INTRODUCTION
The discipline of implant dentistry has grown dramatically over several decades because predictable outcomes have been demonstrated. Successful outcomes have been exhibited in the areas of osseointegration and aesthetics. The conventional, delayed implant approach was based on a stress-free period to establish integration.1 Immediate implant placement and provisionalization (IIPP) is a minimally invasive approach that combines several implant principles to reduce treatment times and eliminate removable partial dentures.2
Clinicians agree that challenges exist in attempting to achieve ideal aesthetics.3 Knowledge of hard- and soft-tissue responses to surgery and restorative procedures as well as materials is critical in obtaining ideal results.4 Clinical research has demonstrated high success rates with the IIPP approach regarding osseointegration.5,6 Furthermore, aesthetics are enhanced because less bone loss and recession are exhibited. Some studies have demonstrated bone gain when IIPP protocols are employed.7
The IIPP approach encompasses a single surgery, including tooth extraction and implant placement with a transmucosal provisional abutment and a crown.8,9 In addition, a final fixture-level impression and guided bone regeneration (GBR) are incorporated in the initial stage of treatment.10 The final restoration is placed after osseointegration is complete.
The specific GBR protocol of IIPP is dependent on the type of tooth socket that exists post-extraction. Elian et al11 described 3 types of sockets based on the presence of soft tissue and the facial plate of bone. A buccal plate deficiency with ideal soft tissue is categorized as a Type II socket. This condition warrants a collagen barrier incorporated into the GBR technique.
This paper discusses the clinical management of a deficiency of the facial plate of bone. The treatment incorporated the utilization of the IIPP approach to resolve a horizontal fracture of a maxillary central incisor (tooth No. 8). Clinical research on using the IIPP approach to treat Type II sockets is limited.
CASE REPORT
A 30-year-old male presented to our office after a traumatic incident to the mouth. His chief complaint was, “I was punched out by my old girlfriend’s new boyfriend.” The clinical and radiographic evaluation demonstrated a horizontal fracture at the gingival margin of the maxillary right central incisor (tooth No. 8) (Figure 1). The periapical radiograph exhibited a residual root without periapical radiolucency (Figure 2).

Figure 1. Horizontal fracture, right central incisor (tooth No. 8).

Figure 2. Periapical radiograph, maxillary right central incisor (tooth No. 8).
Prior to surgery, the patient was draped, prepped, and asked to rinse with a chlorhexidine mouthwash for 30 seconds. Local anesthesia (2 carpules of 2% Lidocaine [36 mg] with 1:100,000 epinephrine [Benco Dental]) was given via a buccal-palatal infiltration approach. The extraction of tooth No. 8 was initiated with a flapless intrasulcular incision with a 15c blade.
Then 301 and 34s elevator and atraumatic forceps were used to remove the tooth (Figure 3). The socket was degranulated with a doubled-ended molt curette, and the bony walls were evaluated with a periodontal probe. A 4.7- × 13-mm SBM tapered implant (Legacy 1 [Implant Direct]) was inserted with a straight driver 1 mm coronal to the final position.
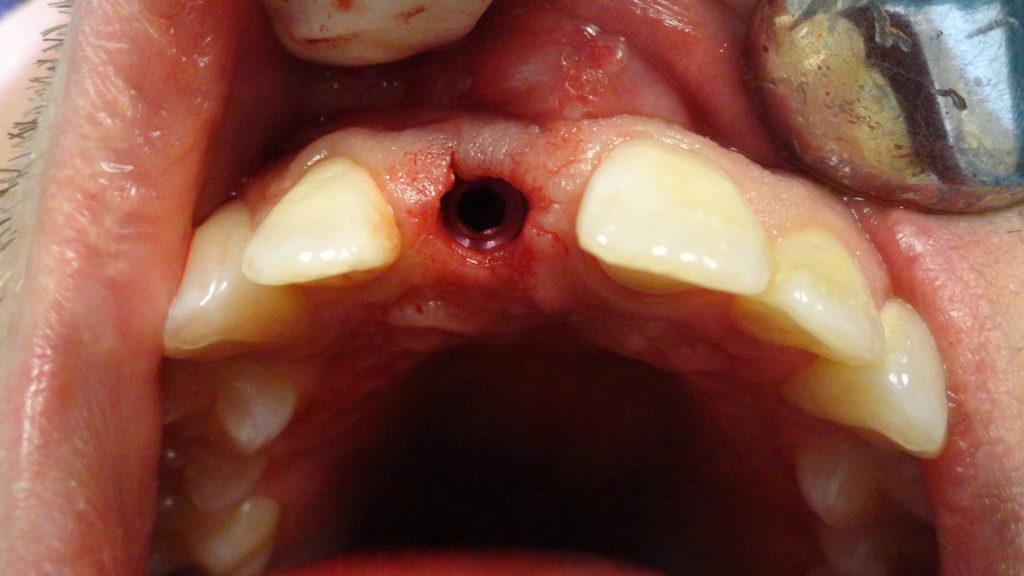
Figure 3. Tooth socket.
Torque was confirmed at a value greater than 35 mm. The implant was inserted to its final position of 4 mm apical to the ideal mid-facial gingival margin (Figure 4).

Figure 4. Fixture mount 4.7- × 13-mm SBM Legacy 1 (Implant Direct).
A fixture-level impression was taken utilizing a 4.7-mm transfer pin and polyvinyl siloxane material (Figures 5 and 6). After the impression procedure, a PEEK abutment was modified, and the retaining screw was torqued to 20 Ncm. A provisional crown was fabricated to avoid any contact in centric occlusion, protrusion, or right and left lateral excursions.

Figure 5. Periapical radiograph—transfer pin/implant.
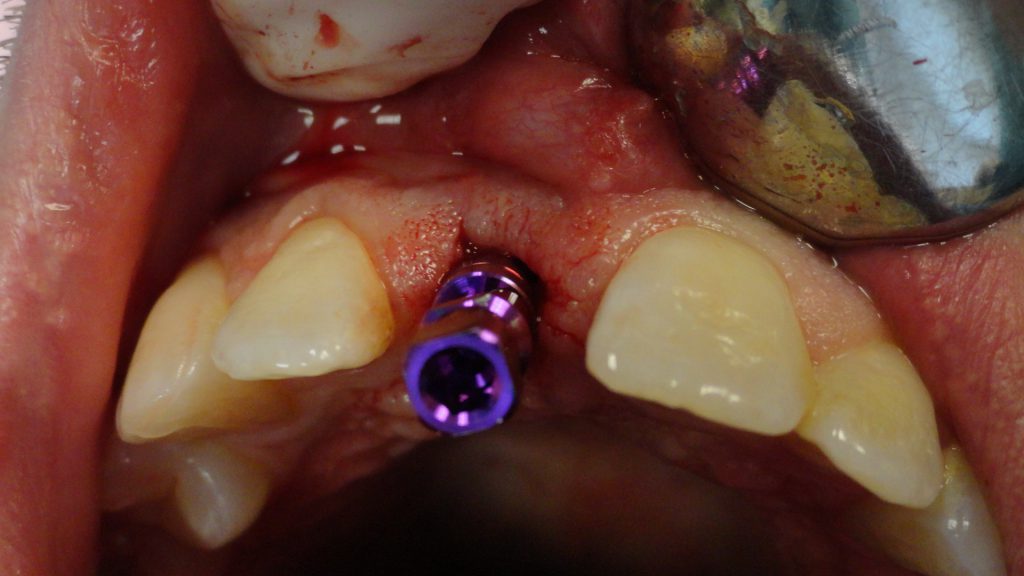
Figure 6. Impression transfer pin.
The incisal edge was made shorter than the contralateral adjacent tooth.
A restorable collagen bovine membrane (Cytoplast RTM [Implant Direct]) was positioned in the buccal aspect of the socket (Figure 7).

Figure 7. Collagen membrane.
The “gap,” which is defined as the space between the implant surface and the mucosa, was grafted with sterile saline and a cancellous, mineralized, irradiated bone allograft with a particle size of 420 to 1000 µm, (Fine [Rocky Mountain Tissue Bank]) (Figures 8 and 9).

Figure 8. Cortico-cancellous allograft.
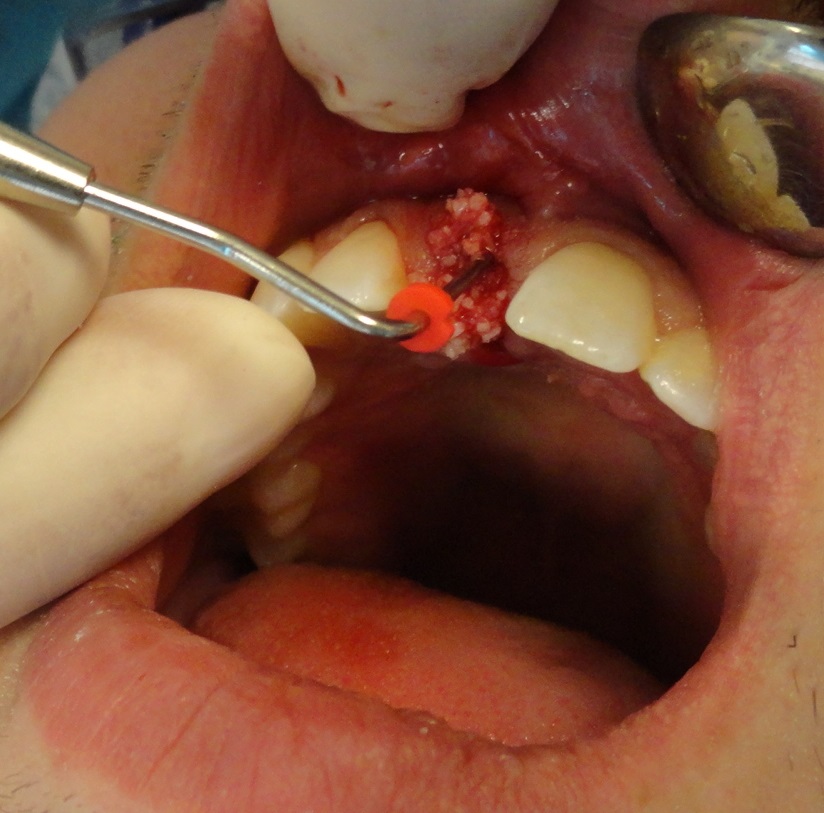
Figure 9. Bone graft plugger.
The provisional crown was placed with a permanent resin cement (RelyX [3M]) (Figure 10).

Figure 10. Provisional/crown.
After 4 months, the provisional crown and abutment were removed as a one-piece unit by creating a palatal hole with a 4-round bur to gain access to the retaining screw. A counterclockwise rotation with a torque wrench and a 1.25-mm hex tool loosened the screw.
A custom zirconia abutment was placed, and a periapical radiograph was taken to confirm an accurate fit (Figure 11). An accurate fit was not achieved, and the Zr abutment was removed. Local anesthesia (one carpule of 2% Lidocaine [18 mg] with 1:100,000 epinephrine) was administered in a buccal and palatal infiltration manner.
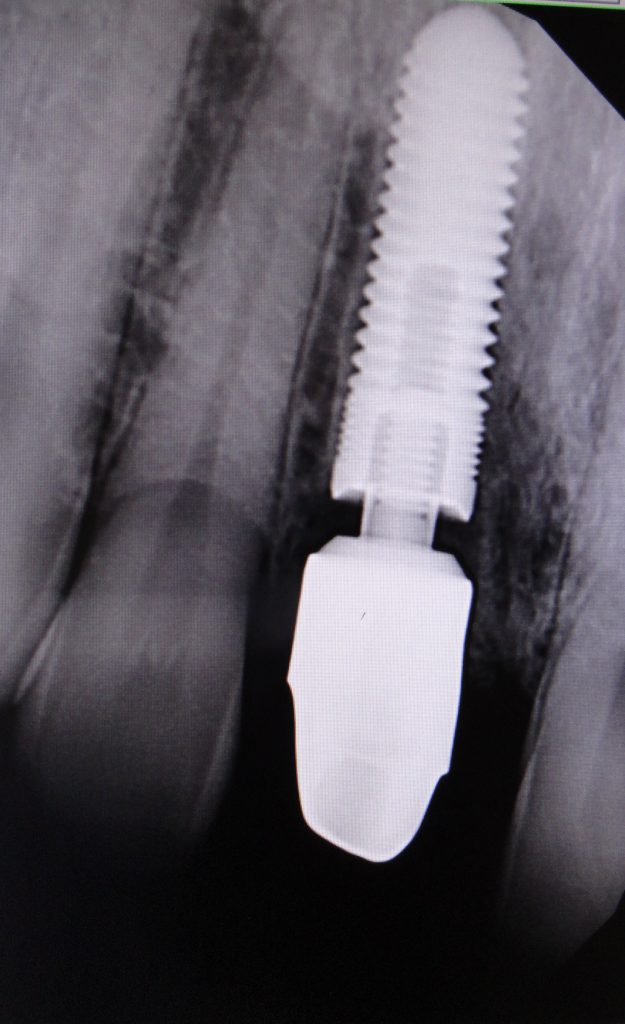
Figure 11. Zr Abutment, not seated.
A 15c blade and a double-ended molt curette were utilized to incise and debride the hyperplastic sulcular tissues. The abutment was reseated, and a periapical radiograph was taken to confirm an intimate fit between the Zr abutment and the implant platform (Figures 12 and 13). The retaining screw was torqued to 30 Ncm 2 times in a 10-minute interval.
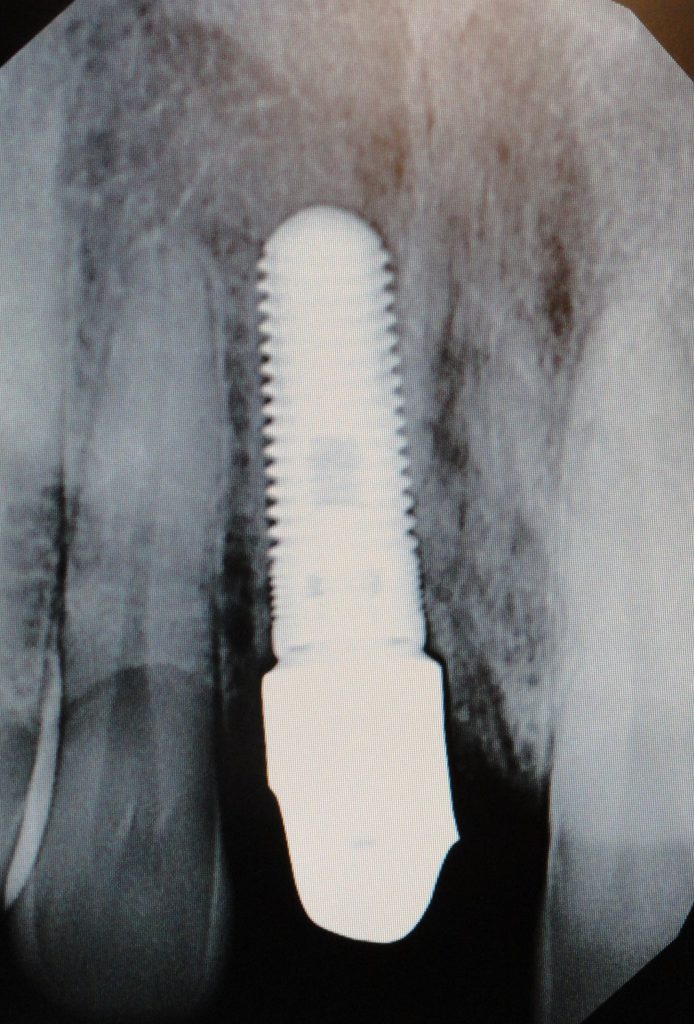
Figure 12. Zr Abutment seated.

Figure 13. Zr Abutment.
The final all-ceramic crown (IPS e.Max [Ivoclar Vivadent]) was placed using an adhesive resin cement (Figure 14).

Figure 14. Final prosthesis, all-ceramic crown/facial view.
DISCUSSION
The IIPP approach deviates from the conventional delayed concept where a stress-free loading period exists for 3 to 6 months.12 The IIPP GBR protocols are based on the degree of hard and soft tissue present after removal of the hopeless tooth. When a hard-tissue deficiency exists, surgical management is more complex, and the aesthetic outcomes are less predictable.13
Flapless, atraumatic extraction techniques are employed to minimize the disruption of the blood supply to the facial plate of bone. Studies have demonstrated that the periosteum is the major source of blood supply to the facial bone plate.14 Elevation of a flap disrupts blood flow for several days.15 Inspecting the bone socket to confirm the presence of the facial plate of bone is essential in determining the surgical technique to be employed.
A torque value greater than 35 Ncm is a key determinant in deciding whether to incorporate the immediate provisional aspect of IIPP.16,17 If it is not achieved, a healing collar and a removable partial denture are employed.
A provisional abutment and crown are fabricated to develop soft-tissue contours, prevent graft loss and protect the blood clot. Studies indicate that greater mid-facial recession is demonstrated when a healing collar is used vs a provisional crown. The temporary abutment screw is torqued to 20 Ncm to prevent screw loosening. During the osseointegration stage, the crown adheres to the abutment with a permanent resin cement.18 The author reports that the most common complication to the IIPP approach was screw loosening of the temporary abutment and decementation of the provisional crown. These complications can be minimized by torquing the retaining screw to 20 Ncm and cementing the provisional crown with a resin cement.
The Type II socket demonstrates ideal soft-tissue contours with a deficiency of the facial plate of bone. A resorbable barrier is placed within the facial aspect of the socket to exclude soft-tissue cells from migrating onto the implant surface, facilitating bone regeneration.19 Autogenous and allographic bone graft materials can be used to manage the gap between the mucosa and the implant surface.20,21 IIPP management of the Type II socket is based on the ice cream cone technique. That study utilized a xenograft and collagen barrier exhibiting a facial net bone gain of 1.32 mm.22 Autogenous bone grafting has been described as exhibiting 100% implant survival rates with stable mid-facial bone height.23,24
Research by Sarnachiaro et al25 utilizing a flapless extraction technique, implant placement, a custom temporary abutment, allograft, and a resorbable barrier demonstrated an average facial bone plate net gain of 2.00 mm. This case report utilized a mineralized irradiated cancellous bone allograft obtained from the vertebral column.26 Allografts share similar properties with autogenous bone, such as osteoinduction and osteoconduction, without increased morbidity.
Allografts have demonstrated bone morphogenic proteins while maintaining space via a scaffold design to enhance bone formation.27,28 Further studies suggest that graft materials placed coronal to the abutment-implant connection increase soft-tissue thickness and reduce the need for additional surgery.29,30
Restorative materials selected, designed, and utilized affect the aesthetic outcome.31 All restorative materials create a color change in the mucosa.32 Titanium requires 3 mm of soft tissue to be masked, and 1 mm of mucosal thickness visually hides no restorative materials.33 Zirconia minimizes that color change when tissue thickness is greater than 2 mm. Zirconia exhibits biocompatibility, minimizes color alteration, and reduces recession.34
It is important to confirm an accurate component fit between the abutment and fixture platform. Soft and hard tissue may impede the accurate seating of component parts. This will alter short- and long-term outcomes, including occlusal and mechanical complications. A periapical radiograph is recommended to confirm the fit of restorative parts. Implant occlusal principles applied to the final restoration consist of no contact in centric occlusion, excursions, or protrusion.
A contact is achieved during maximum occlusal contact. The mid-facial gingival contour of the final restoration is undercontoured to facilitate a soft-tissue passive drape.35
ACKNOWLEDGEMENTS
The author wishes to acknowledge LeeAnn Klotz, DA; Tatyanna Lybezhamina, DA, and Anna Jackson, BS, MA, for their assistance in the preparation of this paper.
REFERENCES
1. Albrektsson T, Brånemark PI, Hansson HA, et al. Osseointegrated titanium implants. Requirements for ensuring a long-lasting, direct bone-to-implant anchorage in man. Acta Orthop Scand. 1981;52(2):155–70. doi:10.3109/17453678108991776
2. Lazzara RJ. Immediate implant placement into extraction sites: surgical and restorative advantages. Int J Periodontics Restorative Dent. 1989;9(5):332–43.
3. Kan JY, Rungcharassaeng K, Lozada J. Immediate placement and provisionalization of maxillary anterior single implants: 1-year prospective study. Int J Oral Maxillofac Implants. 2003;18(1):31–9.
4. Kois JC. Predictable single-tooth peri-implant esthetics: five diagnostic keys. Compend Contin Educ Dent. 2004;25(11):895–6, 898, 900 passim; quiz 906–7.
5. Hui E, Chow J, Li D, et al. Immediate provisional for single-tooth implant replacement with Brånemark system: preliminary report. Clin Implant Dent Relat Res. 2001;3(2):79-86. doi:10.1111/j.1708-8208.2001.tb00235.x
6. Wöhrle PS. Single-tooth replacement in the aesthetic zone with immediate provisionalization: fourteen consecutive case reports. Pract Periodontics Aesthet Dent. 1998;10(9):1107–14; quiz 1116.
7. Norton MR. A short-term clinical evaluation of immediately restored maxillary TiOblast single-tooth implants. Int J Oral Maxillofac Implants. 2004;19(2):274–81.
8. Barzilay I, Graser G, Cantron J, et al. Immediate implantation of pure titanium threaded implants into extraction sockets. J Dent Res. 1988;67:234.
9. Schropp L, Isidor F, Kostopoulos L, et al. Patient experience of, and satisfaction with, delayed-immediate vs. delayed single-tooth implant placement. Clin Oral Implants Res. 2004;15(4):498-503. doi:10.1111/j.1600-0501.2004.01033.x
10. Jackson BJ. Immediate implant placement and provisionalization case report. NYSAGD. 2017;12–6.
11. Elian N, Cho SC, Froum S, et al. A simplified socket classification and repair technique. Pract Proced Aesthet Dent. 2007;19(2):99-104; quiz 106.
12. Lang NP, Pun L, Lau KY, et al. A systematic review on survival and success rates of implants placed immediately into fresh extraction sockets after at least 1 year. Clin Oral Implants Res. 2012;23 Suppl 5:39-66. doi:10.1111/j.1600-0501.2011.02372.x
13. Kamperos G, Zambara I, Petsinis V, et al. The impact of buccal bone defects and immediate placement on the esthetic outcome of maxillary anterior single-tooth implants. J Oral Implantol. 2016;42(4):337–41. doi:10.1563/aaid-joi-D-16-00004
14. Brägger U, Pasquali L, Kornman KS. Remodelling of interdental alveolar bone after periodontal flap procedures assessed by means of computer-assisted densitometric image analysis (CADIA). J Clin Periodontol. 1988;15(9):558–64. doi:10.1111/j.1600-051x.1988.tb02129.x
15. Cutright DE. The proliferation of blood vessels in gingival wounds. J Periodontol. 1969;40(3):137–41. doi:10.1902/jop.1969.40.3.137
16. Javed F, Romanos GE. The role of primary stability for successful immediate loading of dental implants. A literature review. J Dent. 2010;38(8):612–20. doi:10.1016/j.jdent.2010.05.013
17. Dilek O, Tezulas E, Dincel M. Required minimum primary stability and torque values for immediate loading of mini dental implants: an experimental study in nonviable bovine femoral bone. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105(2):e20-7. doi:10.1016/j.tripleo.2007.10.003
18. Testori T, Bianchi F, Del Fabbro M, et al. Immediate non-occlusal loading vs. early loading in partially edentulous patients. Pract Proced Aesthet Dent. 2003;15(10):787–94; quiz 796.
19. Wilson TG Jr, Schenk R, Buser D, et al. Implants placed in immediate extraction sites: a report of histologic and histometric analyses of human biopsies. Int J Oral Maxillofac Implants. 1998;13(3):333–41.
20. Corbella S, Taschieri S, Samaranayake L, et al. Implant treatment choice after extraction of a vertically fractured tooth. A proposal for a clinical classification of bony defects based on a systematic review of literature. Clin Oral Implants Res. 2014;25(8):946–56. doi:10.1111/clr.12164
21. Jackson BJ. Proposed treatment approach for type II sockets: report of two cases. J Oral Implantol. 2019;45(3):227–34. doi:10.1563/aaid-joi-D-18-00148.
22.Araújo MG, Linder E, Lindhe J. Bio-Oss collagen in the buccal gap at immediate implants: a 6-month study in the dog. Clin Oral Implants Res. 2011;22(1):1-8. doi:10.1111/j.1600-0501.2010.01920.x
23. da Rosa JC, Rosa AC, da Rosa DM, et al. Immediate dentoalveolar restoration of compromised sockets: a novel technique. Eur J Esthet Dent. 2013;8(3):432–43.
24. Noelken R, Kunkel M, Wagner W. Immediate implant placement and provisionalization after long-axis root fracture and complete loss of the facial bony lamella. Int J Periodontics Restorative Dent. 2011;31(2):175–83.
25. Sarnachiaro GO, Chu SJ, Sarnachiaro E, et al. Immediate implant placement into extraction sockets with labial plate dehiscence defects: a clinical case series. Clin Implant Dent Relat Res. 2016;18(4):821–9. doi:10.1111/cid.12347
26. Amstutz HC, Sissons HA. The structure of the vertebral spongiosa. J Bone Joint Surg Br. 1969;51(3):540–50.
27. Elsharkawy AT, Sharaqy M, Beheiry MG, et al. Autologous versus allogenic bone blocks for augmentation of maxillary deficiency. Egypt Dent J. 2013;59:4117–21
28. Bagoff R, Mamidwar S, Chesnoiu-Matei I, et al. Socket preservation and sinus augmentation using a medical grade calcium sulfate hemihydrate and mineralized irradiated cancellous bone allograft composite. J Oral Implantol. 2013;39(3):363–71. doi:10.1563/AAID-JOI-D-10-00178
29. Chu SJ, Salama MA, Salama H, et al. The dual-zone therapeutic concept of managing immediate implant placement and provisional restoration in anterior extraction sockets. Compend Contin Educ Dent. 2012;33(7):524–32, 534.
30. Rungcharassaeng K, Kan JY, Yoshino S, et al. Immediate implant placement and provisionalization with and without a connective tissue graft: an analysis of facial gingival tissue thickness. Int J Periodontics Restorative Dent. 2012;32(6):657–63.
31. Gapski R, Wang HL, Mascarenhas P, et al. Critical review of immediate implant loading. Clin Oral Implants Res. 2003;14(5):515–27. doi:10.1034/j.1600-0501.2003.00950.x
32. Linkevicius T, Vaitelis J. The effect of zirconia or titanium as abutment material on soft peri-implant tissues: a systematic review and meta-analysis. Clin Oral Implants Res. 2015;26 Suppl 11:139–47. doi:10.1111/clr.12631
33. Jung RE, Sailer I, Hämmerle CH, et al. In vitro color changes of soft tissues caused by restorative materials. Int J Periodontics Restorative Dent. 2007;27(3):251–7.
34. Rompen E, Touati B, Van Dooren E. Factors influencing marginal tissue remodeling around implants. Pract Proced Aesthet Dent. 2003;15(10):754–7, 759, 761.
35. Misch CE. Chapter 31: Occlusal considerations for implant supported prosthesis. In: Misch CE, ed. Contemporary Implant Dentistry. Mosby;1993:705–33.
ABOUT THE AUTHOR
Dr. Jackson is an implant surgeon and a reconstructive dentist who has been surgically placing and restoring dental implants for more than 25 years. He received his DDS degree at University of Buffalo School of Dental Medicine and completed a general practice residency at St. Luke’s Memorial Hospital in Utica, NY.
Dr. Jackson completed his formal oral implantology training at the New York University College of Dentistry. Dr. Jackson is a Diplomate of the American Board of Oral Implantology/Implant Dentistry and an Honored Fellow of the American Academy of Implant Dentistry (AAID).
Dr. Jackson has been published in peer-reviewed dental journals and has presented at numerous implant conferences around the world. He is the director of the Boston MaxiCourse in Oral Implantology. Currently, Dr. Jackson serves on the editorial board for the Journal of Oral Implantology and is the President of the AAID. He can be reached at bjjddsimplant@icloud.com.
Disclosure: The author reports no disclosures.












