision. Over the past several decades, we have witnessed a revolution in the fields of facial and dental aesthetics. A dentist’s key to success is to have a totally clear vision of the desired final result. A sequential treatment plan can then be made to predictably satisfy the patient.
If you watch television, you have undoubtedly seen commercials for orthodontic aligners delivered directly to your home for 60% less than the fees of a conventional orthodontist. The patients in the infomercials all express their total delight without any reservations. In my opinion, these advertisements imply superior high-tech treatment and quality equal to or beyond the capabilities of the average dentist. Everything seems so simple—but is it? In Greek mythology, Procrustes was a villain who either cut the legs off of or stretched his victims so that they would fit exactly into his iron bed. Everyone had to conform to be exactly one size. Procrustean treatment planning places everyone in the identical situation. There is no account for individual differences. Human beings, however, come in different sizes, shapes, and colors and have different personalities.
Having practiced and taught dentistry for more than 40 years, I am constantly asked if I have a set formula for treatment planning. Many educators have attempted to break down treatment planning into rules, steps, and sequences for the sake of teaching. Their aim is to provide their students with repeatable steps. Looking back in time, early orthodontic pioneers based their treatment objectives solely on art and aesthetics. Norman Kingsley (1829-1939) was an artist, sculptor, and orthodontist who published the first orthodontic paper (1853) and textbook (1880). He based his entire diagnosis and treatment objectives on facial proportions and his vision of beauty. When Edward Angle established the first orthodontic school, he set out to find a formula for beauty that could be repeatedly taught. He hired an artist, Edmund Wuerlpel, to help him. However, together, they failed to find a formula for beauty. Instead, they settled on the Angle Class 1/2/3 classification, which is still in use today based on its ability to be repeatable and taught to students. Angle needed set rules in order to be able to teach. However, his classifications are based on static factors, such as molar relationships, and do not always produce aesthetically pleasing results. Orthodontic diagnosis changed from evaluating facial aesthetics to relying on absolute measurements. Visual examination was superseded by information from a cephalometric radiograph and plaster study models. These do not consider patients’ facial features and soft tissue and how they will change over the patients’ lifetimes.
Aesthetic Vision
In my own practice, I have always based my treatment planning on the premise that “people want to look like people,” keeping in mind the ideal vision of the skeletal, soft-tissue, and muscular anatomy of the head and face. I never lose sight of the ideal tooth position, as seen in the typodont study model that I was given in my first year of dental school. This is my initial vision and the goal of my treatment planning. Dr. Irwin Smigel, a pioneer in the arena of aesthetic dental procedures, used to say, “Who owns the face? We do!” Dentists are capable of creating spectacular facial changes! We always begin with a visual assessment of the patient’s face and features. What is the face shape, width, and chin position? How much tooth is displayed at rest and when smiling? The relationship of the smile to the eyes, nose, and facial musculature must be considered. There is not a procrustean method of treatment planning where one size fits all. In aesthetics, there is a great deal of human variation, and a dentist’s experience, artistic ability, and ability to see with aesthetic vision are essential.
The Importance of Orthodontics in Restorative Dentistry
Historically, orthodontists were not accustomed to dealing with patients requiring restorations. A patient with ideally shaped teeth may fit into the “procrustean bed.” However, some patients do not conform to the ideal and require tooth positioning in order to accommodate a change in tooth size. The orthodontic objectives are different for these patients compared to the patient not requiring restorative changes. The teeth may have to be positioned by the orthodontist to accommodate a change in tooth shape, and sometimes we may choose to restore or place a provisional before starting orthodontics. The orthodontist is often the one making a decision that can affect a patient’s appearance for the rest of his or her life. By solely basing an orthodontic treatment plan on the Angle classification, we run the risk of poor facial results and unhappy patients. Orthodontic therapy should establish a functional occlusion, enhance the heath of the periodontium, and improve dental-facial aesthetics. We must approach each patient from an artistic perspective and do facial analysis using dentofacial proportions not solely based on a cephalometric film. We must consider the vertical placement of the anterior teeth at rest and when smiling, the smile arc characteristics, and the vertical relationship of the gingival margins to each other. Above all, we must consider the effect of aging of the patient’s facial features. Time is the “dental twilight zone.”
In order to establish a comprehensive treatment plan, it is essential for the dental team to be able to visualize the final result before commencing any treatment. Meticulous planning is essential. It is paramount for the dental health professional to not limit his or her vision to his or her own specialty. With a coordinated treatment plan and a multidisciplinary team approach, we can achieve predictable and pleasing results that will satisfy our patients for a lifetime.
The face should dictate the treatment. Every case begins with an aesthetic analysis of the facial shape and soft tissue. We must then reference the maxillary anterior tooth position and gingival levels relative to the face and determine if the upper anterior teeth are in an ideal position or if their position must be altered. We cannot establish the occlusal pattern until we determine our final vision of the maxillary anterior teeth. Aesthetics will dictate the final position of the entire dentition and the pathways of guidance.
CASE REPORT
Diagnosis and Treatment Planning
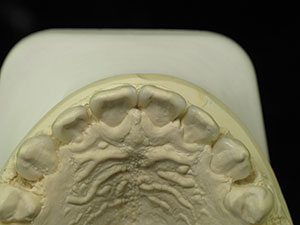
The parents of the 14-year-old boy presented in this case report article believed that he required orthodontics to close the gaps between his front teeth (Figure 1). Beginning with a visual examination, we felt that he had a handsome, oval-shaped face in pleasing proportion with his eyes, lips, and chin. His dental arch displayed full buccal corridors, and the posterior teeth were in occlusion. Upon comparing the patient’s dental models with the ideal typodont, we concluded that the spaces existed between his teeth because the teeth were too narrow and not in proportion with the arch width (Figure 2). To eliminate the spacing, either the arches would have to be constricted to pull the teeth together or the teeth would have to be made larger to fit the existing form.
 |
 |
| Figure 1. Upper anterior teeth, showing spacing. | Figure 2. Occlusal view of the upper dental arch. |
 |
 |
| Figure 3. The 11.0-mm central incisors created by laser gingivectomy. |
 |
 |
| Figure 4. The 9.5-mm lateral incisors and 11.0-mm canines, created by laser gingivectomy. |
We discussed the boy’s current aesthetics and, in addition, the future effect of what may happen to his facial features and aesthetics over time. The patient and his parents did not want to risk changing his appearance and chose to restore his teeth to the proportion necessary to close the spaces maintaining the existing arch form. If they would have chosen to bring the existing narrow teeth together and constrict the arches, occlusal and airway problems could result for his lifetime. These issues would be challenging to resolve. By explaining the problem and presenting the facts and all the possible solutions, a patient can then make an informed decision in his or her best interest.
There are different approaches to this situation. Some orthodontists prefer to finish the orthodontics and then have the teeth restored. If meticulously measured, the case can be done in this manner. In our experience, however, we do not like to leave anything up to chance, so we restore the tooth proportion first and then proceed with the orthodontic alignment. In my experience, closing the interdental spaces with composite bonding is a challenging task requiring 2 adjacent interproximal restorations with ideal dimensions in order for each space to be closed properly. This can consume a great deal of time, patience, and skill, even for a very talented dentist. In order to restore the gaps simply and predictably, we elected to use lab-fabricated micro-veneer additions. These would be conventionally bonded to the interproximal surfaces without any tooth preparations. Since they are composed of composite resin, we would be able to adjust, repair, and polish them.
Clinical Protocol
Each smile design begins by assessing the size of the maxillary central incisors. Ideally, they should respect the golden proportions with a 70% to 75% width-to-length ratio. As the centrals to be widened were 10.0 mm long, we calculated that an 11.0-mm central was necessary to respect the proportion with the additions. Visually, our patient’s teeth were long enough incisally; therefore, we chose to elongate the teeth gingivally by 1.0 mm using a diode soft-tissue laser, without infringing upon the biologic width of the attached gingiva (Figure 3). The lateral incisors were given a new length of 9.5 mm, and the canines were 11.0 mm, which was in proportion with the central incisors (Figure 4). The interproximal tissue was troughed with the laser (Gemini 810+980 diode laser [Ultradent Products]) allowing us to establish a natural emergence profile. We wanted the composite micro-veneer additions to follow the interproximal tooth surface so that overhanging food traps were not created.
 |
 |
| Figure 5. Retraction paste (Expasyl [Kerr]) shown in place. | Figure 6. Interproximal emergence profile. |
 |
 |
| Figure 7. An intraoral scan (TRIOS [3Shape]) was taken. | Figure 8. Final VPS impression (Honigum Pro-Putty and light-body Honigum wash impression materials [DMG]). |
 |
 |
| Figure 9. An accurate acrylic bite registration (LuxaBite [DMG]) was taken. | Figure 10. Mounted stone models. |
 |
 |
| Figure 11. Wax-up of the restorations. | Figure 12. Individually boxed composite micro-veneer additions. |
A gingival retraction paste (Expasyl [Kerr]) was placed for 2 minutes (Figure 5) and then thoroughly rinsed with water (Figure 6), providing clean exposed prep margins. A TRIOS (3Shape) digital scan (Figure 7) registered the impression, bite registration, and shade. While the latest digital technology certainly has its advantages, it is not essential to have a digital intraoral scanner, as identical results can be achieved with conventional impressions and bite registrations. When using a physical impression technique, I prefer to use a quality vinyl polysiloxane (VPS) (such as Honigum Pro Putty [DMG]) to take putty-wash impressions with Rim-Lock trays (Dentsply Sirona). Honigum Pro-Putty is used because it is extremely firm and displaces a light body wash impression material (Honigum) subgingivally into the sulcus, yielding a highly detailed and accurate impression (Figure 8). Subgingival detail is critical, as the microadditions must have ultrafine margins. The rigid metal Rim-Lock trays do not distort upon placing, removing, and pouring the impression. The lower opposing model was taken with a polyvinyl siloxane alginate substitute (StatusBlue [DMG]). The bite registration was taken using an acrylic material (LuxaBite [DMG]), which does not flex, allowing for extremely accurate mounting of the models, which will decrease the number of adjustments and remakes. LuxaBite should be applied sparingly to just the incisal and occlusal surfaces of the teeth so as not to engage in any undercuts (Figure 9).
 |
 |
| Figure 13. Etching (Uni-Etch [BISCO Dental Products]) and bonding (All-Bond Universal [BISCO Dental Products]) were done per the manufacturer’s directions. |
 |
 |
| Figure 14. Individual placement of the micro-veneers. |
Dental Lab Protocol
At the dental laboratory, stone models sealed with Tanaka Stone Surface Sealer (Tanaka Dental Products) were mounted on an Artex Articulator (Jensen) (Figure 10). Iso-Stift Separator (Renfert USA) was applied to prevent the new composite micro-veneer restorations from adhering to the model. A diagnostic wax-up from canine to canine was created on a duplicate model, providing a guide for the proportions of the composite restorations (Figure 11). GRADIA composite (GC America) micro-veneer additions were created by applying incremental layers (shade B1), each light cured for 10 seconds (Steplight SL1 [GC America]). Gradia Air Barrier (GC America) was then applied, and final curing was done with a Labolight LV4 (GC America). Diamonds, carbides, rubber wheels, and points were used to adjust the contours. A diamond polishing paste (Legabril Diamond Polish [Cendres & Metamucil]) then imparted a final high-luster polish. Then the inner surfaces of the restorations were cleaned and sandblasted to prepare them for bonding. Each composite restoration was individually packaged for identification and returned to the dental office (Figure 12).
Delivery of the Lab-Fabricated Micro-Veneer Restorations
The installation of the composite micro-veneer additions required an exacting protocol. First, the teeth were acid-etched (Uni-Etch [BISCO Dental Products]) for 15 seconds and then thoroughly rinsed with water. A universal adhesive (All-Bond Universal [BISCO Dental Products]) was applied (exactly per the manufacturer’s instructions) (Figure 13). A thin coating of a flowable micro-filled composite resin (Renamel Flowable Microfill [Cosmedent]) was applied to the internal surface of the composite micro-veneers, and then they were individually placed to each interproximal tooth surface and light cured (Figure 14). Polishing carbides, strips, and the use of the Top Finisher System (Cosmedent) (Figure 15) finalized the restorations.
 |
 |
| Figure 15. Creation of a new tooth dimension. | Figure 16. The iTero (Align Technology) orthodontic scan. |
 |
 |
| Figures 17 and 18. Insignia custom brackets (Ormco) and wire. |
Orthodontic Phase Begins
A new dimension in our patient’s maxillary incisors had now been established, and the orthodontist can now view them as the natural teeth. An iTero (Align Technology) scan was taken (Figure 16), and Insignia orthodontic software (Ormco) was used to determine the orthodontic movements that would be required. Insignia personalized brackets with built-in custom torque (Ormco) were created. The arch wires were prefabricated with first- and second-order bends that were designed specifically for this case (Figures 17 and 18).
CLOSING COMMENTS
Predictability is the key to success for a successful dental practice. The ability to see with aesthetic vision, meticulously plan, and know which treatment modality to use will often allow a simple solution for complex challenges. Either you see it, or you don’t!
Acknowledgments:
The author would like to thank Dr. Brita Nadeau, orthodontist, for being a key player in our interdisciplinary team and for her continuous inspiration. He also wishes to express his sincere appreciation to Chuck Maragos and the entire dental laboratory team at Valley Dental Arts (Stillwater, Minn) for their excellent work.
Dr. Mechanic has been practicing multi-disciplinary restorative aesthetic dentistry in Montreal since 1979. He received his Bachelor of Science (1975) and Doctor of Dental Surgery (1979) degrees from McGill University. He is a Diplomate of the American Board of Aesthetic Dentistry and a Fellow of the European Society of Cosmetic Dentistry and the International Academy of Dental Facial Aesthetics. He is the author of more than 40 dental publications and the book Aesthetic Dentistry/Smile Design: The Patient Guide, which has been published in 9 languages. He can be reached via email at elliotmechanic@gmail.com.
Disclosure: Dr. Mechanic reports no disclosures.
Related Articles
Treatment of Severe Oligodontia in Identical Twins
Interdisciplinary Treatment Planning: What Would You Do If She Were Your Daughter?
The Interdisciplinary Treatment Planning: The Restorative Quarterback











