INTRODUCTION
Young patients with complex developmental problems that impact the skeletal and dental systems require well-coordinated interdisciplinary management to restore functional, aesthetic, and psychological deficits. The following case report describes the management of a young female with hypohidrotic ectodermal dysplasia (HED) (also known as “anhidrotic ectodermal dysplasia” and “Christ-Siemens-Touraine syndrome”) by an interdisciplinary team comprising prosthodontists, an orthodontist, 2 oral-maxillofacial surgeons, and a team of dental technologists. In addition, this patient’s unique dental needs were well suited for use of a newly available restorative material in the course of her treatment. One of the many advantages of coordinated interdisciplinary treatment is the ability to sequence treatment to achieve short-term and long-term goals that help enhance the patient’s quality of life in logical, sequential steps.1,2
Teeth in proper alignment and interarch relationship are required for phonetics, mastication, deglutition, and sound nutritional support, as well as psychological well-being.3 Yet the medical condition of ectodermal dysplasia has significant dental complications: primarily oligodontia or anodontia and hypoplastic teeth.4,5 The featured patient exhibited all these manifestations, which impacted her ability to chew, speak, and function normally.
The diverse group of hereditary disorders that constitute ectodermal dysplasia mainly affect ectodermal structures such as hair, skin, nails, and teeth.3,4 Patients usually present with onychodysplasia (nail dystrophy), hypotrichosis or alopecia (scant or lacking hair), hypohidrosis (lack of sweat glands), and oligodontia or anodontia involving the primary and/or permanent dentition. This patient reflected her HED as predominately craniofacial malformations and had not developed some of the other systemic signs of HED. HED is thought to be an X-linked inheritance affecting males more severely and only partially in heterozygous female carriers with an incidence of 1:10,000 to 1:100,000 births, which coincides with the findings in this young female patient. Implant-supported crowns are a common treatment modality to replace congenitally missing teeth in the ectodermal dysplasia patient and will be utilized in this case after the skeletal defect and teeth malalignment are corrected.6-9 This article will focus solely on the patient’s phase I treatment to prepare her for the orthodontic and surgical phases that are to follow.
CASE REPORT
Clinical Examination Findings
An 18-year-old woman was referred to our practice from her oral-maxillofacial surgeon (Dr. Michael Gunson, Santa Barbara, Calif) for a prosthodontic evaluation prior to complex orthognathic surgery. She presented with a form of HED that involved oligodontia of 15 teeth. The patient had only 2 areas of occlusal contact for mastication; anteriorly, teeth Nos. 8 and 9 occluded with teeth Nos. 24 to 26, and, posteriorly, teeth Nos. 14 and 15 occluded with teeth Nos. 18 and 19. The deciduous molars were ankylosed/partially resorbed, and the remaining deciduous teeth had severe wear and were not viable for the long term. The oral maxillofacial surgeon (Dr. Gunson) and treating orthodontist (Dr. Todd Walkow, Newport Beach, Calif) requested the deciduous teeth be extracted prior to the commencement of orthodontic alignment to allow consolidation of the spacing for future prosthodontic rehabilitation. Aesthetic and functional improvements could be achieved on an interim basis utilizing the limited deciduous and permanent teeth that were present (Figure 1).
 |
| Figure 1a. Pretreatment photo showing the effects of hypohidrotic ectodermal dysplasia-related dental compromises. She presented with an unaesthetically pleasing smile due to numerous missing maxillary anterior teeth. |
 |
 |
| Figure 1b. Pretreatment photo demonstrating a complete lack of posterior occlusion on the patient’s right side. | Figure 1c. Pretreatment photo demonstrating some posterior occlusion with permanent molars on the patient’s left side. |
The lateral cephalometric radiograph revealed that the patient exhibited a concave facial profile with a maxillary anterior-posterior hypoplasia, a moderate asymmetric skeletal and dental Class III occlusion, an occlusal cant, a midline discrepancy in both jaws, and a severe posterior lateral open bite of 6.0 mm on the right side. These issues would be addressed in later phases of her interdisciplinary treatment.
The patient’s oligodontia involved 15 permanent teeth: Nos. 1, 4 to 7, 10 to 13, 16, 17, 20, 28, 29, and 31. The deciduous teeth that were present at her initial presentation were A to D, G to J, M, R, and T. Her periodontal health was good, but she had high biofilm levels and required focused oral health instruction to improve her cleaning habits to better prepare her for the many years of treatment that were ahead.
Treatment Planning and Sequencing
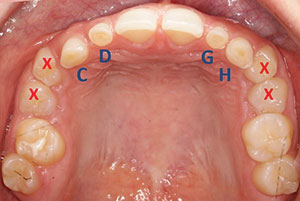
Phase 1 treatment objectives were to provide the patient with improved occlusal stability, extract non-functional deciduous teeth, and prepare her dentition for orthodontic treatment. By maintaining the 4 deciduous teeth C, D, G, and H, it was possible to maintain an anterior centric stop, aid in mastication, provide anchorage for orthodontic treatment, and establish a natural, aesthetic appearance. The maxillary deciduous teeth were restored to ideal permanent tooth contours to assist the orthodontist in establishing the correct spacing of the remaining dentition. The deciduous teeth A, B, I, J, M, R, and T were also extracted in phase 1 to allow the alveolar ridge to be grafted for future implant surgery (Figures 2 and 3).
 |
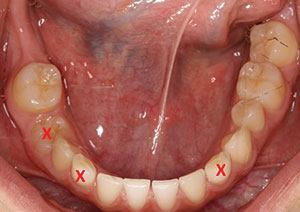 |
| Figure 2. Teeth marked with an X depict deciduous teeth to be extracted in the maxillary arch. Deciduous teeth C, D, G, and H were to be prepared for provisional crowns to establish appropriate tooth dimensions. | Figure 3. Teeth marked with an X denote deciduous teeth to be extracted in the mandibular arch. |
 |
 |
| Figure 4. Pre- (a) and post-diagnostic (b) wax-up study models. The establishment of appropriate tooth dimensions serves to guide orthodontic treatment objectives. |
A long-term, composite-based provisional crown material (LuxaCrown [DMG America]) was selected to build up the fragile, remaining deciduous anterior teeth (C, D, G, and H) to ideal dimensions for presurgical orthodontic anchorage and provide guidance for the orthodontist to align the permanent teeth (Nos. 2, 3, 14, 15, 18, 19, 21, and 30). LuxaCrown was chosen because it would provide the required color stability, polishability, durability, and strength that would be required during the orthodontic and surgical phases of her care. Those 4 teeth (C, D, G, and H) needed to be stable for the long term without significant maintenance, as they would be critical to many aspects of her future care. Additionally, the anterior restorations would provide her with more self-confidence in social interactions, as she was entering college the following year; it would be the first time the patient would have a more “normal” smile.
The planning phase included interdisciplinary consultations; the creation of a diagnostic wax-up; and treatment coordination between the patient, her parents, and the multiple specialists’ offices. This preliminary phase was also utilized to train the patient in the technique of careful biofilm removal, including correct tooth brushing, flossing, and use of the water irrigation device. She mastered the new techniques and understood the significance of this new behavioral change that was reinforced at every hygiene and clinical visit. The diagnostic wax-up and the proposed treatment plan were thoroughly discussed with the patient and her parents. They gave approval for the treatment plan, and the restorative/surgical phase 1 appointment was made. For comparison, the diagnostic casts showing the preliminary and post wax-ups are shown in Figure 4.
 |
| Figure 5. Photo showing the conservative crown preparation and preservation of enamel for deciduous teeth C, D, G, and H. |
 |
 |
| Figure 6. Gypsum model of tooth preparation for fabrication of the provisional crowns. | Figure 7. LuxaCrown (DMG America) resin material was selected for long-term aesthetic provisionalization of the maxillary anterior teeth. |
Clinical Phase
The patient was sedated by an anesthesiologist for the extended appointment to complete the restorative and preliminary surgical procedures.
The primary teeth to be restored had partially resorbed roots and were severely worn, with approximately only half of the clinical crowns remaining. Conservation of enamel was paramount to provide sufficient enamel surface area for bonding during phase 1 of her treatment. The preparation design preserved as much tooth enamel as possible, only removing sharp corners/angles created by the wear. Conservative full-coverage micro-preparations were completed on the 4 teeth as demonstrated in Figure 5. The mesial aspect of teeth Nos. 8 and 9 were bonded chairside to close the diastema that was present and provide more aesthetic contours.
 |
 |
| Figure 8. Utilization of a vinyl polysiloxane (VPS) putty guide served to secure composite material onto the preparation model to fabricate the provisional restorations. |
 |
| Figure 9. Provisional restorations on the model, ready for trimming and refinement. |
Laboratory Phase
In the dental laboratory, an immediate plaster model was made from the vinyl polysiloxane (VPS) impression taken of the tooth preparations. The model was trimmed to allow the putty (Precision Putty [Denmat]) guide made from the diagnostic wax-up to fit over the tooth preparations. The teeth on the model were lubricated to prevent the composite material from sticking to the plaster. The LuxaCrown material was placed into the VPS putty stint and then seated over the plaster model and placed in a pressure cooker for a denser and more rapid set of the material. The putty mold was removed, the restorations were trimmed, the occlusion was adjusted, and the restoration was polished. The restorations were then returned to the operatory for delivery to the patient following the tooth extractions (Figures 6 to 9).
 |
| Figure 10. Bonded LuxaCrown provisional restorations provided enhanced aesthetics and orthodontic guidance and stability. |
 |
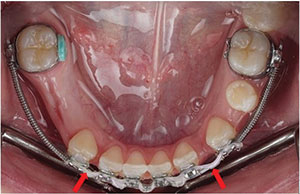 |
| Figure 11. A more favorable arch form and tooth/space distribution were achieved after the deciduous posterior teeth were extracted and the incisors were restored to ideal dimensions. | Figure 12. Orthodontic presurgical treatment with deciduous teeth extracted. Anterior spacing was left for stabilization wires post-surgery. |
 |
 |
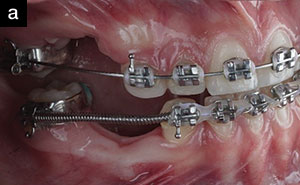
| Figure 13. Right (a) and left (b) lateral views of orthodontic treatment orchestrated through well-coordinated interdisciplinary care. |
The oral maxillofacial surgeon (Dr. Larry Lorenzi, Newport Beach, Calif) extracted all the ankylosed teeth without complications while the laboratory team completed the indirect restorations. The restorations were tried in to evaluate the fit, aesthetic display, and occlusion. All clinical goals were accomplished, patient approval was obtained pre-sedation, and the restorations were bonded individually for greater control and precision. Each preparation was cleaned, etched, and bonded with a resin-modified glass ionomer cement (RelyX Luting Plus Cement [3M]). The excess resin was removed with a resin-moistened microbrush (Scotchbond Single Bond Universal Adhesive [3M]) prior to final curing. Teeth Nos. 8 and 9 were restored using direct composite resin (Filtek Supreme Ultra Universal Restorative, shade A1 [3M]) to eliminate the diastema (Figure 10).
Follow-up
The patient was evaluated one week postoperatively and demonstrated excellent healing. She was very pleased with the aesthetic improvement that the anterior restorations had created for her. She stated that she was smiling much more. She was referred back to her orthodontist to commence her presurgical orthodontic therapy. The patient was maintained on a 3-month hygiene and oral health review schedule that continues to the present time. Her orthodontic treatment has been completed (Figures 11 to 13), and she has been scheduled for the orthognathic surgery in the summer of 2019.
CLOSING COMMENTS
Newly available restorative materials provide excellent alternatives when longer-term provisional stabilization and restoration of dental patients who are undergoing long-term multi-phase prosthodontic rehabilitation are required. This cost-effective, long-term approach is beneficial from a mechanical, a functional, an aesthetic, and an economic perspective. In this ectodermal dysplasia patient, the
LuxaCrown material proved perfectly suited to provide strong, aesthetic, and functional restorations until she is ready to proceed with her final restorative phase.
References
- Pigno MA, Blackman RB, Cronin RJ Jr, et al. Prosthodontic management of ectodermal dysplasia: a review of the literature. J Prosthet Dent. 1996;76:541-545.
- Van Sickels JE, Raybould TP, Hicks EP. Interdisciplinary management of patients with ectodermal dysplasia. J Oral Implantol. 2010;36:239-245.
- Kaul S, Reddy R. Prosthetic rehabilitation of an adolescent with hypohidrotic ectodermal dysplasia with partial anodontia: case report. J Indian Soc Pedod Prev Dent. 2008;26:177-181.
- Clarke A. Hypohidrotic ectodermal dysplasia. J Med Genet. 1987;24:659-663.
- Crawford PJ, Aldred MJ, Clarke A. Clinical and radiographic dental findings in X linked hypohidrotic ectodermal dysplasia. J Med Genet. 1991;28:181-185.
- Koyuncuoglu CZ, Metin S, Saylan I, et al. Full-mouth rehabilitation of a patient with ectodermal dysplasia with dental implants. J Oral Implantol. 2014;40:714-721.
- Knobloch LA, Larsen PE, Saponaro PC, et al. Early implant placement for a patient with ectodermal dysplasia: thirteen years of clinical care. J Prosthet Dent. 2018;119:702-709.
- Mascolo A, Boschetti E, Flanagan D. An ectodermal dysplasia patient treated with a small diameter implant supporting a single crown. Clin Cosmet Investig Dent. 2018;10:171-177.
- Alsayed HD, Alqahtani NM, Alzayer YM, et al. Prosthodontic rehabilitation with monolithic, multichromatic, CAD-CAM complete overdentures in an adolescent patient with ectodermal dysplasia: a clinical report. J Prosthet Dent. 2018;119:873-878.
Dr. Sheets maintains a full-time private practice in Newport Beach, Calif, for aesthetic rehabilitative dentistry. She is an international educator, a clinician, an author, and a researcher. She is a Fellow of the AGD, the American College of Dentists (ACD), the International College of Dentists (ICD), the Pierre Fauchard Academy (PFA), and the Academy of Dentistry International. Dr. Sheets is founder and co-executive director of the Newport Coast Oral Facial Institute (NCOFI), a non-profit international teaching and research center for dentists and dental technicians, in Newport Beach, Calif. She and James C. Earthman, PhD, professor of material science and bioengineering at the University of California Irvine School of Engineering, are leading research on energy dissipation in teeth and implants. They hold numerous US and international patents on the technology for quantitative percussion diagnostics. Dr. Sheets can be reached at cgsheets@ncofi.org.
Dr. Paquette is a past president of the American Academy of Esthetic Dentistry and the Pacific Coast Society of Prosthodontics (PCSP) and serves on the editorial board of the Journal of Prosthetic Dentistry. She is recognized nationally and internationally as a leader in aesthetic dentistry, prosthodontics, and implant dentistry. She is a Diplomate of the American Board of Prosthodontics and a Fellow of the American College of Prosthodontists. She holds fellowships in the ICD, the ACD, and the PFA. She is also a member of the American Academy of Restorative Dentistry and the Academy of Osseointegration. Dr. Paquette has authored numerous research and clinical articles on her areas of expertise and co-authored several textbook chapters. She is co-executive director of the NCOFI. Dr. Paquette can be reached at jmpaquette@ncofi.org.
Dr. Wu is on the executive council for the PCSP and a past president of the Academy of Microscope Enhanced Dentistry. She is also a member of the ADA, the California Dental Association, and the Orange County Dental Society (OCDS). She was a board member of the OCDS in 2011 and a senior delegate in 2012. Currently, Dr. Wu is a partner in the Sheets, Paquette & Wu Dental Practice and on the faculty at the NCOFI. She is also actively involved with several research projects on dental implants and materials and has published articles in several dental journals. Dr. Wu can be reached at jcwu@ncofi.org.
Disclosure: The authors report no disclosures.
Related Articles
The Epidemic of Cracked and Fracturing Teeth
America’s ToothFairy Celebrates a Decade of Service
New Technique Simplifies Bone Graft Procedures











