Epidemiologic data indicate that the population is aging and retaining its teeth. As this occurs, wear of the incisal edges of anterior teeth will become a significant clinical problem. In most cases, attrition of the mandibular incisors is seen as loss of the enamel on the incisal edge, leaving the dentin exposed (Figure 1). In some cases the dentin becomes stained, and the patient notices this. In the maxillary arch, the patient notices tooth wear due either to chipping of the incisal edges (Figure 2) or to the increase in incisal translucency where the underlying enamel has worn thin (Figures 3 and 4).
 |
 |
| Figure 1. Discolored worn mandibular incisal edges. | Figure 2. Chipping of worn maxillary incisors. |
 |
 |
| Figure 3. Translucency in the incisal third of the maxillary central incisor due to lingual wear. | Figure 4. Lingual wear of the maxillary central incisor. |
Pinborg has classified tooth attrition as physiologic (the gradual and regular loss of tooth structure as a result of normal mastication); pathologic wear confined to a single tooth or groups of teeth caused by abnormal function or improper position of teeth; or intensified attrition (wear) that is more extensive than would normally be expected.1 One study reported that of 520 older adults, 84.2% had enamel attrition, 72.9% had dentin attrition, and 4.2% had severe attrition.2 It is interesting to note that although tooth wear is usually associated with older adults, Schneider and Peterson reported that 15% of children demonstrate tooth wear due to bruxism.3
Wear of the teeth may be due to bruxism, abrasion, and dietary erosion due to acid dissolution.4-6 In fact, wear of the occlusal surfaces has been characterized as a natural phenomenon with the continuing eruption of the posterior teeth to compensate for loss of tooth substance.7,8 Since tooth wear is in fact physical trauma to the teeth, pulpal changes occur to compensate for the loss of tooth structure.9 There can be evidence of mineralization within the pulp chamber and root canal. Although the treatment of wear is mainly a restorative concern, in cases of severe attrition, it has been reported that 11.6% of 448 patients had either near pulpal exposures or frank pulpal exposures.10
In most clinical cases, tooth wear is not due to a single cause. The wear may be related to a combination of factors including attrition, abrasion, and erosion.11 Attrition usually refers to loss of tooth structure due to wear. Wear can be due to parafunctional occlusal habits, such as bruxism or clenching, or due to the mastication of abrasive foods. Abrasion has been defined as loss of tooth substance due to mechanical means such as toothbrushing with an abrasive paste. Erosion differs from both attrition and abrasion in that loss of tooth structure is due to a chemical process such as acid erosion of the tooth. An example would be a patient with gastrointestinal reflux disease that has stomach acids entering the oral cavity due to acid reflux, which dissolves tooth substance. Mair has investigated the causes of tooth wear, and rather than use the classification schemes described in the past, has focused on mechanisms of wear.12 He has described these mechanisms as surface-to-surface wear, slurry wear (early stage), and corrosive wear (erosion). Surface-to-surface wear of teeth can be either enamel-to-enamel, with contact resulting in microfractures of the enamel structure, or the harder substance (enamel) wearing an opposing softer substrate (dentin). Wear of enamel is generally associated with bruxism. Slurry wear is due to an abrasive slurry between 2 moving tooth surfaces. This is also referred to as “3-body wear” because 3 surfaces are in function— tooth structure on either side of the food substrate. Corrosive wear, also referred to as erosion, is nonmicrobial, acid-induced tooth wear.
 |
 |
| Figure 5. Cupping of the mandibular incisal edges due to slurry, erosive wear. | Figure 6. Worn buccal and lingual cusps on a mandibular molar of a 17-year-old patient. |
Clinically, the diagnosis of these conditions can be made by examining the tooth surfaces in different occlusal positions. Surface-to-surface wear can be seen where the teeth interdigitate. Where slurry wear has occurred, the teeth do not always fit together where the loss of tooth structure has occurred.13 The cupping seen on incisal edges and posterior cusps (the class VI lesion) can be attributed to this type of wear (Figures 5 and 6). Corrosive wear from acids can be caused by ingesting acidic foods and beverages or by stomach acid affecting the teeth as a result of bulimia or stomach acid reflux. In these cases, evidence of corrosive wear is indicated by the presence of restorations protruding above the occlusal plane of the tooth structure.
In recent years data have suggested that for adolescents, there is a relationship between chemical erosion of tooth substrate and ingestion of acidic beverages.14,15 Acid reflux from gastrointestinal reflux disease can also be a major contributor to corrosive wear.16,17 In actuality, the diagnosis of tooth wear is often multifactorial.
Although tooth wear has been associated with older patients, young adults can also demonstrate tooth wear. Pintado and others measured attrition in 18 dental students ages 22 to 30 years old. They found there was an average tooth structure loss of 10.7 after one year and almost twice that amount after 2 years.18 Others13,19,20 found almost 50 of wear over one year.
While bruxism is considered to be the most common cause of tooth wear, with the clinical recommendation to have an oral appliance placed to minimize tooth structure loss from grinding, the diagnosis of erosion should not be ruled out. Tooth wear may be multifactoral, with some chemical erosion occurring, such as the bulimic patient who also grinds the teeth. Khan and coworkers21 analyzed 104 patients in Queensland, Australia with excessive tooth structure loss from erosion and attrition due to bruxism. Their findings indicate that for subjects in the dehydrating environment of South East Queensland, both extrinsic and intrinsic acid erosion was strongly associated with attrition found in bruxers. Toothwear patterns were unreliable indicators of attrition from bruxing alone. Their data suggest that attrition may be the initial cause of tooth wear, but when the wear is severe (with dentin exposed), erosion becomes a more important factor in the progression of wear.
CLINICAL MANAGEMENT OF TOOTH WEAR
Early, subtle tooth wear can be followed and re-evaluated during recall examinations. When the wear requires restorative intervention, less severe anterior wear can be treated with adhesive composite resin.22,23 When the wear is more severe, a number of treatment modalities are available. Bonded porcelain veneers have been used to treat incisal wear.24 Adhesive cast metal restorations have also been used to replace missing tooth structure.25,26 In cases where the occlusion is severely altered by attrition, the only treatment choice may be a reconstruction with crowns and bridges.27-29
In the case of anterior wear, the loss of enamel at the incisal edge can lead to dentin exposure and the continuing loss of tooth structure due to slurry wear. Cook demonstrated progressive wear of anterior teeth using an analogy of crayon wear.30 The tip of the crayon has a narrow diameter. As it is used, the crayon diameter becomes larger, similar to the phenomenon seen with anterior tooth wear. He found that this example educated the patient about the need for treatment.
How does one treat the worn anterior dentition when dentin is exposed and is continuing to wear? In some cases, the patient notices and asks about the discoloration of the exposed dentin on the incisal edges of the mandibular teeth. In other cases the patient notices a bluish translucency at the incisal edges on the facial surfaces of maxillary incisors due to wear on the lingual surfaces, leaving only enamel that is translucent. In some cases, the incisal edges can be restored to the original vertical dimension with direct composite resin.22,31 Hemmings and coworkers32 reported on the restoration of severe anterior wear, including re-establishment of the occlusal vertical dimension. They reported a 89.4% success at 30 months. When composite resin is used to restore the lost tooth structure in the anterior region, it is important that special attention is paid to the principles of occlusion combined with the use of occlusal appliances to minimize future wear.23
The following case report describes a conservative treatment of the worn anterior dentition using direct bonded, wear-resistant composite resin.
CASE REPORT

|
|
| Figures 7 and 8. Chipping and discoloration of the worn mandibular incisors and canines. |
 Figure 9. Maxillary incisors and canines with lingual wear.
|
A 53-year-old man requested treatment for all dental needs. As part of the treatment review, the patient asked if anything could be done for his lower front teeth that were chipped and discolored on the incisal edges (Figures 7 and 8). It was noted during the examination that the maxillary incisors and canines also had significant lingual wear (Figure 9). The diagnosis was anterior tooth wear through the enamel into the dentin with a cupped-out appearance indicative of a combined surface-to-surface and slurry tooth wear pattern. The restorative treatment plan for these teeth was the placement of direct-bonded composite resin to restore the worn incisal edges and cusp tips of teeth Nos. 22 to 27 and the lingual surfaces of teeth Nos. 6 to 11.
In the past, the use of composite resin to restore worn anterior teeth was not successful because tooth preparation to retain the restoration was inadequate. The teeth would be lightly beveled, the dentin roughened with a bur with no definitive preparation, and an adhesive composite resin of insufficient thickness (less than 1 mm) would be placed. Within a short period of time, the restoration would be dislodged during function.31 Success of these restorations depends on a fundamental approach to tooth preparation to ensure durability of the restoration.22
 |
| Figure 10. Placement of the dental dam. |
For this patient, the presence of slight tooth mobility allowed for the placement of the rubber dam without the need to reshape the incisal embrasures. When punching the holes in the rubber dam for the mandibular incisors, the smallest hole in the rubber dam punch is used. The holes should be positioned over the center of each tooth, leaving adequate interseptal rubber dam to displace the gingival papillae. Here the rubber dam was placed from the right to the left mandibular second premolar (Figure 10).
Tooth Preparation
Before preparing the dentin, the enamel surface was finished and polished using an abrasive disk system (EP Polishing System, Brasseler USA) from medium to fine grit. A final polish of the enamel was accomplished using a Dialite intraoral rubber abrasive enamel polishing point (Brasseler, USA). The finishing and polishing of the enamel surface removes any irregularities of the enamel and loose enamel rods that can fracture after the completion of the restoration.
 |
 |
| Figure 11. Preparation with a 329 bur. | Figure 12. Depth of preparations are 1 mm. |
Using a small, pear-shaped 329 bur, a preparation was made into the dentin to a depth of 1 mm (Figure 11). The 329 bur was used because it has a length of 1 mm, which was the preparation depth desired (Figure 12). A periodontal probe can also be used to verify the 1-mm pulpal depth of the tooth preparation for all enamel walls. This depth into the dentin allows for adequate composite resin retention during function. The preparation removes only dentin, leaving a shell of enamel. Because the enamel may be very thin in some areas, the enamel may chip away during preparation. This is not a significant problem, since the composite resin will restore that surface.
Restoration Placement
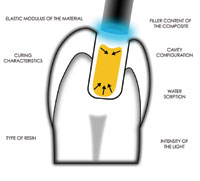
After tooth preparation, a self-etching adhesive (Tenure UniBond, Den-Mat) was placed into the preparations with a microapplicator and agitated for 20 seconds. The adhesive was gently air-thinned and dried, keeping the air syringe 4 to 6 inches from the surface of the tooth so that the adhesive would not pool within the cavity preparations. The adhesive was light-cured for 10 seconds with a blue LED curing light (Allegro, DenMat). The latest generation of LED curing lights has been shown to be equivalent to conventional quartz halogen curing lights.33 The light tip of the Allegro LED curing light differs from most other LED curing lights. The fiber-optic bundles at the end of the light probe adjacent to the LED gallium nitride blue emitter have a modified geometry (concave bowl-shaped). This shape creates a total internal reflector (TIR). TIR refers to the capturing of the light ray on the interface of the LED and the light probe and resultant transfer of the light energy with no loss of energy per reflection.34 Even at 2 mm from the surface, the Allegro provides a depth of cure and microhardness equivalent to actual contact with the composite resin.
 |
| Figure 13. Placement of nanofilled hybrid composite resin (Virtuoso Universal). |
Once the adhesive was light-cured, a wear-resistant, nanofilled hybrid composite resin (Virtuoso Universal, Den-Mat) was placed into the incisal preparations (Figure 13). The composite resin was shaped, keeping the end of the plastic filling instrument (AB1 PFI, Hu-Friedy) flush to the facial and lingual cavosurface margins so that there was little excess remaining to be finished. This also allows the composite resin to be placed with little if any change in the occlusal vertical dimension. The composite resin was then light-cured for 10 seconds holding the light tip at right angles to each tooth.
Finishing and Polishing
 |
| Figure 14. Finishing excess composite resin on the facial surface with a needle-pointed finishing bur (ET3). |
 |
| Figure 15. Finishing excess on the incisal edges with a composite resin finishing disk. |
 |
| Figure 16. Final polish with a diamond-impregnated silicone disk. |
 |
| Figure 17. Preparation of the worn lingual surfaces of maxillary anterior teeth. |
 |
| Figure 18. Maxillary teeth restored with self-etching adhesive and nanofilled composite resin. |
 |
| Figure 19. Final restoration of the maxillary anterior teeth. |
 |
| Figure 20. Final restoration of the mandibular anterior teeth. |
There was very little excess composite resin. In most cases, finishing can begin with a medium, abrasive-backed disk. In this case, some excess composite resin was removed using a needle-ended finishing bur (ET 4EF, Brasseler USA) (Figure 14). The remainder of the finishing for these restorations was accomplished using abrasive disks from a composite resin finishing system (EP Polishing System, Brasseler USA), progressing from coarse to medium to fine (Figure 15). The final polish was accomplished using silicone abrasive diamond-impregnated finishing disks (Dialite Polishers, Brasseler USA) (Figure 16). The rubber dam was removed, and then the maxillary incisors with lingual wear were treated following the same protocol. The teeth were prepared as previously described with a 329 bur (Figure 17). The self-etch adhesive and composite resin were placed, finished, and polished (Figure 18). All occlusal movements were checked using a very thin, 2-sided occlusal film (AccuFilm II, Parkell). Hyperocclusive contacts were adjusted. The restored incisal edges made the teeth more wear-resistant and created a more aesthetic appearance (Figures 19 and 20).
CONCLUSION
In the past, practitioners would watch and evaluate worn incisal edges of anterior teeth as they continued to wear. The only choice to restore these teeth was full-coverage, porcelain-metal crowns. The conservative technique described in this article provided a wear-resistant composite resin restoration to maintain the occlusion on the anterior tooth surfaces and defer or eliminate the need for more extensive crown restorations.
References
1. Pindborg JJ. Pathology of the Dental Hard Tissues. Philadelphia, Pa: WB Saunders; 1970:294-300.
2. Hand JS, Beck JD, Turner KA. The prevalence of occlusal attrition and considerations for treatment in a noninstitutionalized older population. Spec Care Dentist. 1987;7:202-206.
3. Schneider PE, Peterson J. Oral habits: considerations in management. Pediatr Clin North Am. 1982;29:523-546.
4. Kaidonis JA, Townsend GC, Richards LC. Abrasion: an evolutionary and clinical view. Aust Prosthodont J. 1992;6:9-16.
5. Mair LH, Stolarski TA, Vowles RW, et al. Wear: mechanisms, manifestations and measurement. Report of a workshop. J Dent. 1996;24:141-148.
6. Bishop K, Kelleher M, Briggs P, et al. Wear now? An update on the etiology of tooth wear. Quintessence Int. 1997;28:305-313.
7. Murphy TR. The progressive reduction of tooth cusps as it occurs in natural attrition. Dent Pract Dent Rec. 1968;19(1):8-14.
8. Fishman LS. Dental and skeletal relationships to attritional occlusion. Angle Orthod. 1976;46:51-63.
9. Mjor IA. Pulp-dentin biology in restorative dentistry. Part 5: clinical management and tissue changes associated with wear and trauma. Quintessence Int. 2001;32:771-788.
10. Sivasithamparam K, Harbrow D, Vinczer E, et al. Endodontic sequelae of dental erosion. Aust Dent J. 2003;48:97-101.
11. Litonjua LA, Andreana S, Bush PJ, et al. Tooth wear: attrition, erosion, and abrasion. Quintessence Int. 2003;34:435-446.
12. Mair LH. Understanding wear in dentistry. Compend Contin Educ Dent. 1999;20:19-32.
13. Xhonga FA, Sognnaes RF, Wolcott RB. Dental erosion. I. Erosion-like patterns occurring in association with other dental conditions. Dental erosion. II. Clinical measurements of dental erosion progress. J Am Dent Assoc. 1972;84:571-576,577-582.
14. Asher C, Read MJ. Early enamel erosion in children associated with the excessive consumption of citric acid. Br Dent J. 1987;162:384-387.
15. Grando LJ, Tames DR, Cardoso AC, et al. In vitro study of enamel erosion caused by soft drinks and lemon juice in deciduous teeth analysed by stereomicroscopy and scanning electron microscopy. Caries Res. 1996;30:373-378.
16. Meurman JH, Toskala J, Nuutinen P, et al. Oral and dental manifestations in gastroesophageal reflux disease. Oral Surg Oral Med Oral Pathol. 1994;78:583-589.
17. Taylor G, Taylor S, Abrams R, et al. Dental erosion associated with asymptomatic gastroesophageal reflux. ASDC J Dent Child. 1992;59:182-185.
18. Pintado MR, Anderson GC, DeLong R, et al. Variation in tooth wear in young adults over a two-year period. J Prosthet Dent. 1997;77:313-320.
19. Molnar S, McKee JK, Molnar IM, et al. Tooth wear rates among contemporary Australian Aborigines. J Dent Res. 1983;62:562-565.
20. Lambrechts P, Braem M, Vuylsteke-Wauters M, et al. Quantitative in vivo wear of human enamel. J Dent Res. 1989;68:1752-1754.
21. Khan F, Young WG, Daley TJ. Dental erosion and bruxism. A tooth wear analysis from south east Queensland. Aust Dent J. 1998;43:117-127.
22. Strassler HE, Kihn PW, Yoon R. Conservative treatment of the worn dentition with adhesive composite resin. Contemp Esthet Restor Pract. 1999;1(4):42-52.
23. Bernardo JK, Maia EA, Cardoso AC, et al. Diagnosis and management of maxillary incisors affected by incisal wear: an interdisciplinary case report. J Esthet Restor Dent. 2002;14:331-339.
24. Ibsen RL, Ouellet DF. Restoring the worn dentition. J Esthet Dent. 1992;4:96-101.
25. Nohl FS, King PA, Harley KE, et al. Retrospective survey of resin-retained cast-metal palatal veneers for the treatment of anterior palatal tooth wear. Quintessence Int. 1997;28:7-14.
26. Cheung SP, Dimmer A. Management of the worn dentition: a further use for the resin-bonded cast metal restoration. Restorative Dent. 1988;4:76-78.
27. Stewart B. Restoration of the severely worn dentition using a systematized approach for a predictable prognosis. Int J Periodontics Restorative Dent. 1998;18:46-57.
28. Lytle JD. Clinician’s index of occlusal disease: definition, recognition, and management. Int J Periodontics Restorative Dent. 1990;10:102-123.
29. Turner KA, Missirlian DM. Restoration of the extremely worn dentition. J Prosthet Dent. 1984;52:467-474.
30. Cook DA. Using crayons to educate patients about front-tooth wear patterns. J Am Dent Assoc. 1998;129:1149-1150.
31. Christensen GJ. A new technique for restoration of worn anterior teeth—1995. J Am Dent Assoc. 1995;126:1543-1546.
32. Hemmings KW, Darbar UR, Vaughan S. Tooth wear treated with direct composite restorations at an increased vertical dimension: results at 30 months. J Prosthet Dent. 2000;83:287-293.
33. Strassler HE. Cure depths compared with LED and other curing lights. J Dent Res. 2003;82(special issue A):80. Abstract 894.
34. Fan J, Dogariu A, Wang LJ. Amplified total internal reflection. Optics Express. 2003;11:299-308.
Dr. Strassler is professor and director of operative dentistry, department of restorative dentistry, University of Maryland Dental School. He can be reached at hes001@dental.umaryland.edu.
Dr. Serio is assistant professor, department of care planning and restorative sciences, University of Mississippi School of Dentistry. She can be reached at clserio@sod.umsmed.edu.