In the world of restorative dentistry, every day is a new day. You never know what may be coming your way! The restorative dentist must often act as a quarterback1 to coordinate multidisciplinary treatment approaches to patient care. The clinician must be familiar with the growing number of restorative techniques and dental material options, and realize that having a go-to bag of tricks can make the difference between poor and spectacular treatment outcomes.
This article will be focused on 2 of 4 brothers who presented with varying numbers (3 to 18) of congenitally missing teeth. Having 4 brothers present with this many congenitally missing teeth is certainly not a common everyday occurrence in a dental practice!
CONGENTIALLY MISSING TEETH: CLASSIFICATIONS AND ETIOLOGY
There are various terms used in the classification of congenitally missing teeth. Hypodontia is the term used when fewer than 5 teeth are missing. Oligodontia is when a patient is missing 6 or more permanent teeth. Someone born without any deciduous or permanent teeth is said to have anodontia.
Hypodontia is highly prevalent in the population. Early recognition is essential for diagnosis, treatment planning, and restoration.2 However, oligodontia is rare, affecting 0.09% of the population, usually occurring in conjunction with other genetic disorders such as ectodermal dysplasia, Van der Woude syndrome, Down syndrome, or Rieger syndrome. Oligodontia has seldom been observed to occur as an isolated entity. Thirty percent of oligodontia patients have a reduced secretion of saliva, and 10% have a reduction in function of their sweat glands. Syndromic and nonsyndromic forms of oligodontia can be differentiated by a thorough examination of hair, nails, sweat glands, eyes, etc.
 |
 |
| Figure 1. Vincent (age 21 years), missing 3 teeth. | Figure 2. Louis (age 24 years), missing 9 teeth. |
 |
 |
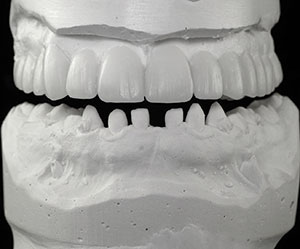
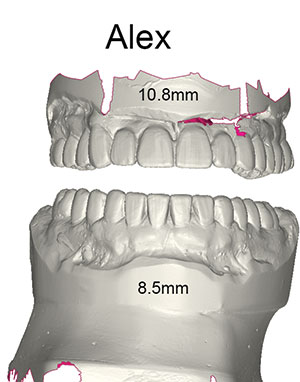
| Figure 3. Thomas (age 16 years), missing 15 teeth. | Figure 4. Alex (age 16 years), missing 18 teeth. |
Missing teeth have been reported with an increase in maternal age, low birthweight, and multiple births.3,4 A wisdom tooth is the most commonly missing tooth, occurring in 25% to 35% of the population. Upper lateral incisors are missing as frequently as 2%, and when only one lateral is missing, the other is usually misshaped or a microdont. Often, the central incisors and canines may also be misshaped. The incidence of missing second premolars has been reported to be as high as 3%.5
 |
 |
| Figure 5. An orthodontic appliance was used to open the vertical dimension of occlusion (VDO) in the centric relation position and to align the teeth. |
Missing teeth not only affect appearance but can also contribute to situations involving dental breakdown. Moderate to severe malocclusion, impaired chewing ability, periodontal problems, insufficient alveolar bone growth, and difficulties in pronunciation can create complicating consequences. Treating these situations can be time-consuming, costly, and painful.
The precise etiology of congenitally missing teeth is believed to originate from environmental or genetic factors during dental development. There is an increased frequency in twins, leading one to believe that the condition is programmed from the time of conception. Although research has shown that genetics play a dominant role, the exact genetic mechanism is unknown. It is believed that mutations of divergent genes coding for transcription factors, such as MSX1 and PAX9, are responsible.6-8
 |
 |
| Figure 6. The VDO was re-established with a positive overjet and a pleasing profile for one of the twins. (The same result was achieved with his twin brother.) | Figure 7. A LuxaBite registration (DMG America) captured the desired VDO. |
 |
| Figure 8. The completed bite registration. |
Oral Rehabilitation Considerations
The oral rehabilitation of a patient with congenitally missing teeth begins with early recognition. It is usually both an orthodontic and a restorative issue with the restorative dentist typically acting as the team leader for the multidisciplinary treatment of the patient’s care. Procedures and materials available in the various dental disciplines should be evaluated, and realistic treatment objectives should be established based upon the patient’s needs and expectations. A clinical protocol is determined that often involves periodontal, orthodontic, and implant treatments. Misshapen and malformed teeth are sometimes built to ideal proportions before orthodontics begins. The restorative dentist must interact with the participating specialists throughout the treatment, while also checking and taking radiographs to visualize root proximity, angulations, and if adequate space is available for the proposed restoration (implants, fixed bridgework, or removable dentures).9 Missing teeth are a dental anomaly that is debilitating, time-consuming, and a financial burden for the patient.
CASE REPORT
For this family, every sibling was affected by missing teeth. Their mother is a dental hygienist, which made communication and her understanding of the problem much easier.
 |
| Figure 9. Mounted study models. |
 |
 |
| Figure 10. The maxillary diagnostic wax-up. | Figure 11. The completed upper full-arch and lower full-arch diagnostic wax-ups. |
 |
 |
| Figure 12. A stereolithography file was created from an optical scan of the diagnostic wax-up. | Figure 13. Snap-On Smile appliances (DenMat). |
Vincent, age 21 years, was missing 3 premolars and had already completed orthodontics (Figure 1). Louis, age 24 years, had 9 missing teeth and was left with a deep bite after orthodontics (Figure 2). It was decided to retreat him with orthognathic surgery to correct the shift in his mandible. Then he would be retreated orthodontically to be able to establish an ideal vertical dimension, leaving precise spacing to eventually replace all his missing teeth with implants and to reconstruct his misshapen teeth to ideal proportions.
The focus of this case report article will be on a pair of 16-year-old twin brothers: Thomas, who was missing 15 teeth (Figure 3), and Alex, who was missing 18 teeth (Figure 4). They required what I refer to as disaster relief dentistry.
The twins had nearly identical severe bite collapses with the mandibular teeth completely overlapping the uppers. Since early childhood, the boys had been followed by the dental department of a pediatric hospital. The supervising orthodontist had informed their parents that there was nothing that could be done until the boys were older and finished growing. They would then have an “operation” to move their lower jaws “into the proper position” so that restoration could be possible. The parents were told that it was impossible to improve upon what their sons had at this time in their lives. I believe that the orthodontist in that busy hospital clinic probably assumed that they were Angle Class 3 and would require mandibular orthognathic surgery. This diagnosis was based solely by looking at the teeth without placing the patients in the appropriate vertical dimension.
From the conversations that we had, I believed that the psychological effect on the twins was just as important as their dental condition. Although both brothers easily accommodated to chewing and speech, they felt that they were constantly perceived as being “different.” Having understanding friends, strong family values, confidence, and inner strength are what led them into adolescence. With high school graduation approaching, the boys and their family really hoped that something could be done aesthetically, even if it was only temporary. I believed that, if the existing permanent teeth could be placed in their appropriate positions, a removable prosthesis (Snap-On Smile [DenMat]) could be fabricated over the existing teeth, recreating vertical dimension, function, aesthetics, and phonetics. This noninvasive prosthesis could be used for restorative assessment and, in addition, as a template for the eventual placement of implants and fixed restorations.
 |
 |
| Figure 14. Post-op photo of Alex. | Figure 15. Post-op photo of Thomas. |
 |
| Figure 16. Post-op profile view of one of the twins. (The same result was achieved with his twin brother.) |
I introduced myself to the treating orthodontist via telephone and, unfortunately, I was immediately met with aggressive resistance. She was insulted that I questioned her diagnosis and said that what I proposed would cause irreversible temporomandibular joint (TMJ) problems and result in the twins losing all their teeth. I explained that they were currently at the wrong vertical dimension of occlusion (VDO) and, if opened with cotton rolls, they displayed normal profiles. I also clarified that I would be opening their bite to the centric relation (CR) position, and that current research has shown that opening the vertical dimension is safe and predictable. Furthermore, it does not create problems in the TMJ and any negative effects are self-limiting.10 I was then told that I did not know what I was talking about, was not an orthodontist, and should not interfere.
I believe in the concept of health professionals working together for the benefit of the patient.11 Egos should be left at the door. I believed that a Snap-On Smile was a simple solution to help Alex and Thomas feel and immediately appear like other teenagers their age. I explained the situation to the parents. They tried to approach their orthodontist and were again told that there was nothing that could be done until the boys were older. Understanding that what I was proposing was completely reversible, and knowing how important aesthetics were to their sons, the parents chose to abandon their orthodontist and continue care with us, under our treatment plan.
A full set of radiographs and a digital intraoral iTero scan were taken. The vertical dimension would be opened based on ideal aesthetic dimensions. The stomatognathic system can adapt rapidly to a change in the vertical dimension. There is no indication in the current research that a permanent alteration of occlusal dimension will produce long-lasting TMJ symptoms. Transient discomfort can occur, usually not lasting longer than 2 to 3 months.12 In many instances, opening the vertical dimension is beneficial in the following ways: (1) to create adequate space for the restoration, (2) to enhance aesthetic tooth display, (3) to reestablish a physiologic occlusion, (4) to avoid crown lengthening, and (5) to avoid cutting teeth (thus maintaining tooth structure).
Every dental treatment plan begins by first evaluating the facial aesthetics referencing the patient’s lips, cheeks, skin, etc. We always begin the dental evaluation by looking at the position of the maxillary central incisors and their gingival levels relative to the face to evaluate if and how they must be changed. The occlusal scheme cannot be established until we determine the desired position of the upper anterior teeth. The position of the maxillary 6 anterior teeth will dictate the vertical display as well as establish the pathways of guidance. Ideally, if orthodontics is indicated, the final position of the existing permanent teeth should be centered within the proposed restoration. Once we have the parameters of the position of the upper arch, we can then set the position of the mandibular teeth accordingly.
An upper Hawley retainer was fabricated with posterior occlusal acrylic coverage, which allowed sufficient bite opening for the correction of the anterior crossbite. Anterior springs were used to bring teeth Nos. 7 and 8 slightly more buccal. Hooks were soldered onto the molar Adams clasps to allow placement of CL III elastics. Caplan hooks were bonded to the deciduous mandibular canines to support the CL III traction and, to increase anchorage, an Essix appliance was placed, covering the entire lower arch (Figure 5). Upon initial observation, the bite was extremely closed and the maxilla appeared to be retrognathic. By opening the bite, it was observed that we would achieve a positive overjet. If this position could be maintained, it may stabilize whatever is remaining of the residual growth. If surgery would be necessary in the future, it would most likely be a maxillary advancement (Figure 6).
The twins wore CL III Ormco 5/16 light (3 oz) elastics (Ormco) on this setup for 4 months. The VDO was comfortable and the profile was pleasing. We felt that we were ready for impressions and a bite registration. A digital optical scanning system is ideal for this situation as there are no tooth preparations necessary, and all the information that needs to be captured is supragingival, which greatly simplifies the process. For the sake of this article, I chose to take traditional impressions and bite registration. The impressions were taken with StatusBlue (DMG America), a vinyl polysiloxane with a firm consistency that remains dimensionally stable and can be poured multiple times.
The bite registration was taken with a bis-acryl material (LuxaBite [DMG America]) with glass filler in a matrix of multifunctional methacrylates. I prefer to register the LuxaBite with cheek retraction so that the patient bites passively into the material with minimal resistance and no interference from the patient’s cheeks that could disturb the material. The use of cheek retractors also allows me to be able to visually ascertain that the patient is biting properly, as there is an unobstructed field of vision. The secret to using LuxaBite is to use it sparingly, placing it as a ribbon and being sure not to allow it to flow and engage in any undercuts. The material is easy to trim and does not compress for mounting, as do polyvinyl materials. LuxaBite is conveniently dispensed from a 10:1 gun and sets to a Barcol hardness of 20.
Leaving the orthodontic bite appliance in place to maintain the VDO and to open the patient’s bite in the CR position, we initially placed LuxaBite on the anterior section and allowed it to set for 2 minutes (Figure 7). The material set to a rigid consistency, locking the desired anterior bite into place. We then did a second-stage technique, removing the bite appliance and adding the LuxaBite to the posterior sections, then joining it to the previously taken anterior section (Figure 8). LuxaBite is a highly accurate bite registration, allowing us to capture the CR bite at the appropriate/desired VDO.
The study models were then poured with Silky-Rock low-expansion stone (Whip Mix) and mounted on an Artex Articulator (Jensen) (Figure 9). A conventional wax-up was created for the upper arch, based upon the parameters established by our orthodontic setup, allowing for a maxillary central incisor length of approximately 11.0 mm. The rest of the tooth dimensions can be easily extrapolated based on the size of the centrals (Figure 10). Once the shape and form of the upper arch was complete, the lower arch was added, establishing anterior guidance, midline, and overbite overjet parameters (Figure 11).
As previously stated, these procedures are ideal for a digital scan, smile design, and the wax-up. For the sake of this article, the presentation is conventional. Having a diagnostic wax-up in hand gives us the benefit of being able to physically visualize it and thus make modifications before fabricating the restoration. However, with current advancements in 3-dimensional printing, this step is not essential.
The diagnostic wax-up was optically scanned by the lab (DenMat) (Figure 12) and a stereolithography digital file was created. Proprietary CAD software was then used to design the Snap-On Smile. Specialized pucks of acetal resin were then milled to the prescribed parameters (Figure 13). The pucks come in a variety of shades. Once milled, the appliances were trimmed, finished, and polished.
The Snap-On Smile appliances snapped into place exactly as claimed. Made of crystalized acetal resin, they display unique flex characteristics. The material expands over the heights of the contours of the teeth, creating the snap effect. What a thrill it was to see the twins look at their new smiles for the first time (Figures 14 and 15). Neither appliance required any adjustment whatsoever. The CR position prescribed vertical dimension and bite registration, and the working models proved to be extremely accurate and created a pleasing profile (Figure 16). Speech and comfort were easily adapted to by the patients within a few days. The twins wear these appliances all the time, removing them only for cleaning, with no negative effects. Entirely tooth-borne, the appliances do not impinge on the gingival tissue.
Once the twins stop growing and are ready for phase 2, the next step is to plan the placement of implants according to the positions set forth in the Snap-On Smile appliances. Restoration at that point should be straightforward with the ultimate goal being to restore their dentitions with individual implants and ceramic restorations.
CLOSING COMMENTS
What appeared to be a crisis situation turned into simple case management. Although the final restoration is far from complete, the first phase’s outcome was life changing and satisfied the twins and their family. The intermediate Snap-On Smile appliances not only gave them noninvasive immediate gratification but also set the parameters for their future implant restoration by establishing an appropriate and tested vertical dimension with the ability to judge if the existing permanent teeth are in appropriate position to accommodate the final restoration. Until the actual Snap-On Smile appliances were placed in their mouths, there was no way to be completely sure.
As exemplified herein, the Snap-On Smile appliances, when used as diagnostic devices, can be an invaluable tool. And, from a psychological perspective of the patient, they can be life changing! Sometimes, simple solutions are all that is really needed. Knowing about them is the secret.
Acknowledgment
The author would like to thank Brita Nadeau, DMD, Cert Ortho (Montreal, QC, Canada).
References
- Mechanic E. Interdisciplinary treatment planning: the restorative quarterback. Dent Today. 2015;34:72-77.
- Larmour CJ, Mossey PA, Thind BS, et al. Hypodontia—a retrospective review of prevalence and etiology. Part I. Quintessence Int. 2005;36:263-270.
- AlShahrani I, Togoo RA, AlQarni MA. A review of hypodontia: classification, prevalence, etiology, associated anomalies, clinical implications and treatment options. World Journal of Dentistry. 2013;4:117-125.
- Schalk van der Weide Y, Prahl-Andersen B, Bosman F. Tooth formation in patients with oligodontia. Angle Orthod. 1993;63:31-37.
- Kokich VG, Kokich VO. Congenitally missing mandibular second premolars: clinical options. Am J Orthod Dentofacial Orthop. 2006;130:437-444.
- De Coster PJ, Marks LA, Martens LC, et al. Dental agenesis: genetic and clinical perspectives. J Oral Pathol Med. 2009;38:1-17.
- Lyngstadaas SP, Nordbo H, Gedde-Dahl T Jr, et al. On the genetics of hypodontia and microdontia: synergism or allelism of major genes in a family with six affected members. J Med Genet. 1996;33:137-142.
- Vastardis H. The genetics of human tooth agenesis: new discoveries for understanding dental anomalies. Am J Orthod Dentofacial Orthop. 2000;117:650-656.
- Forgie AH, Thind BS, Larmour CJ, et al. Management of hypodontia: restorative considerations. Part III. Quintessence Int. 2005;36:437-445.
- Abduo J. Safety of increasing vertical dimension of occlusion: a systematic review. Quintessence Int. 2012;43:369-380.
- Mechanic E. Focus on: interdisciplinary dentistry. Dent Today. 2014;33:18.
- Moreno-Hay I, Okeson JP. Does altering the occlusal vertical dimension produce temporomandibular disorders? A literature review. J Oral Rehabil. 2015;42:875-882.
Dr. Mechanic received his bachelor of science (1975) and doctor of dental surgery (1979) degrees from McGill University, and practices aesthetic dentistry in Montreal, Canada. He maintains membership in numerous professional organizations, including the American Academy of Cosmetic Dentistry, the Academy for Dental Facial Esthetics, the American Society for Dental Aesthetics, and the European Society of Cosmetic Dentistry. Dr. Mechanic is the co-founder of the Canadian Academy for Esthetic Dentistry. For Dentistry Today, he is a member of the advisory board of and is also listed as one of its leaders in continuing education. He can be reached via the email address: info@drmechanic.com.
Disclosure: Dr. Mechanic reports no disclosures.
Related Articles
Interdisciplinary Treatment Planning: What Would You Do If She Were Your Daughter?
Reversing Genetic Mutations Can Restore Smiles











