INTRODUCTION
Implants are already recognized as essential to enhancing a patient’s quality of life. To ensure successful integration of the oral implant in the patient’s edentulous area, implants are now being developed in all different sizes, shapes, and widths, with various grooved surfaces and designs. This facilitates prosthetic restoration and the return of function. However, to achieve successful implant integration, aesthetic enhancement must be considered as an added possibility, along with phonetic improvement, when needed.
The practitioner’s goal is for a patient to be able to enjoy improved mastication as well as to speak with confidence. The patient is not only able to avoid a denture, which would hinder speaking and masticatory functions, but after successful oral implant integration, the patient also has a more youthful appearance and the potential for a new outlook on life.
The success of oral implants depends on the acceptance of the implant and its integration with the bone. Certain considerations of the implant surgical site must first be made. Key questions include whether the bone of the implant surgical site can be optimized to ensure predictable integration and whether there is enough bone to support an implant. Another important question is whether there is enough bone to support and ensure predictable integration. Extractions are a major concern today.
After extraction, will there be enough bone to support the endosseous implant and its prosthetic restoration? Currently, it is generally accepted and advised to extract sooner rather than later as there is more bone available to support an implant. By waiting too long to extract, you risk ending up with less than the desired amount of bone. The more bone that is available, the more the implant surface contacts bone and, with all of today’s designs, the more predictable the osseous integration and success are.
This article emphasizes the preservation of the osseous walls of the extraction site during surgical extraction. There are now new proper surgical instruments with which the practitioner can, without strain or unnecessary physiologic positions, access and luxate in mesial and distal directions and remove the roots while preserving both the buccal and lingual walls of the osseous socket. This enables the retention of the existing blood supply, which will guide and aid the osseous regeneration of the future ideal osseous implant site.
In the history of dental extractions, removing the debilitated tooth out of the oral cavity as rapidly and as painlessly as possible has always been paramount. Based on the concept that the buccal bone is usually the thinnest zone of bone that retains the tooth and that it provides the least resistance, it is common practice after anesthesia to luxate in a bucco-lingual movement. Anatomically, the buccal plate of bone is usually much thinner than the palatal or lingual osseous plates.
However, this article will show that this method will not meet with optimal success. The easier extraction toward the buccal will actually result in the loss of more buccal bone. This is because healing depends on the available blood supply, primarily from the osseous walls of the extraction site. The constant pressure from the buccal-lingual luxation leads to ischemia in the remaining thin plate of buccal bone. The ischemia leads to further resorption and, therefore, the loss of buccal bone.
Upon healing, the area will have a depression in the buccal plate and occlusal resorption.
Problems resulting from the healed buccal depression include a buccal void, leading to poor oral hygiene, food retention, and an unaesthetic appearance. Another possible problematic result is the incorrect placement of the implant. The implant needs to be placed in adequate osseous support to succeed.
Since the implant must be placed where bone is, the implant placement will be lingual to the original tooth being replaced. This may result in a situation requiring a prosthesis that is similar to a buccal cantilever—ie, a prosthesis that is overextended buccally to ensure correct occlusion—but this would put undue stress on the implant. During extraction, our goal should be to preserve as much bone as possible by averting bone loss, especially of the buccal osseous plate.
Mesial-distal Hoexter Luxators have been developed for use during extractions for the specific purpose of preserving as much bone as possible and have been utilized for many years. The Hoexter Luxators, distributed by Hu-Friedy, (Figure 1), are designed to be used expressly in a mesial-distal motion to avoid any buccal pressure. The design of the instruments ensures that the practitioner maintains the correct angle of mesial or distal pressure on the root to be extracted with strain-free access and visibility, thus ensuring a successful and predictable result.

Figure 1. The Hoexter Luxator series of instru- ments is designed to facilitate the removal of roots by mesial-distal movement, allowing the preservation of buccal and lingual osseous walls during an extraction while also allowing the practitioner to visualize the operating area in comfort and ease. The instruments are available in incised edges of 3 or 5 mm for various sized teeth and comfortable angulations.
The Hoexter Luxator technique relies on the concept that it is easier to extract a single-root tooth than a multi-rooted one. After applying local anesthesia, the practitioner should remove the posterior tooth’s crown horizontally at its CEJ, thereby exposing the individual roots. At this time, the Hoexter Luxator should be placed in the desired location (Figure 2) and moved with slight pressure in a mesial-distal direction. The root will become quite mobile and is easily removed.
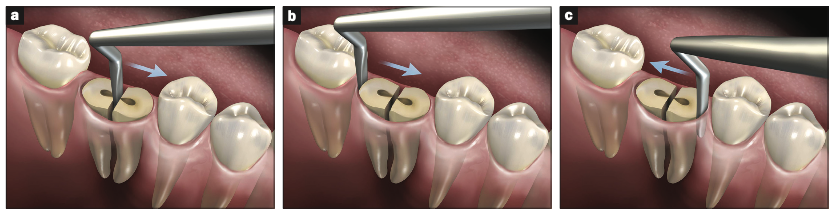
Figure 2. (a) The Hoexter Luxator in the septal area of the mandibular molar. The force is being directed toward the mesial. (b) The Hoexter Luxator placed at the distal of the mandibular molar with the force directed in a mesial direction. (c) The Hoexter Luxator placed at the mesial of the mandibular molar. The force is being directed in a distal direction. With the constant mesial-distal pressure, the root is easily made mobile and removed, thus preserving the buccal and lingual osseous walls.
There should be no pressure exerted on the buccal plate of bone during the technique. The resultant void will have its osseous walls intact. This can and will induce osseous regeneration and result in the desired healthy osseous support for the soon-to-be-inserted implant. This regenerated bone will include the buccal wall as well as the mesial, distal, and lingual and probably some interseptal bone. All the remaining osseous walls may be productive in guiding the positive regeneration of bone.
By using this technique and the Hoexter Luxator instruments, you will avoid the unhygienic buccal void; the unaesthetic, dark appearance of the buccal depression; and the resorptive depression of the buccal bone. You will also avoid the placement of an implant too lingually, which may cause future occlusal trauma. By successfully completing these steps with the Hoexter Luxator instruments, you will help to avoid bad oral hygiene and to overcome aesthetic and restorative challenges, thereby avoiding future occlusal trauma.
CASE PRESENTATION
Figures 3 to 8 demonstrate how a practitioner can remove roots while preserving both the buccal and lingual walls of the osseous socket.
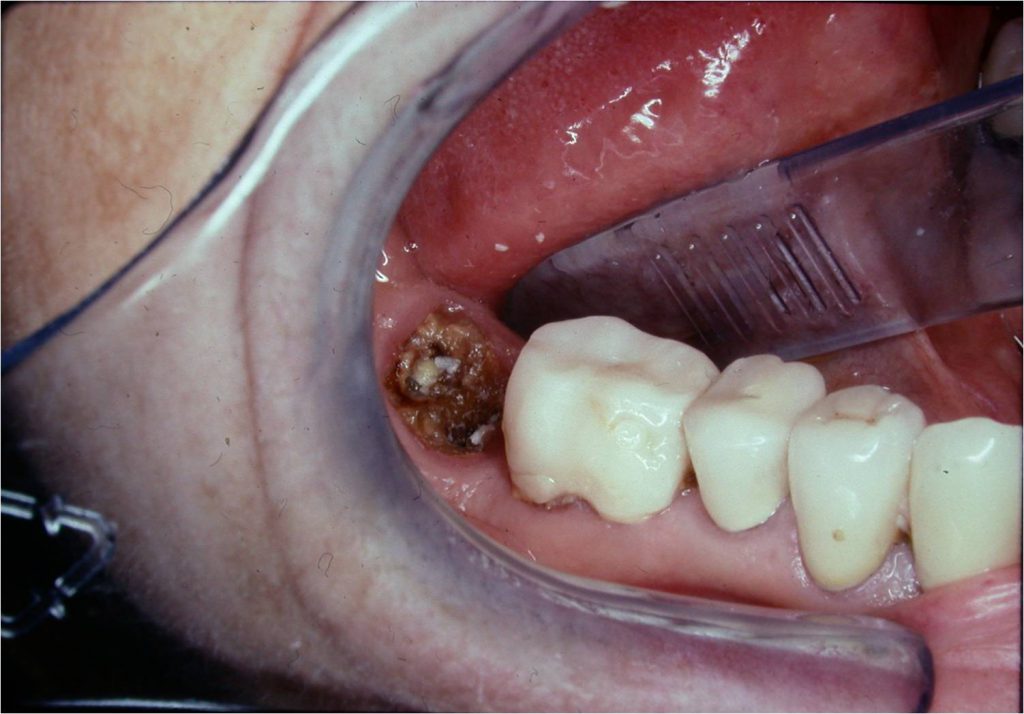
Figure 3. Tooth No. 31 (LR second molar) with the temporary crown off, showing caries and broken tooth structure.
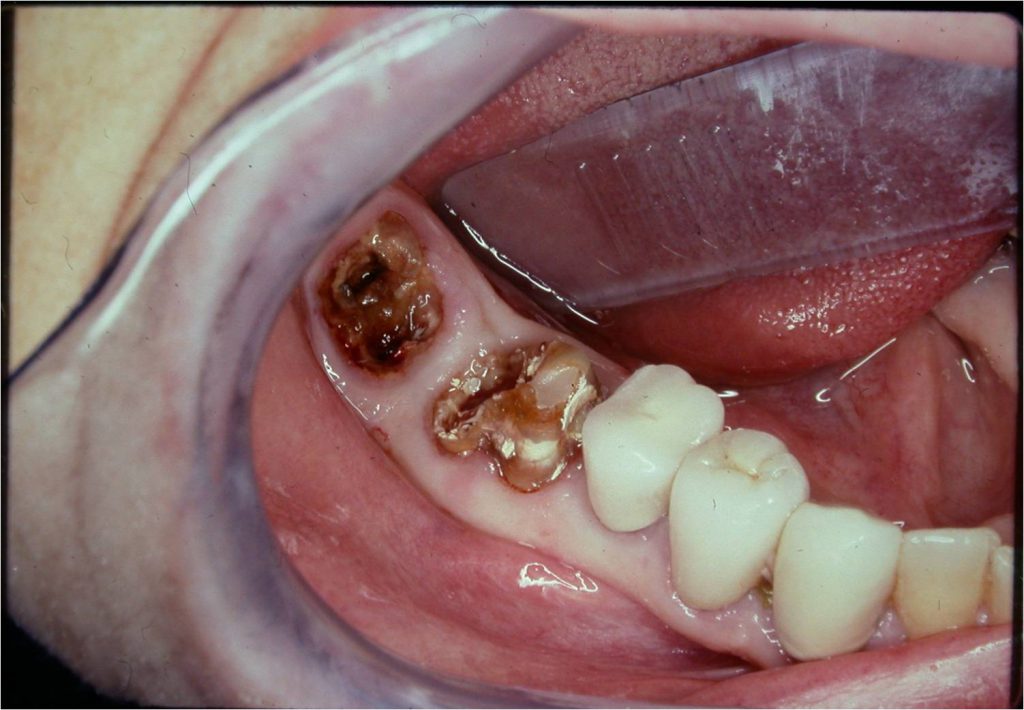
Figure 4. Tooth No. 30 with its temporary crown now off, exposing extensive caries, poor remaining tooth structure, and poor prognosis for both teeth Nos. 30 and 31.

Figure 5. Tooth No. 30 crown portion divided into 2 halves.
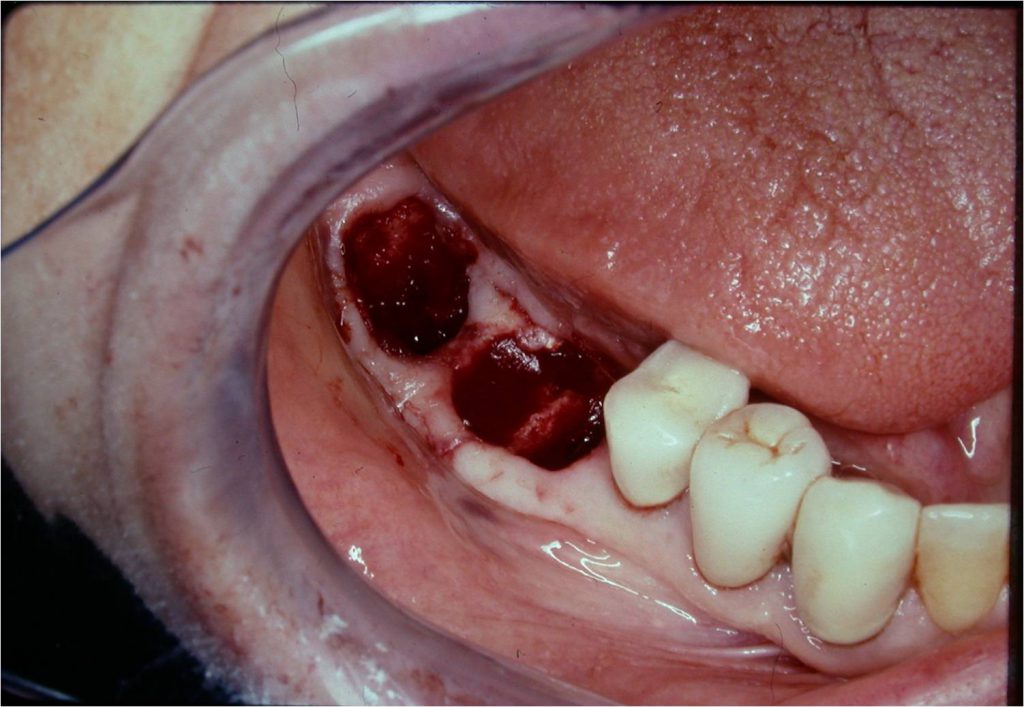
Figure 6. All 4 root sockets and even the osseous septum of tooth No. 30 were preserved by luxating mesial-distally.

Figure 7. All 4 of the roots were easily luxated out.
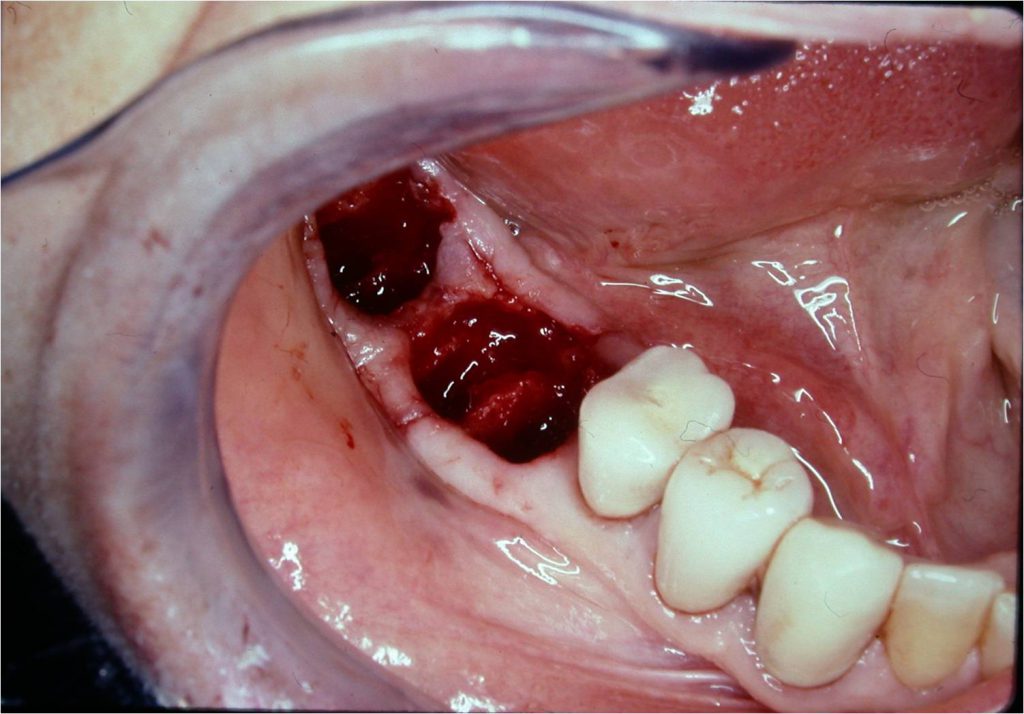
Figure 8. Blood clots seen in the No. 30 and 31 sockets.
After the extraction, I recommend the utilization of guided bone regeneration (GBR). After the removal of the individual roots with the mesial-distal luxation described, leaving the intact osseous walls where the removed roots were, I strongly advise you to use an osseous regenerative bone graft material (Figures 9 and 10) to fill the described void. Following the bone graft, I place a covering of an absorbable barrier. It is sutured, covering the void-filled osseous graft as a GBR technique.
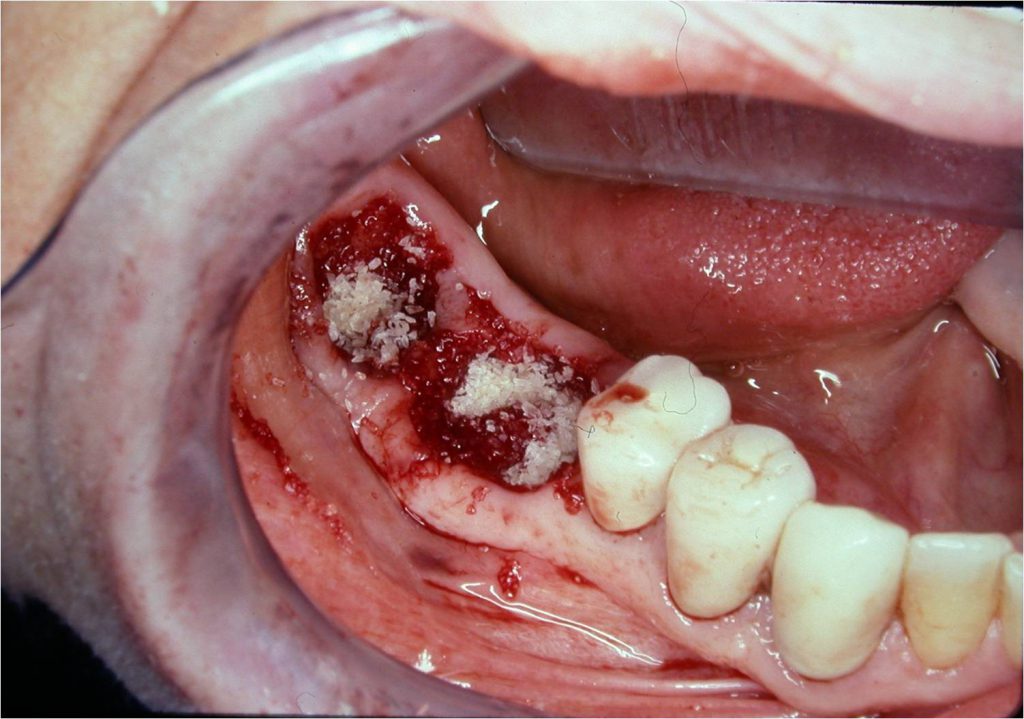
Figure 9. Osseous graft material was inserted into the sockets of both Nos. 30 and 31.
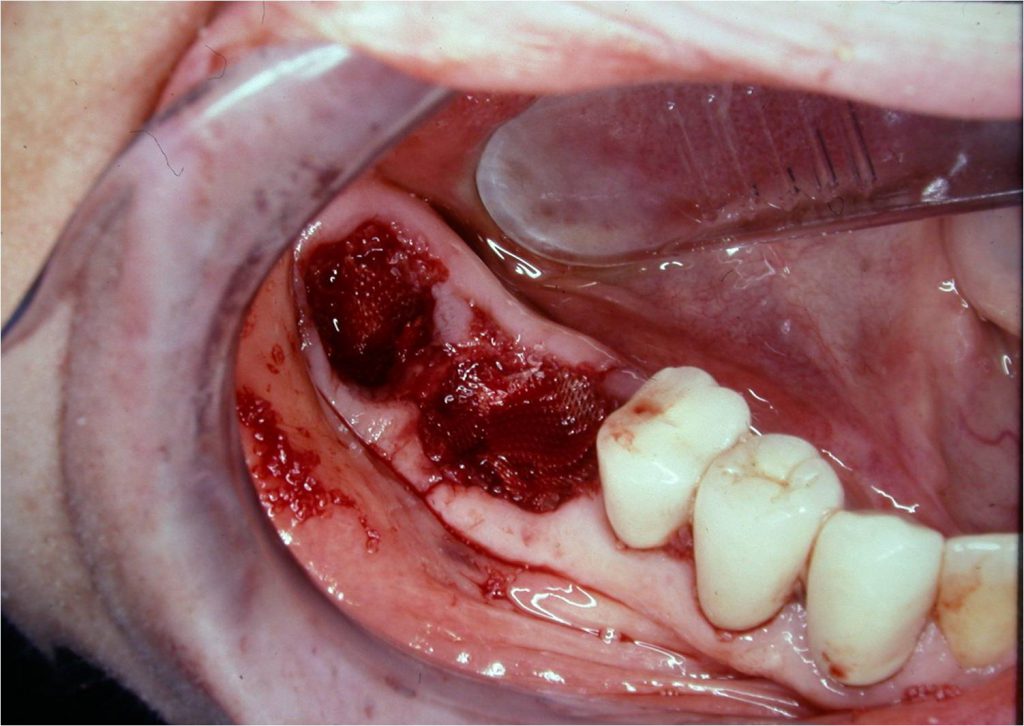
Figure 10. An absorbable membrane was placed over the grafts, such as in a GBR technique, before suturing.
After the correct time for healing (Figure 11), bone regeneration will result in a supported endosseous implant being placed in its correct position (Figures 12 and 13).

Figure 11. The lower right healed area at 3 months postoperatively.
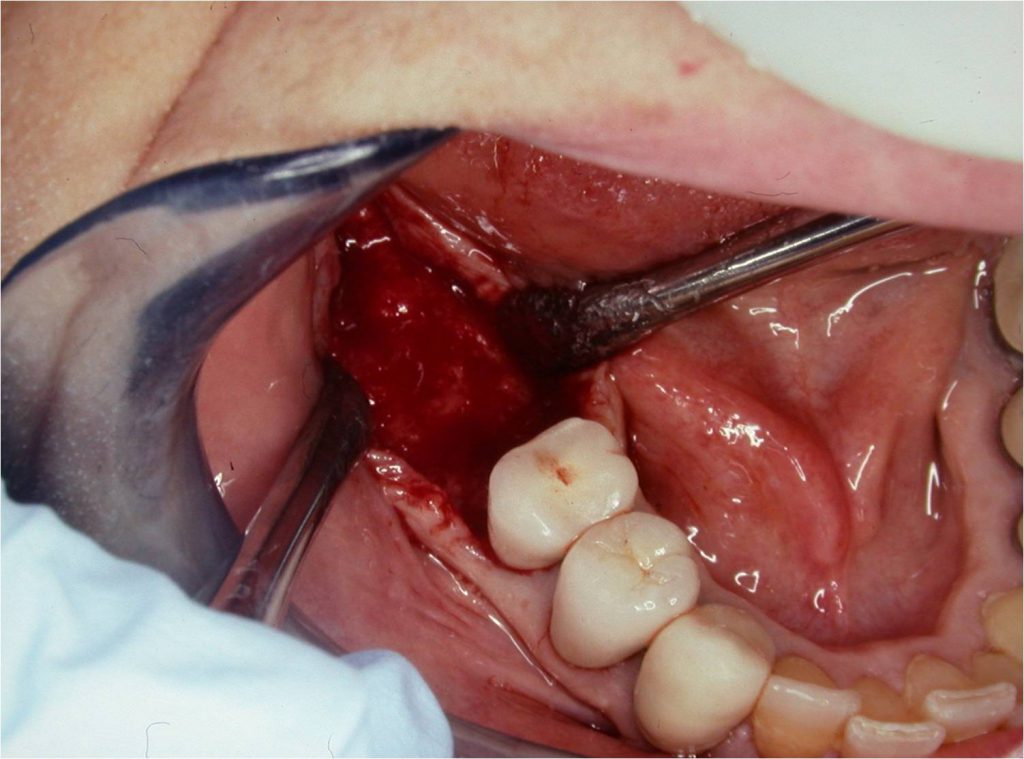
Figure 12. Exposed regenerated bone area 3 months later. Note the full ridge of bone regenerated buccal-lingually as well as mesial-distally.
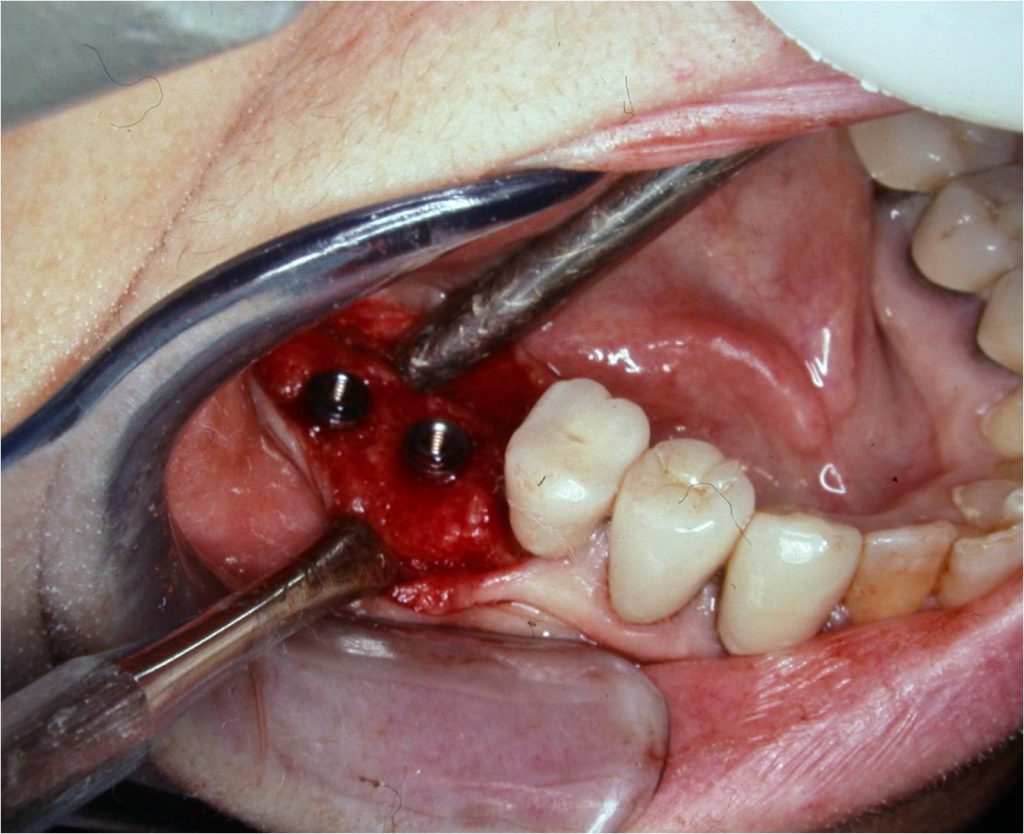
Figure 13. Implants inserted at bone level in the No. 30 and 31 positions.
The practitioner at the proper time will then be able to provide the optimal prosthetic replacement—a physiological one—in occlusal harmony: one that is physiologically shaped for the best function as well as aesthetically pleasing and easy to maintain.
The required period of time is allowed for the bone to mature and allowing osseous integration with the implant (Figures 14 and 15).
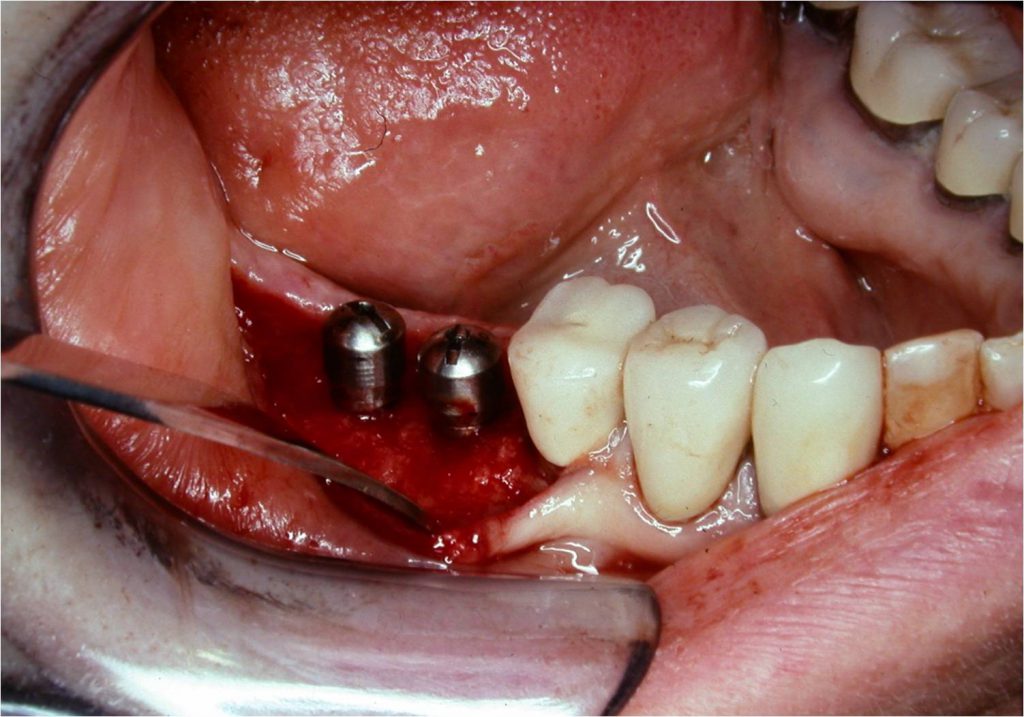
Figure 14. Implant healing abutments in place.

Figure 15. The keratinized area of the mucogingival flap was sutured at the correct level.
Changing the temporary healing abutment to a permanent abutment is sequential. This author prefers the utilization of a custom-made abutment, followed by an aesthetically pleasing, occlusally and physiologically functioning prosthesis (Figures 16 and 17). The surrounding keratinized gingival tissue will allow the patient to maintain his or her oral hygiene with more ease, thus allowing predictability of maintaining this desired result.

Figure 16. Buccal view of the completed, restored prosthesis with healthy keratinized tissue.

Figure 17. Lingual view of the restored prosthesis with healthy keratinized tissue.
ABOUT THE AUTHOR
Dr. Hoexter received his DMD degree from Tufts University in Boston. He is director of the International Academy for Dental Facial Aesthetics and a Diplomate of Implantology in the International Congress of Oral Implantologists and the American Society of Osseointegration. He is a Diplomate of Dental Aesthetics from the American Board of Aesthetic Dentistry. He has been awarded 13 Fellowships and practiced in New York City, limited to periodontics, implantology, and cosmetic periodontal surgery.
He is also a clinical professor in the periodontal and implant department at Temple University in Philadelphia. He was previously a clinical professor in periodontics at the University of Pittsburgh. Dr. Hoexter lectures throughout the world and has been published extensively both nationally and internationally. He can be reached at drdavidlh@gmail.com.
Disclosure: Dr. Hoexter has a financial arrangement with Hu-Friedy, the manufacturer and distributor of Hoexter Luxators.












