As dentists learn to look beyond “teeth and gums,” they will discover how they have the power to alter a dentition to enhance a patient’s facial features. After all, the oral cavity provides the internal structure supporting the lower one third of the face. Aesthetic dental procedures have changed the standards of all the dental specialties. The entire dental team must share the same vision and work together for the patient’s benefit. Advances in techniques and materials have opened the door to possibilities that were not previously possible. The restorative dentist must learn to act as the “quarterback” (team leader), calling the plays to achieve the final outcome.1 The dental clinician, in this role, must listen to the patient, establishing realistic treatment goals. Furthermore, the clinician must have a clear vision of the desired final result, be familiar with the procedures available from the various dental specialties, be able to plan the sequence of treatment, and act as the general contractor, overseeing every detail.
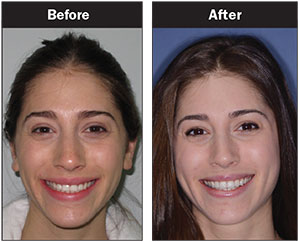 |
| Before Image. Preoperative photo. After Image. The beautifully restored and naturally appearing teeth. A very happy patient. |
When establishing a treatment plan, the dental paradigm has shifted to what is now referred to as “facially generated treatment planning.”2 In other words, the patient’s face dictates the treatment plan. A dentist should look at a patient’s face and profile and assess if the dentition is in the correct position for ideal facial aesthetics. We observe the patient’s lips, cheeks, chin, skin, etc, and then evaluate if the maxillary anterior tooth position and gingival levels are in aesthetic harmony.3 The clinician is unable to establish an ideal occlusion until the desired position of the maxillary central incisors has been established, as this will dictate the vertical and horizontal positions as well as the guidance pathways. Then one can look at the position of the mandibular teeth and assess if they are in the correct position to support the desired position of the maxillary arch. Lower arch discrepancies affect the position of the upper arch and result in deviations in the incisal and occlusal planes.
CASE REPORT
Background
My daughter’s 23-year-old friend, Emma, asked if I could look at her teeth and then share an opinion as to their appearance and health (Before Image). Orthodontics had been completed when she was age 16. Just a few weeks prior to her request for an opinion, she had returned to her orthodontist concerned about the incisal wear that she was noticing. The orthodontist told her that everything was fine, stating that she should consider getting a nightguard from her general practitioner (GP) since she was “grinding” her teeth (Figure 1).
She returned to her GP and was then told that she was “stressed out” and was “brushing too hard.” Impressions were taken for a maxillary occlusal guard. Emma was then told that she needed gingival grafting and the subsequent placement of 6 porcelain veneers. She felt a sense of urgency in the dentist’s voice. Why was this never previously mentioned? She had just had her regular checkup 6 weeks earlier and was told that absolutely everything was fine. What was wrong with this picture? She had always done everything that was recommended, did not have a single restoration in her mouth, and was now suddenly in need of gingival grafts and artificial porcelain teeth.
 |
| Figure 1. Clinical signs of bruxism (wear). |
 |
| Figure 2. Loss of canine guidance. |
Diagnosis and Treatment Planning
Upon examination of her teeth, we observed that the maxillary anterior teeth had lost approximately 2.0 mm from the incisal edges.4-6 As teeth wear, (1) the positions of the teeth change, (2) the gingival levels become unharmonious, (3) the papillary positions and the contact lengths move, (4) maxillary tooth display decreases, (5) the anterior smile-line morphs into a reverse curve, and (6) the centrals and laterals lose their proportion, becoming more square in shape. We concluded that the width-to-length ratio of Emma’s incisors had diminished and that the subsequent incisal wear led to the loss of canine guidance, resulting in an edge-to-edge bite (Figure 2). Gingival recession occurred as a result of abfraction to teeth Nos. 10 and 11, and supereruption of teeth Nos. 6 and 7 caused the gingiva to move incisally. The occlusal view photos of the maxillary and mandibular arches illustrate near ideal arch form with a very slight amount of lower anterior crowding (Figure 3).
 |
| Figure 3. Near ideal arch form with slight mandibular crowding. |
 |
 |
| Figure 4. Photo drawing illustrating changes that had occurred. | Figure 5. Taking the iTero scan (Align Technology). |
The key to establishing a treatment plan is to be able to visualize the ideal endpoint of treatment and then compare it with the current condition. If the desired result does not match the way the teeth presently are, then the restorative quarterback must determine what steps are needed, and in what sequence the treatment should take place. Every case begins by evaluating the aesthetics first. We must always reference the maxillary tooth position and gingival levels relative to the face, determining if and how they must be changed. We cannot establish occlusal issues until we determine the final aesthetic vision. Aesthetics will dictate where to put the teeth. I generally use a typodont study model as a reference for “ideal.”
Treatment planning a case begins by using a retracted photo of the patient’s dentition. This is used to visualize the gingival levels, tooth position, tooth arrangement, contours, length-to-width ratios, and so on. The photo can also be drawn on, thus becoming a tool to illustrate any changes that are to be made. In Emma’s case, her maxillary anterior teeth appeared to be in ideal position, only displaying incisal wear and gingival changes (Figure 4).
By drawing on the photo, one can visualize the desired form and position of the maxillary teeth. Then, the position of the lower teeth must be evaluated. Why? In the author’s concept, the lower arch is really the “upper” arch! Lower dental arch discrepancies result in deviations in the incisal and occlusal planes. By looking at our study models, we can judge if the lower mandibular incisors are in the correct position to accommodate the proposed restoration to the upper arch. We must carefully assess the tooth arrangement as to midline, overbite, overjet, wear, mobility, fractures, and signs of disharmony. Does the anterior envelope of function allow the posterior teeth to disclude, or is the patient in “auto grind”? In Emma’s case, there was a slight amount of lower mandibular crowding and anterior flaring resulting in a minimal amount of overjet. The incisal wear patterns on the upper teeth aligned with the corresponding lower antagonists, resulting in attrition. Attrition happens when teeth rub against each other, resulting in wear. Although most people are “low responders” who can tolerate this amount of minimal crowding with no consequences, there are always some individuals who cannot. A “high responder” is sensitive to every little stimulus, reminiscent of the fairy tale of The Princess and the Pea. Emma was a driven student wanting to excel at every activity in which she participated, and she totally fit the description of the “high responder.” It was concluded that her mandibular incisors had to be aligned and retracted, creating adequate overjet to allow the upper anterior teeth to be restored to their original length.
 |
 |
| Figure 6. Virtual models using Insignia 3D software (Ormco). |
Clinical Protocol
An iTero (Align Technology) intraoral scan was taken of Emma’s teeth and bite, creating a virtual model (Figure 5). Using Insignia 3D software (Ormco), the orthodontic objectives of aligning and intruding the lower anterior teeth were established (Figure 6).7,8 Customized Damon brackets (Ormco) were bonded to the teeth (Figure 7) and first (horizontal) and second (vertical) order bends placed in the specified wire. Orthodontic treatment was achieved in 9 weeks (Figure 8). An Ortho-Flextech (Reliance Ortho Products) retention wire was then bonded to the lingual surface of the lower anterior teeth (Figure 9). A sufficient amount of overjet was created in order to have enough space to restore the maxillary incisal edges, and to re-establish anterior guidance with a cuspid-protected envelope of function (Figure 10).
 |
 |
| Figure 7. Damon brackets (Ormco) were placed on the lower arch. | Figure 8. Orthodontic treatment was completed in 9 weeks. |
 |
 |
| Figure 9. A lingual retention wire (Ortho-Flextech [Reliance Ortho Products]) was placed on the lower incisors. | Figure 10. Space was created to accommodate the restoration of the maxillary teeth. |
 |
 |
| Figure 11. Face-bow record (Artex [Jensen Industries]). | Figure 12. An inflexible acrylic bite registration was taken (LuxaBite [DMG America]). |
 |
 |
| Figure 13. Diagnostic wax-up. | Figure 14. A nanohybrid composite resin (IPS Empress Direct [Ivoclar Vivadent]) was used to make the incisal additions. |
The restorative quarterback has to be able to visualize the arrangement, contour, and color of the teeth the patient desires. In Emma’s case, this was straightforward. Our goal was just to put back what had been taken away. A face-bow record was taken (Artex Facebow [Jensen Industries]) (Figure 11). Then, a bite registration was taken using LuxaBite (DMG America). Luxabite is an acrylic bite registration material with a setting time of 2 minutes. It is extremely accurate and, since it is acrylic, it does not have the flexibility of silicone bite registrations where even the slightest movement results in inaccuracies. Because the material is not flexible, there is only one way to mount the case (Figure 12). A diagnostic wax-up was created on the articulated study models (Figure 13) illustrating the incisal additions that were to be made.
When choosing a material to use for a dental restoration, we must consider biological, structural, spatial, and logistical issues. We must evaluate the space available for the restoration, the mechanical forces the restoration must absorb, and how we can achieve adequate retention for the restorative material. As Emma’s teeth were healthy, and the treatment goal was to restore the missing incisal edges, bonded composite resin restorations were the best choice. These minimally invasive restorations, requiring minimal tooth preparation, are capable of producing lifelike aesthetics. In addition, the clinician can use them to assess the future wear to the teeth by observing how often they break. They are easy to repair and can be upgraded to porcelain veneers at any time. Dental porcelains and bonding materials will certainly improve in the future and, since Emma was a young patient, there would be plenty of time for porcelain later, if needed.
A 2.0-mm featheredge bevel was prepared in enamel, to serve as a ferrule to which to bond. A beautiful and strong nanohybrid composite (IPS Empress Direct [Ivoclar Vivadent]) was chosen for this case. The enamel bevel was treated with Etch-Rite (Pulpdent), 38% phosphoric acid, for 15 seconds and then copiously rinsed, leaving a frosty surface which was then coated with ALL-BOND UNIVERSAL (BISCO Dental Products), according to the manufacturer’s instructions. The nanohybrid composite restored the form of the teeth and left them looking as nature intended them to be (Figure 14).
In Emma’s case, what we did for her was exactly what I would do for my own daughter (After Image).
CLOSING COMMENTS
Our dental office runs by the philosophy of treating all patients as if they were family. Therefore, we always suggest the treatment choices that we would offer to our own close relatives. It is good for the long-term health of our practice. After all, we want to be on speaking terms with our all of our patients in 20 years!
Acknowledgment
The author would like to thank Brita Nadeau, DMD, Cert Ortho (Montreal, QB, Canada).
References
- Mechanic E. Interdisciplinary treatment planning: the restorative quarterback. Dent Today. 2015;34:72-75.
- Mechanic E. Anterior tooth challenges, part 4: Canines in the lateral position. Dent Today. 2014;33:84-89.
- Vig RG, Brundo GC. The kinetics of anterior tooth display. J Prosthet Dent. 1978;39:502-504.
- Sarver DM. The importance of incisor positioning in the esthetic smile: the smile arc. Am J Orthod Dentofacial Orthop. 2001;120:98-111.
- Kokich VG. Esthetics and vertical tooth position: orthodontic possibilities. Compend Contin Educ Dent. 1997;18:1225-1231.
- Kokich V. Esthetics and anterior tooth position: an orthodontic perspective. Part II: vertical position. J Esthet Dent. 1993;5:174-178.
- Kokich VG, Spear FM. Guidelines for managing the orthodontic-restorative patient. Semin Orthod. 1997;3:3-20.
- Sarver DM, Ackerman MB. Dynamic smile visualization and quantification: Part 2. Smile analysis and treatment strategies. Am J Orthod Dentofacial Orthop. 2003;124:116-127.
Dr. Mechanic received his bachelor of science (1975) and doctor of dental surgery (1979) degrees from McGill University. He maintains membership in numerous professional organizations, including the American Academy of Cosmetic Dentistry, the Academy for Dental Facial Esthetics, the American Society for Dental Aesthetics, and the European Society of Cosmetic Dentistry. He practices aesthetic dentistry in Montreal, Canada, is the aesthetic editor of Canada’s Oral Health dental journal, and is on the editorial board of Dentistry Today. He also is the co-founder of the Canadian Academy for Esthetic Dentistry, program coordinator of the University of Toronto Advanced Restorative Continuum, and recognized as a leader in continuing dental education. His work has been profiled in magazines, television, and radio. He can be reached at info@drmechanic.com.
Disclosure: Dr. Mechanic reports no disclosures.











