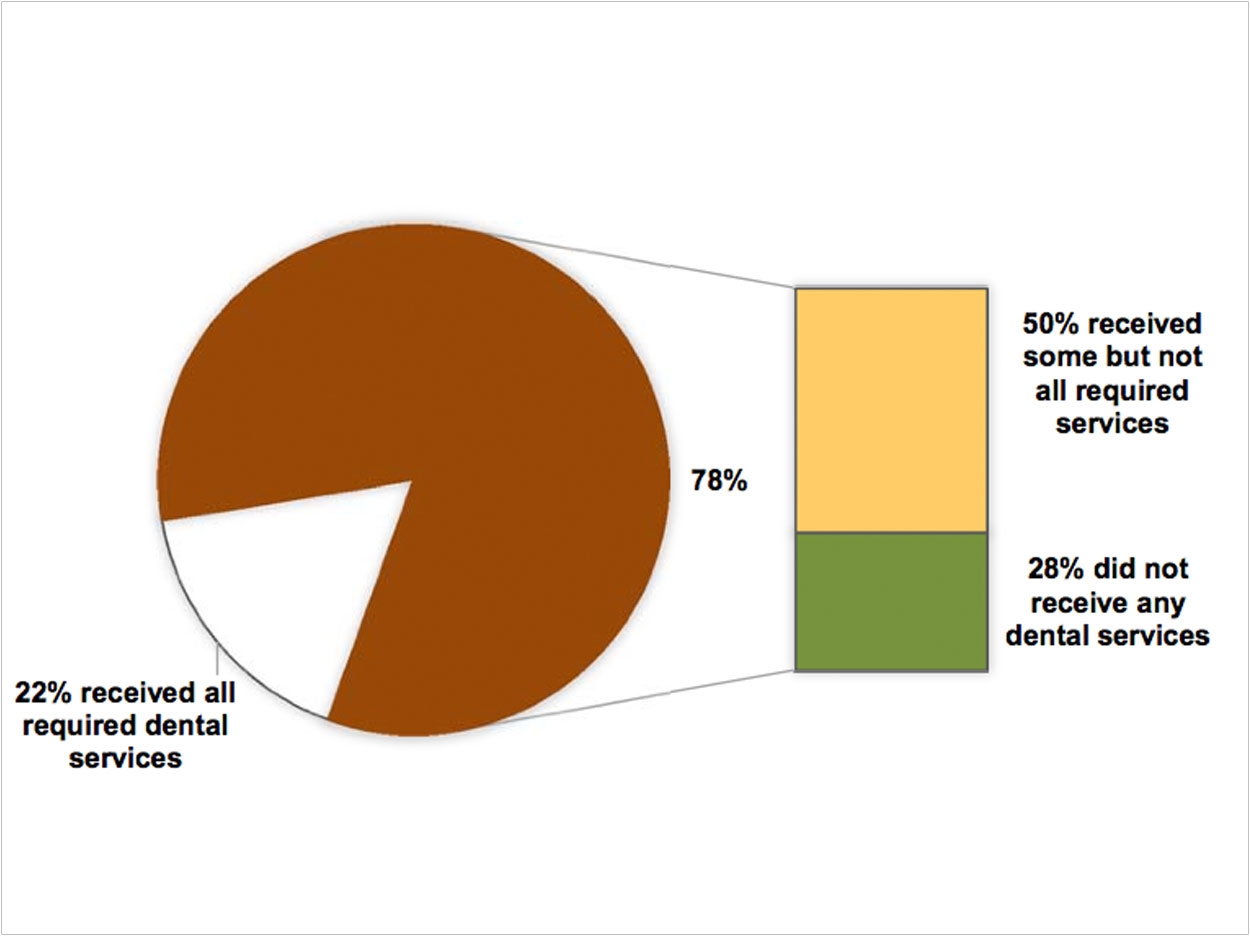
As tooth decay grows among pediatric populations, access to dental care remains challenging. The Department of Health and Human Services (DHHS) reports that Medicaid is the primary source of dental coverage for children in low-income families, supporting care for about 37 million children. Yet 3 out of 4 children in a DHHS study did not receive all required services, with one of those 4 not seeing a dentist at all.
Medicaid’s Early and Periodic Screening, Diagnostic, and Treatment program requires states to cover all medically necessary dental services at the intervals specified in their pediatric dental periodicity schedules. The department’s study then focused on California, Indiana, Louisiana, and Maryland, which collectively serve approximately 19% of all children on Medicaid, and analyzed their 2011 and 2012 claims and other data.
Specifically, the study looked at 3 required services—biannual oral exams, dental cleanings, and fluoride treatments—for children continuously enrolled in Medicaid for 2 years. According to the data, 22% received all required services, yet 50% received some but not all services. Plus, 28%, or more than one million children, did not receive any dental services at all. Percentages varied by state.
None of these states routinely track whether children are receiving all of the required services, while 2 of the states do not allow payment for particular services in accordance with their periodicity schedules. These states also reported shortages of participating dental providers and difficulties in educating families about regular dental care.
“This isn’t the first time we’ve heard of such issues,” said Colin Reusch, senior policy analyst with the Children’s Dental Health Project (CDHP). “In fact, CDHP has specified the need to align periodicity and payment policies with clinical guidelines and caries risk factors in previous policy briefs.”
The study additionally noted the importance of dental homes, or ongoing relationships between pediatric patients and their dentists. While 86% of the children who received all the required services visited the same practice during the course of 2 years, the children who received only some of the required services were more likely to visit multiple practices.
“Oral health improves when children have access to regular, preventive dental care,” said Dr. Brad Bryan, managing director of Kool Smiles, a dental health provider operating in 15 states, including Louisiana. “By providing a Medicaid dental home to Louisiana children who have historically lacked access to a dentist, we are able to reduce the potential for more expensive procedures over time.”
The DHHS Office of Inspector General has provided the Centers for Medicare & Medicaid Services (CMS) with 8 recommendations to monitor and ensure the required services:
- Develop a comprehensive plan to increase the number of children who receive required services;
- Develop benchmarks for dental services and require states to create mandatory action plans to meet them;
- Work with states to identify areas with limited providers and barriers that prevent providers from participating in Medicaid;
- Work with states to analyze the effects of Medicaid payments on access to dental providers;
- Work with states to educate families about the importance of dental care and encourage ongoing relationships between children and dentists;
- Work with states to track children’s utilization of required dental services;
- Identify and share effective strategies with states; and
- Ensure that states pay for services in accordance with their periodicity schedules.
The CMS is now concluding its 5-year Oral Health Initiative, which is aimed at increasing utilization rates for preventative dental services and dental sealants. Between 2007 and 2011, 24 states achieved at least a 10 percentage point increase in the proportion of children enrolled in Medicaid and the Children’s Health Insurance Program. Yet the DHHS study reveals that work needs to continue.
“More must be done to ensure that Medicaid-enrolled children receive the dental services that are identified in states’ periodicity schedules,” said Reusch. “At the same time, Medicaid policies should ensure that each child receives the individualized care that reflects his or her risk for tooth decay.”
Related Articles
31% of Kids Miss School Due to Dental Problems
Kids at Higher Risk for Cavities Are Missing Preventive Treatments
Stressed Moms Have Kids with More Cavities












