A Case Series and Review of the Literature
INTRODUCTION
It seems like cracked teeth are becoming a more and more prevalent finding in clinical practice. The ADA News and the New York Times recently published articles on this subject. One reason is people are living longer and are retaining their natural dentition. “Cracked teeth seem to be a result of repetitive stress injury, and so the longer teeth are in use, the more likely they will become cracked. This is a modern epidemic and something we have never before as a profession had to deal with,” said Rob Roda, past president of the American Association of Endodontists. “Cracked teeth are undergoing a time-dependent, load-related, progressive process that, without intervention, results in pain, infection, and splitting of the tooth requiring extraction.”
A cracked tooth can be defined as an incomplete fracture initiated from the crown and extending cervically and sometimes subgingivally, usually directed mesiodistally.1 The depth and extent of the fracture are usually unknown and may progress to communicate with the pulp and/or periodontal ligament.
A cracked tooth diagnosis can be very perplexing because of the very vague nature of the presenting signs and symptoms. Do we treat, or do we extract? Studies show that the range of treatment for the cracked tooth can vary from conservative treatment modalities to extraction and replacement with implants. When a crack is suspected, guiding the patient to the proper treatment and then following up is paramount. The initial symptoms of a cracked tooth can often mimic those of pulpitis, necrosis, or apical periodontitis while there are clinically and radiographically no signs of caries. Most of the time, the involved tooth is minimally restored or not restored at all, making the diagnosis all the more difficult (Figure 1). The goal of this article is to help the practitioner navigate the complexities of diagnosing and treating the cracked tooth.
COMMON CRACK LOCATION
Mandibular first and second molars are the most susceptible to fracture, followed by the maxillary premolars. The crack is most often found on the mesial or distal marginal ridge or under an existing restoration.2-4
DIAGNOSING THE CRACKED TOOTH
Understanding the extent of the crack is important as well. A craze line is a small crack that does not extend past the enamel. Teeth with craze lines will not cause any sensitivity to biting or temperature, and no treatment is necessary. Once a crack extends into the dentin, the patient can start to have temperature sensitivity and biting pain. As long as the crack does not extend into the root canal space, the crack can be managed by making a crown to establish complete cuspal protection. This treatment protocol is dependent on the patient’s symptoms.
If a tooth is minimally restored (or not restored at all) and has no caries yet presents with symptoms of pulpitis or necrosis, a cracked tooth should be suspected (Figures 1 and 2). These teeth can be retained if diagnosed and treated in a timely manner. The prognosis drops precipitously if the tooth has become necrotic. This would suggest that the crack has been there for a much longer period of time.5
Classic symptoms of a cracked tooth include sharp pain on biting (or release) and unexplained temperature sensitivity. Often, the patient has difficulty pinpointing the offending tooth, which makes reproducing the patient’s chief complaint all the more critical. One of the best ways to diagnose a cracked tooth is by testing each cusp of a suspected cracked tooth with a “tooth sleuth.”6 Cotton roll compression is another technique that can be employed.2-4 Vitality testing is important as well. These tools will help to pinpoint the offending tooth.
Early diagnosis and detection are paramount in the management of the cracked tooth. With early detection, many teeth can be saved. Unfortunately, because the pain is intermittent, and due to the vague nature of the symptoms, there may be a delay in treatment. Many cracks are diagnosed when they have already extended deeply into the root structure, making the prognosis hopeless (Figures 2 and 3). These cracks also provide an avenue for bacteria to invade the pulp space, eventually leading to either an inflamed pulp (pulpitis) or an infected pulp (necrosis/apical periodontitis).5,7 The cause of the sharp pain on biting is due to the movement of the fractured segments triggering fluid movement within the dentinal tubules. This fluid movement triggers nerve fibers located in and around the dentinal tubules.8
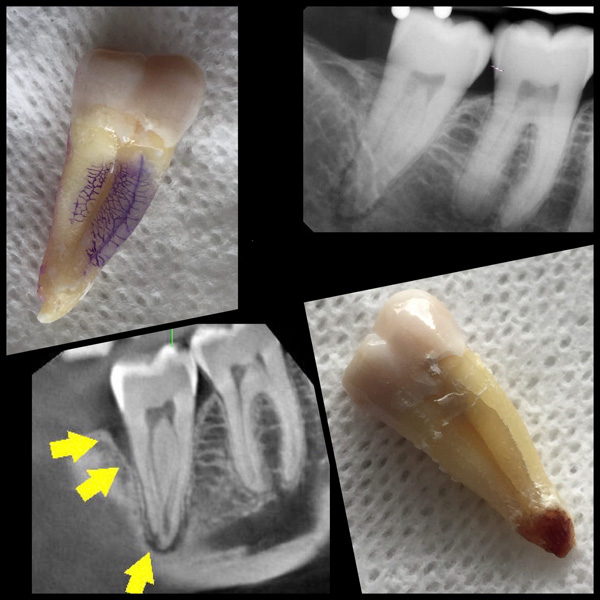
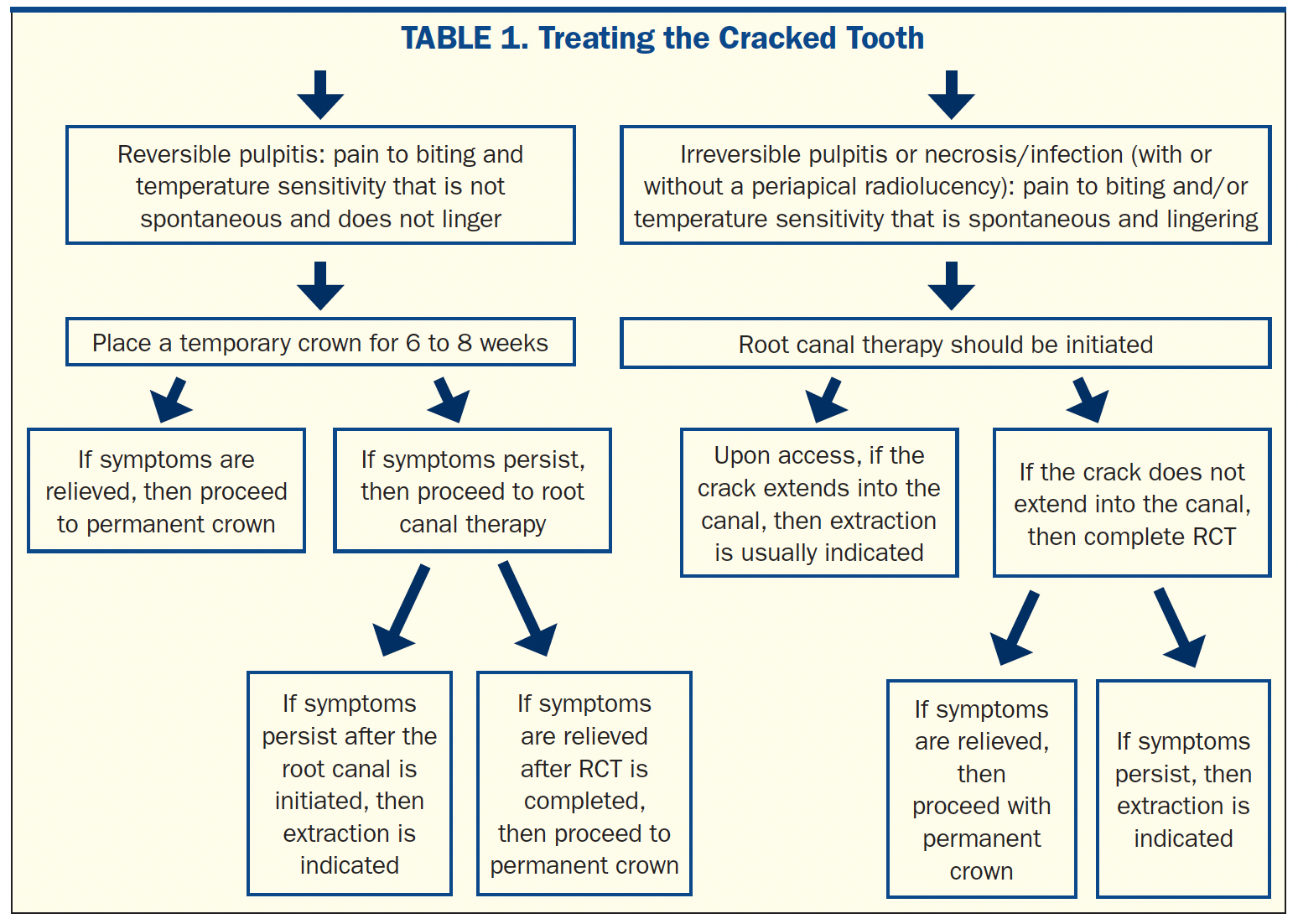
Figure 1 The patient in this case had been to multiple dentists over the past 2 years with a vague discomfort on the lower right side. Due to a lack of caries or restorations and the inability to reproduce the patient’s chief complaint, no treatment was rendered. A CBCT scan (Veraviewepocs 3D R100 [J. Morita]) revealed periapical radiolucency, as well as a narrow vertical defect, on the distal aspect of tooth No. 31. This was confirmed with clinical periodontal probing depths of 8 mm. This tooth also tested negative to vitality testing. A diagnosis of a cracked tooth with radicular extension was made, and extraction was recommended. All symptoms subsequently resolved. The extracted tooth revealed a crack running down the full extent of the buccal aspect of the mesial root. There was a second crack (not visualized) on the distal aspect corresponding with the distal bone loss.
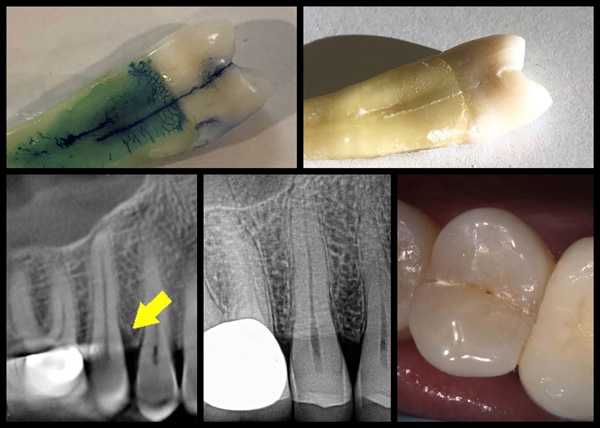
Figure 2 The patient in this case presented with severe acute biting pain on the upper right. Tooth No. 4 was extremely tender to percussion and biting. There were no caries or restorations on tooth No. 4. You can see a crack line running mesial to distal on the occlusal table. A 7-mm periodontal pocket was probed on the mesial. A diagnosis of a cracked tooth with radicular extension was made. After the tooth was extracted, you can visualize the crack running from the mesial marginal ridge halfway down the root.

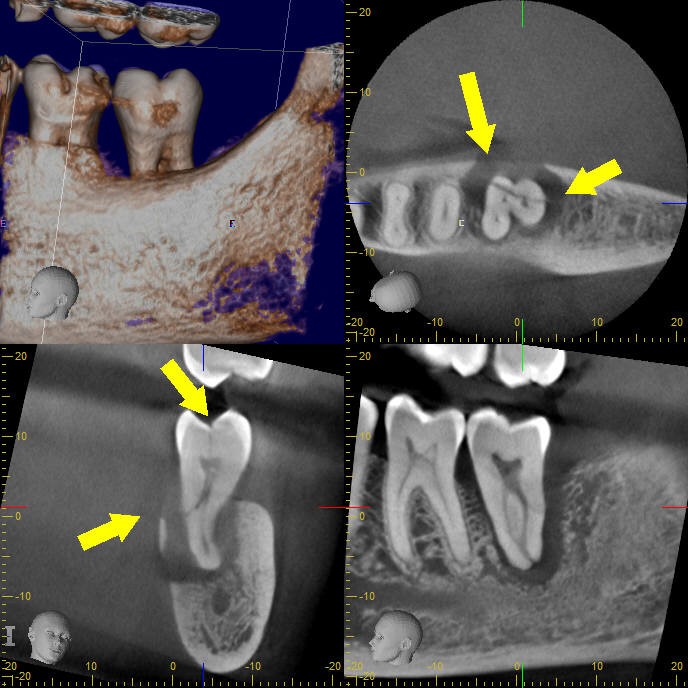
Figure 3 Tooth No. 18: The patient presented with severe pain to biting and continuous throbbing pain on the lower left. A diagnosis of pulp necrosis with symptomatic apical periodontitis was made. CBCT images revealed the cause being a cracked tooth extending in a mesiodistal direction and obliquely to communicate with the PDL on the lingual. The extent and direction of this fracture was not visualized on conventional radiography.
TREATMENT OF THE CRACKED TOOTH
There is a wide range of treatment options for the cracked tooth. Treatment will usually fall into 1 of 3 categories:
1. Crown
2. Root canal and crown
3. Extraction
The treatment depends on the status of the pulp and the depth of the crack. A surgical operating microscope is essential in determining the extent of the crack and the prognosis once the root canal is initiated.
If a cracked tooth is diagnosed with reversible pulpitis (no lingering sensitivity to biting or thermal stimulation), a temporary crown is advised for 6 to 8 weeks. If symptoms resolve, then proceed with a permanent crown. If symptoms don’t resolve, root canal therapy is indicated prior to permanent crown placement.2-4
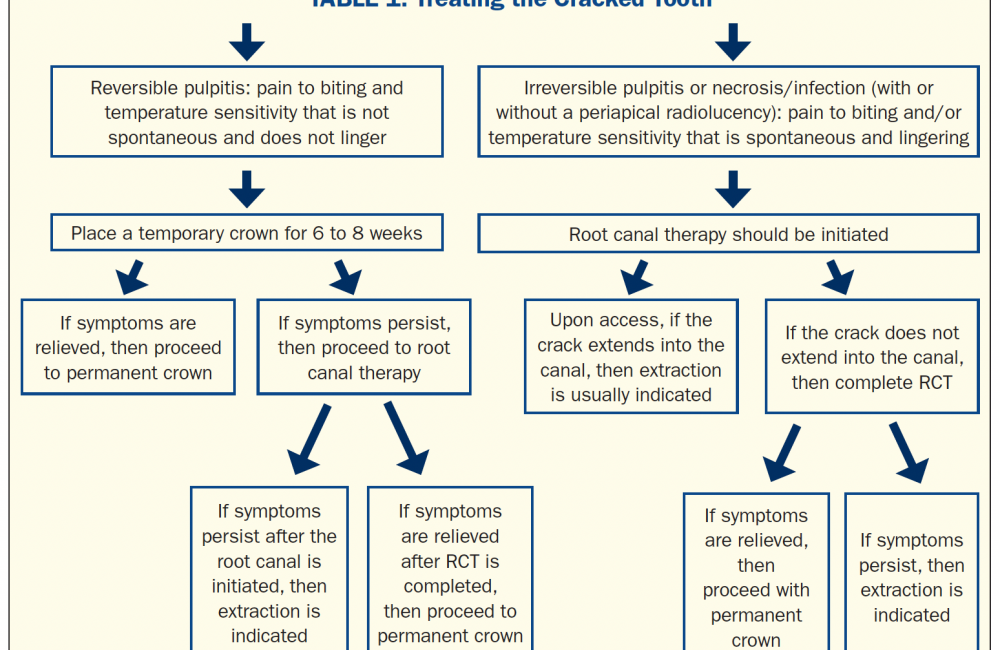
If a cracked tooth has a pulpal diagnosis of irreversible pulpitis (a crack that elicits spontaneous or lingering pain) or necrosis (infection) with or without a periapical lesion, then root canal therapy is indicated prior to crown placement (Table 1) (Figures 4 and 5). If root canal treatment is initiated and it’s discovered that the crack extends into the root, then extraction may be indicated.5,9-13 A recent study showed very promising results when treating a cracked tooth, even when the crack extended into the radicular dentin.14 The technique employed used intra-orifice barriers placed apically to the apical extent of the crack in the radicular dentin. The goal was to prevent the ingress of bacteria and reinforce cervical dentin.14
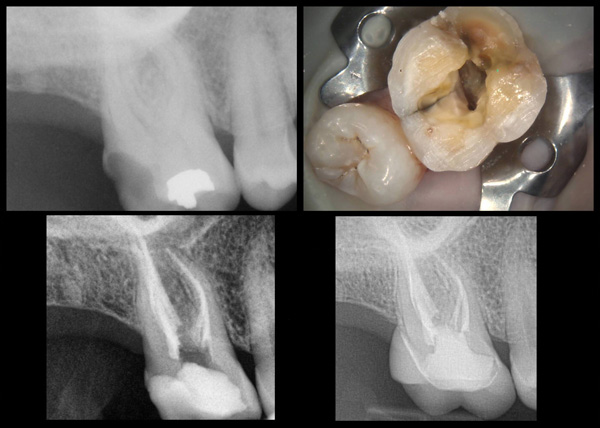
Figure 4 The patient in this case presented with signs and symptoms of a cracked tooth (visualized clearly upon access of the tooth) and irreversible pulpitis associated with tooth No. 3. The patient was motivated to save the tooth with root canal therapy and a crown. The patient was completely asymptomatic after the first visit. The tooth was crowned one month after the root canal was completed. At the 2-year followup, the patient presented asymptomatic. The radiograph revealed no periapical pathology or marginal bony breakdown.
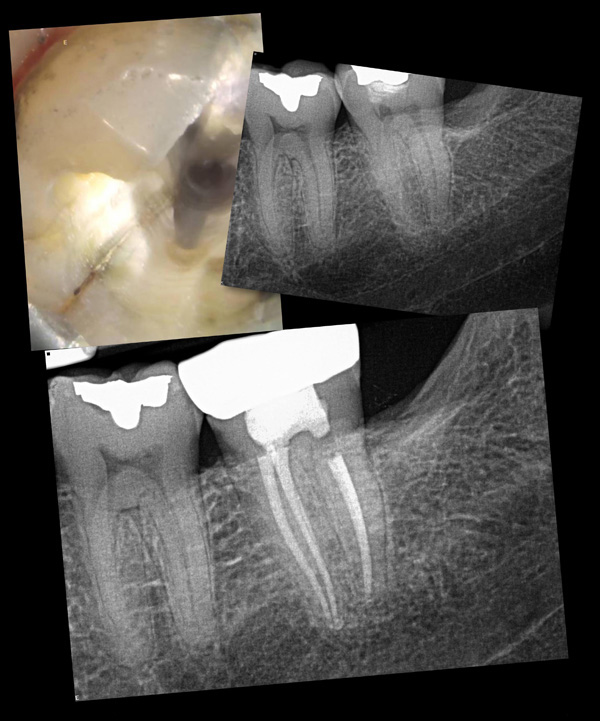
Figure 5 The patient in this case presented with acute biting pain on the lower left. A tooth sleuth revealed biting pain associated with the ML cusp of tooth No. 18. There was a lingering, painful response to vitality testing. Upon access, a crack line was noted running from the occlusal surface down to the level of the ML canal but not into the canal. A cracked tooth was diagnosed. The patient opted to have this tooth endodontically treated and then crowned. Upon the 3-year evaluation, the tooth was asymptomatic with no signs of periapical pathology or periodontal breakdown.
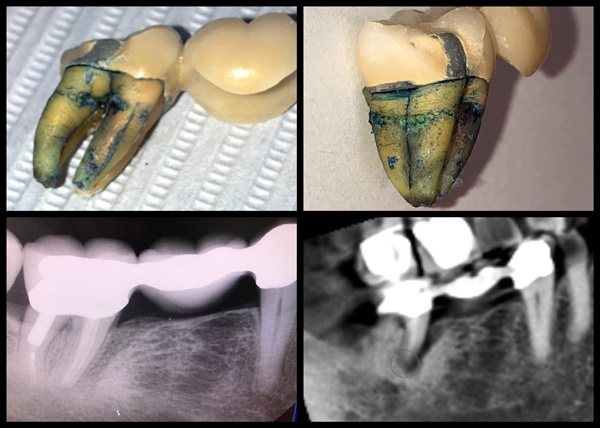
Figure 6 The patient in this case presented with a vague discomfort on the lower right. The gingiva adjacent to tooth No. 31 was inflamed and slightly swollen. The initial diagnosis was a periodontal abscess. Local curetting of the area temporarily relieved the patient’s pain. However, the patient returned with a similar discomfort after a short time. A CBCT scan was recommended and revealed a J-shaped radiolucency on the mesial root of tooth No. 31. A 10-mm periodontal pocket was probed on the mesiobuccal aspect of tooth No. 31. A diagnosis of vertical root fracture (VRF) was made, and extraction was recommended. After the tooth was extracted, a fracture was not only noted on the mesiobuccal, as expected, but surprisingly also along the distal root.
CRACKED TOOTH VS VERTICAL ROOT FRACTURE
A cracked tooth shouldn’t be confused with a vertical root fracture (VRF). VRFs are mostly found in previously endodontically treated teeth. These fractures are initiated at the apical end and progress coronally (Figure 6). They can also be found mid-root adjacent to the terminus of a post. On the other hand, cracked teeth are found mostly in teeth that have not had root canal treatment, and the crack is initiated in the crown and spreads apically toward the root (Figure 7). Cracked teeth can sometimes occur on endodontically treated teeth that have not been properly restored with cuspal coverage. Cracked teeth are often directed in a mesiodistal direction (Figure 8), while VRFs are mostly directed in a buccolingual direction within the root. The classic J-shaped or halo-shaped apical radiolucency, as well as the deep, narrow “isolated” periodontal pocket, is classically associated with VRFs (Figure 6). In contrast, classic symptoms of biting pain and unexplained temperature sensitivity are associated with cracked teeth.15-18 While cracked teeth are amenable to a range of treatments, VRFs usually have a hopeless prognosis and require extraction and replacement with an implant. If the offending tooth is multi-rooted, it may be possible to resect the root with the VRF and retain the tooth with the remaining roots (Figure 9). Because the pain associated with VRFs may be fleeting and intermittent, the patient often doesn’t seek treatment until significant bone has been lost around the tooth.

Figure 7 The patient in this case presented with extreme pain on the entire right side of his face, extending into his ear. The patient reported on and off biting pain and temperature sensitivity over the prior 2 months. The pain had recently became unbearable. A clinical exam revealed that tooth No. 31 had pain on biting as well as a 7-mm probing depth on the distal. There was no response to vitality testing. A cracked tooth with radicular extension was diagnosed, and the tooth was planned for extraction. The extracted tooth revealed a crack running from the distal marginal ridge deep into the root structure.
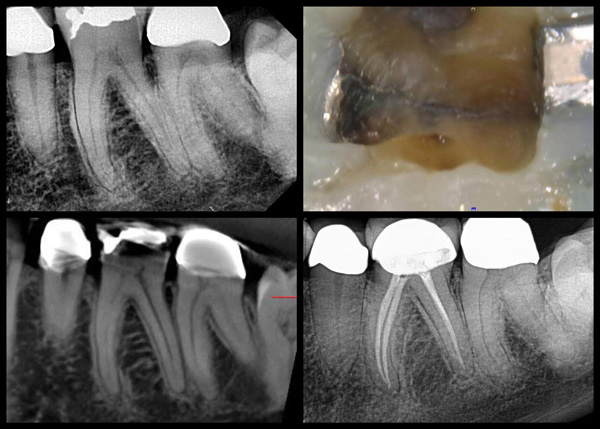
Figure 8 The patient in this case presented with a chief complaint of on and off biting discomfort on the lower left. Tooth No. 19 was very sensitive to percussion and cotton roll compression. The cold test was inconclusive. A CBCT scan revealed PDL widening at the apex of the mesial and distal roots. Tooth No. 19 was planned for “exploratory” root canal therapy and a crown. After the amalgam was removed, a crack (cracked tooth) was seen running from the mesial to the distal. Once access was made into the pulp chamber, the full extent of the crack could be visualized running on both the mesial and distal aspects of the crown but not down to the pulpal floor. The patient returned for the second visit, reporting that all symptoms had subsided. The root canal was completed, and the patient was referred back to her dentist for the crown. The patient returned for the 10-month re-evaluation with a core buildup and permanent crown (no post). The tooth was completely asymptomatic, and the radiograph revealed no signs of periapical pathology or periodontal breakdown.
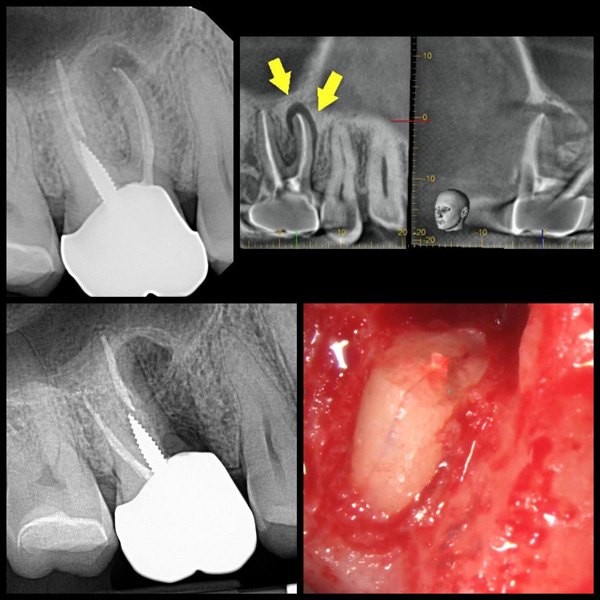
Figure 9 The patient in this case presented with a previously endodontically treated tooth No. 3. The chief complaint included a dull discomfort around the apical region of tooth No. 3. Radiograph examination revealed a periapical breakdown around the apex of No. 3. The J-shaped radiolucency around the MB root was strongly indicative of a VRF. The patient was very motivated to save this tooth, and a root resection was planned. Upon flap reflection and removal of granulation tissue, a VRF was clearly visualized. The MB root was resected.
ETIOLOGY OF THE CRACKED TOOTH
Cracked teeth are the result of repetitive stress to the dentition. They can also be the result of sudden stress on a vulnerable tooth. Repetitive stress would result from parafunctional habits such as bruxism and clenching, whereas a sudden stress injury could be the result of biting on ice, nuts, hard candy, etc.
CRACKS WITH AGE
Older patients have a more brittle dentin structure, and as such, their teeth are more prone to fracture. Rarely do we see classic cracked tooth symptoms in children or adolescents. One study found that the dentin is 50% weaker in those above 55 years old in comparison to those younger than 35 years old.19 It seems that the fatigue resistance of human dentin decreases with age.20
PREVENTING CRACKS
One of the best ways to prevent cracking a tooth is to have the patient wear a nightguard if clenching or grinding is a habit.
A patient with a history of a cracked tooth should be evaluated for full-coverage restorations on teeth vulnerable to fracture in the future. It is very common to see a patient have a tooth removed due to a crack, only to return a short time later with a crack on another tooth because the edentulous space was never restored. The lack of a restoration after the loss of a tooth puts more stress on the remaining teeth, thus leading to greater vulnerability for fractures on the remaining teeth.
CONCLUSION
Diagnosing and treating the cracked tooth can be a complex endeavor. Many factors contribute to the proper diagnosis and treatment of the cracked tooth. With a better understanding of cracked teeth, more of these teeth can be saved than previously thought.
A chart outlining a few classic studies associated with cracked teeth and vertical root fractures is available here.
ACKNOWLEGEMENTS
The author wishes to thank Dr. Charles Solomon and Dr. Leslie Elfenbein for their valuable input.
REFERENCES
1. Rivera EM, Walton RE. Cracking the cracked tooth code: detection and treatment of various longitudinal tooth fractures. In: Colleagues for Excellence. Chicago: American Association of Endodontists; 2008
2. Cameron CE. The cracked tooth syndrome: additional findings. J Am Dent Assoc. 1976;93:971–5. doi:10.14219/jada.archive
3. Krell KV, Rivera EM. A six year evaluation of cracked teeth diagnosed with reversible pulpitis: treatment and prognosis. J Endod. 2007;33(12):1405–7. doi:10.1016/j.joen.2007.08.015
4. Kahler W. The cracked tooth conundrum: terminology, classification, diagnosis, and management. Am J Dent. 2008;21(5):275–82.
5. Berman LH, Kuttler S. Fracture necrosis: diagnosis, prognosis assessment, and treatment recommendations. J Endod. 2010;36(3):442–6. doi:10.1016/j.joen.2009.12.018
6. Türp JC, Gobetti JP. The cracked tooth syndrome: an elusive diagnosis. J Am Dent Assoc. 1996;127(10):1502–7. doi:10.14219/jada.archive.1996.0060
7. Ricucci D, Siqueira JF Jr, Loghin S, Berman LH. The cracked tooth: histopathologic and histobacteriologic aspects. J Endod. 2015;41(3):343–52. doi:10.1016/j.joen.2014.09.021
8. Brannstrom M. The hydrodynamic theory of dentinal pain: sensation in preparations, caries, and the dentinal crack syndrome. J Endod. 1986;12(10):453–7. doi:10.1016/S0099-2399(86)80198-4
9. Kang SH, Kim BS, Kim Y. Cracked Teeth: Distribution, Characteristics, and Survival after Root Canal Treatment. J Endod. 2016;42(4):557–62. doi:10.1016/j.joen.2016.01.014
10. Rivera EM, Walton RE. Longitudinal fractures. In: Torabinejad M, Walton RE, eds. Principles and Practice of Endodontics, 4th ed. Philadelphia: Saunders; 2009: 108–28.
11. Tan L, Chen NN, Poon CY, et al. Survival of root filled cracked teeth in a tertiary institution. Int Endod J. 2006;39(11):886–9. doi:10.1111/j.1365-2591.2006.01165.x
12. Sim IG, Lim TS, Krishnaswamy G, et al. Decision making for retention of endodontically treated posterior cracked teeth: a 5-year follow-up study. J Endod. 2016;42(2):225–9. doi:10.1016/j.joen.2015.11.011
13. Krell KV, Caplan DJ. 12-month success of cracked teeth treated with orthograde root canal treatment. J Endod. 2018;44(4):543-548. doi:10.1016/j.joen.2017.12.025
14. Davis MC, Shariff SS. Success and survival of endodontically treated cracked teeth with radicular extensions: a 2- to 4-year prospective cohort. J Endod. 2019;45(7):848-855. doi:10.1016/j.joen.2019.03.015
15. Tsesis I, Rosen E, Tamse A, et al. Diagnosis of vertical root fractures in endodontically treated teeth based on clinical and radiographic indices: a systematic review. J Endod. 2010;36(9):1455–8. doi:10.1016/j.joen.2010.05.003
16. Fuss Z, Lustig J, Tamse A. Prevalence of vertical root fractures in extracted endodontically treated teeth. Int Endod J. 1999;32(4):283–6. doi:10.1046/j.1365-2591.1999.00208.x
17. PradeepKumar AR, Shemesh H, Jothilatha S, et al. Diagnosis of vertical root fractures in restored endodontically treated teeth: a time-dependent retrospective cohort study. J Endod. 2016;42(8):1175–80. doi:10.1016/j.joen.2016.04.012
18. Tamse A, Fuss Z, Lustig J, et al. An evaluation of endodontically treated vertically fractured teeth. J Endod. 1999;25(7):506–8. doi:10.1016/S0099-2399(99)80292-1
19. Yan W, Montoya C, Øilo M, et al. Reduction in fracture resistance of the root with aging. J Endod. 2017;43(9):1494-1498. doi:10.1016/j.joen.2017.04.020
20. Seo DG, Yi YA, Shin SJ, et al. Analysis of factors associated with cracked teeth. J Endod. 2012;38(3):288–92. doi:10.1016/j.joen.2011.11.017
ABOUT THE AUTHOR
Dr. Stern is a Diplomate of the American Board of Endodontics. He is the director of endodontics at the Touro College of Dental Medicine and lectures frequently on the subject of clinical endodontics. He has lectured at many local county dental societies, the New Jersey Dental Association Annual Session in May 2019, and the Greater New York Dental Meeting in 2020. He maintains a private practice, Clifton Endodontics, in Clifton, NJ. He can be reached at jstern5819@gmail.com.
Disclosure: Dr. Stern reports no disclosures.
RELATED ARTICLES