INTRODUCTION
Implant dentistry has become a discipline in health care to reconstruct lost soft and hard tissues to facilitate dental rehabilitation. Endosseous implants demonstrate high success rates when placed in an adequate volume of bone.1 Bone resorption is a common sequel after the loss of a tooth.2 Tooth loss is a result of caries, trauma, periodontal disease, perio-endo lesions, or congenitally missing teeth. Several approaches to managing alveolar ridge deficiency have been described, including ridge expansion, guided bone regeneration (GBR), and autogenous and allogenic block grafting.3-5
Autogenous block grafts are considered the gold standard approach for bone grafting because they provide osteogenic, osteoinductive, and osteoconductive properties.6 This source of bone can be procured from intraoral sites, such as the mandibular symphysis, ramus, or maxillary tuberosity. Extraoral sites can be utilized for larger recipient areas harvested from the iliac crest, calvarium, or tibia. The limitations of autogenous block grafting are morbidity, limited quantities, resorption potential, and a high skill level needed by the clinician.7
Allographic block grafting has gained wide acceptance because of reduced morbidity and unlimited availability if a large quantity of bone is needed.8 Allogenic grafts may be utilized in a particulate or block form, depending on the nature of the surgical objective. There is evidence of high success rates of graft integration with minimal resorption. In addition, implants placed into allogenic bone have demonstrated high survival rates.9,10
This case report discusses the management of a congenitally missing maxillary lateral incisor with a horizontal alveolar ridge deficiency. A staged approach encompassing an allogenic block graft followed by implant placement and prosthetic reconstruction was employed. This technique is for consideration for horizontal ridge augmentation for dental implant reconstruction.
CASE REPORT
A 21-year-old female patient presented to my office with an edentulous space associated with the maxillary right lateral incisor (tooth No. 7). The patient’s history revealed that the tooth was congenitally missing, and orthodontic therapy was completed 10 years ago. The medical history revealed no significant findings except for the daily intake of the medication Escitalopram (Lexapro) to manage episodes of depression. The clinical and radiographic examination revealed a Class I occlusion, adequate keratinized gingiva, and a deficiency in the buccal-palatal alveolar ridge (Figures 1 to 3). A diagnosis of horizontal ridge atrophy was made. The agreed-upon treatment plan was endosseous implant therapy post allogenic block grafting in a staged approach.
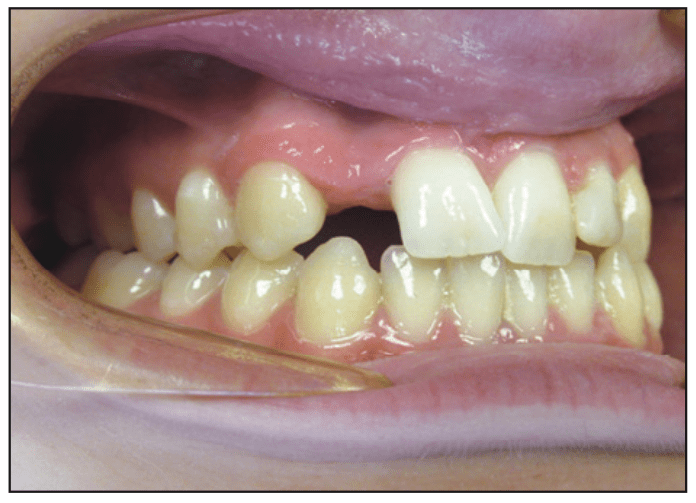
Figure 1. Presurgical site, maxillary right lateral incisor (tooth No. 7).
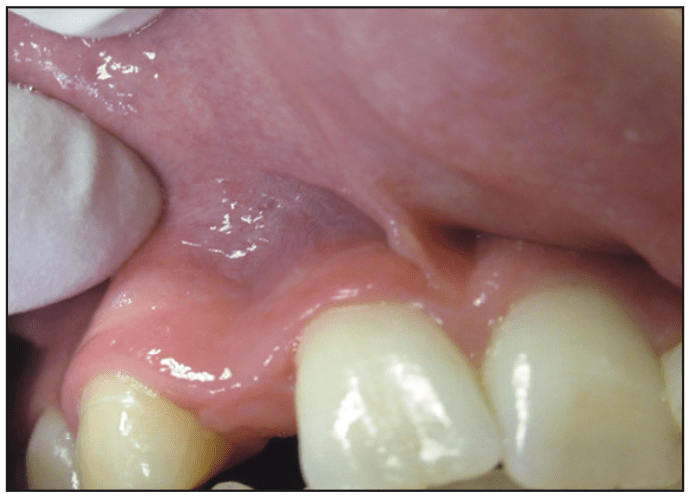
Figure 2. Buccal-palatal deficiency.
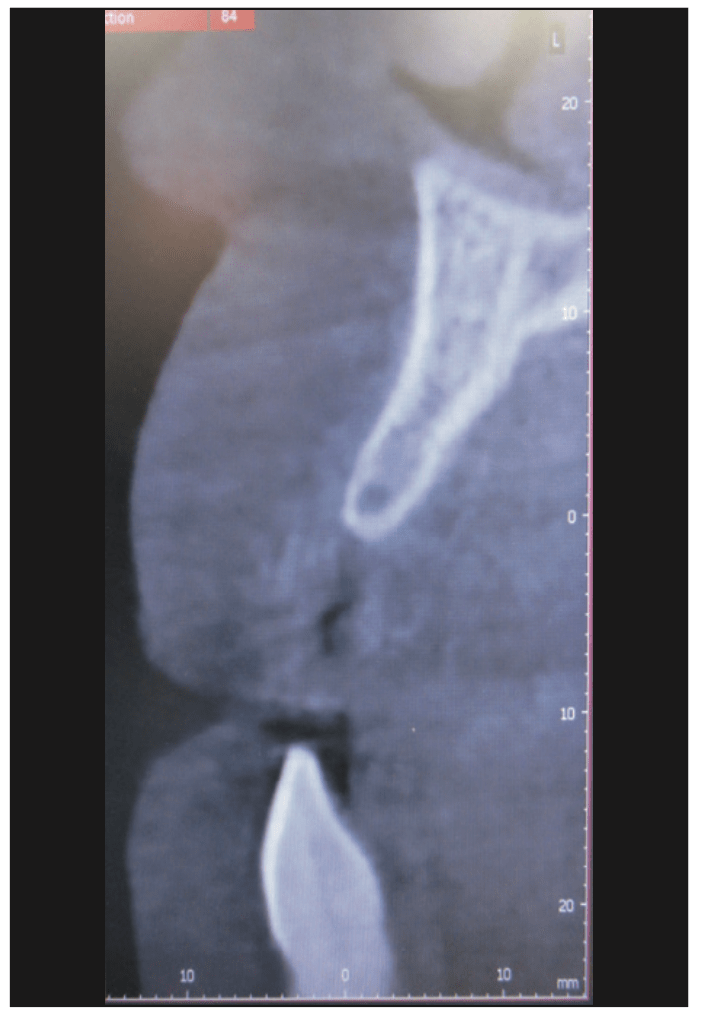
Figure 3. CBCT image, section view.
The surgical phase was initiated with a 20-mL blood draw from the median cubital vein to develop platelet-rich fibrin (PRF) and buffy coat platelet-rich plasma (BC-PRP). BC-PRP and PRF were produced with a single-spin centrifuge at 3,100 rpm for 12 minutes and processed. Local anesthesia—one carpule 3% Polocaine (54 mg) without epinephrine and one carpule 2% Lidocaine (36 mg) with epinephrine (Benco Dental)—was administrated in an infiltration manner. A full mucoperiosteal flap was raised after a midcrestal and intrasulcular incision design was made with a 15C Bard Parker blade (Figure 4). Vertical releasing incisions were made, including in the dental papilla one tooth mesial and distal to the surgical site. Collagen and elastin fibers were released and separated utilizing the dull side of a 15C blade in a back-action sweeping technique.
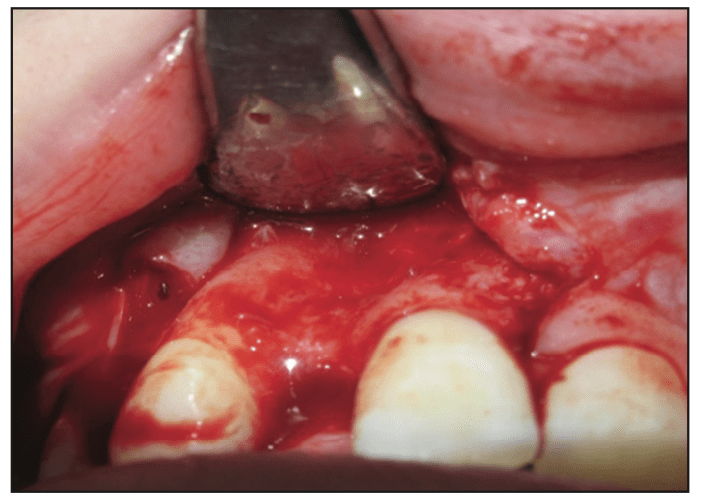
Figure 4. Full mucoperiosteal flap.
The recipient site was prepped with a 700 XL bur in an attempt to create a positive seat for the block graft. Perforations utilizing a No. 4 round bur on the alveolar ridge to promote bleeding points were made. A 10- × 10- × 5-mm corticocancellous allogenic block graft (Rocky Mountain Tissue Bank) was secured by placing a 1.5- × 10-mm machined TriStar Bone Graft Fixation System (IMPLADENT LTD) through the graft and into the palatal bone (Figure 5). After fixation was confirmed, the bony edges were rounded with a No. 6 round bur.
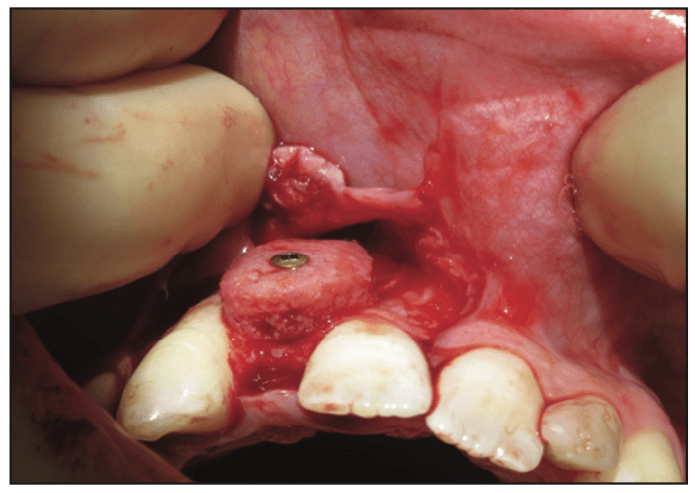
Figure 5. Allogenic block with fixation screw.

Figure 6. Collagen membrane.
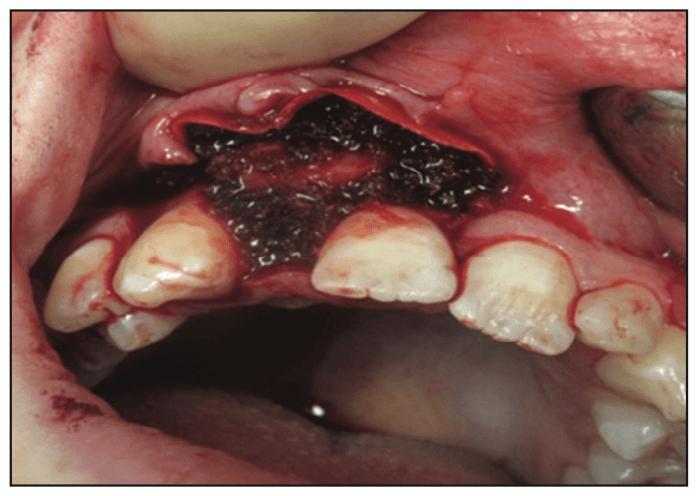
Figure 7. Particulate allographic (particulate mineralized irradiated bone) and platelet-rich fibrin.
Particulate mineralized irradiated bone (MIRB) cancellous allograph (Fine [Rocky Mountain Tissue Bank]) was mixed with PRP and mortised into all voids existing between the block and host site. The entire graft was covered with PRF and a type 1 collagen resorbable membrane (OSSix Plus [OraPharma]) (Figures 6 and 7). A fixed transitional appliance (Essix) was placed. The flap was closed, consisting of a dual technique encompassing a horizontal mattress and interrupted 3.0 d-PTFE sutures (Figure 8). A 4-month healing period prior to implant surgery was established (Figure 9).
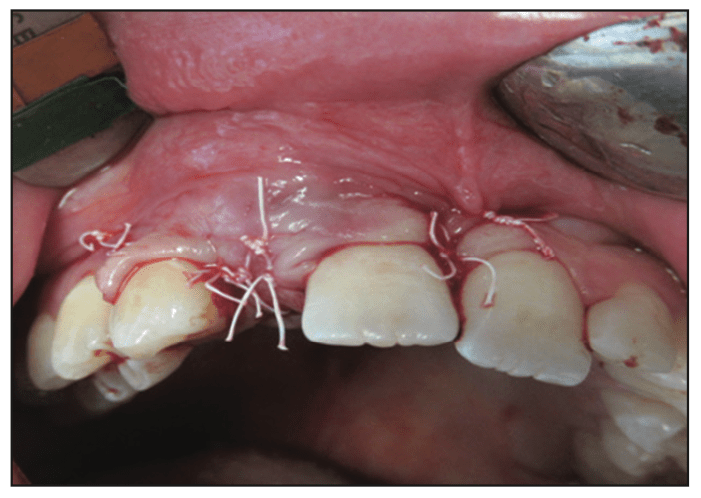
Figure 8. Primary closure, d-PTFE.
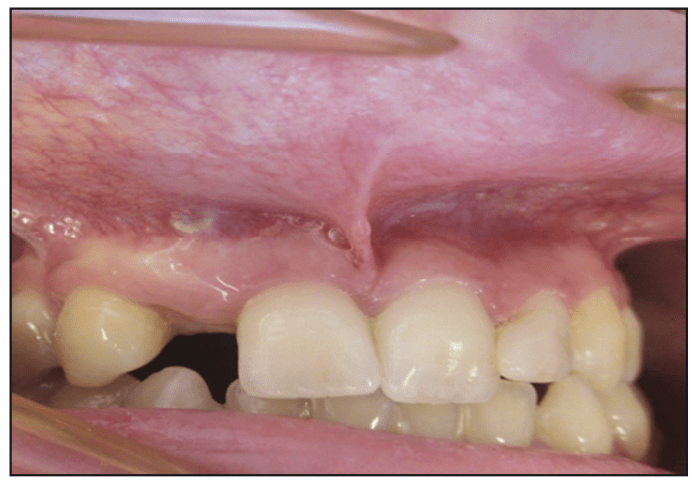
Figure 9. Surgical site after 4 months of healing.
The implant surgery procedure was prepared concerning PRP/PRF and local anesthesia exactly in the same manner as for the block graft. A midcrestal incision was made with a 15C Bard Parker blade extending distal to the maxillary right canine and mesial to the right maxillary central incisor. A full mucoperiosteal flap was reflected to expose the block retention screws and removed with the appropriate driver (Figures 10 and 11). The implant osteotomy was developed utilizing osseodensification (OD) Densah drills (Versah). The sequence was a 1.6-mm pilot drill rotating clockwise (forward), followed by 2.0-, 2.5-, and 2.8-mm Densah drills rotating in a counterclockwise (reverse) OD mode to a depth of 13 mm. A 3.2- × 13-mm SBM Legacy2 (Implant Direct) implant was inserted utilizing a straight driver to the level of the bony crest (Figure 12). A 3.2-mm transfer pin was placed, and a radiograph was taken prior to taking an impression with a heavy-body polyvinyl siloxane (Imprint III [3M]) material (Figures 13 and 14). A maxillary-mandibular relation and a shade B2/B1 were taken. A 3.2- × 2-mm healing collar was placed with a 1.25-mm hex tool and covered with a PRF bioactive membrane. The flap was approximated in a dual-closure approach with a horizontal mattress and interrupted 4.0 Vicryl sutures.
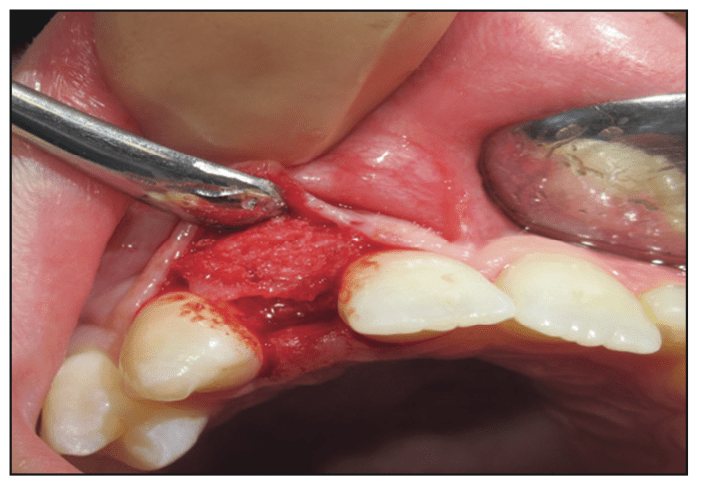
Figure 10. Full mucoperiosteal flap and allogenic block after 4 months of healing.
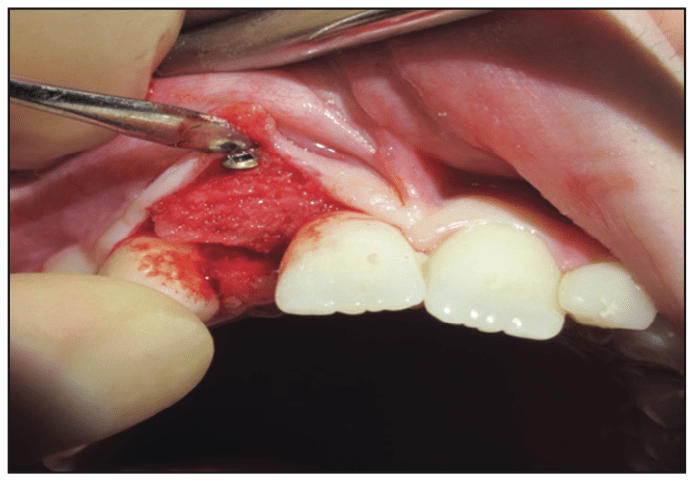
Figure 11. Fixation screw.
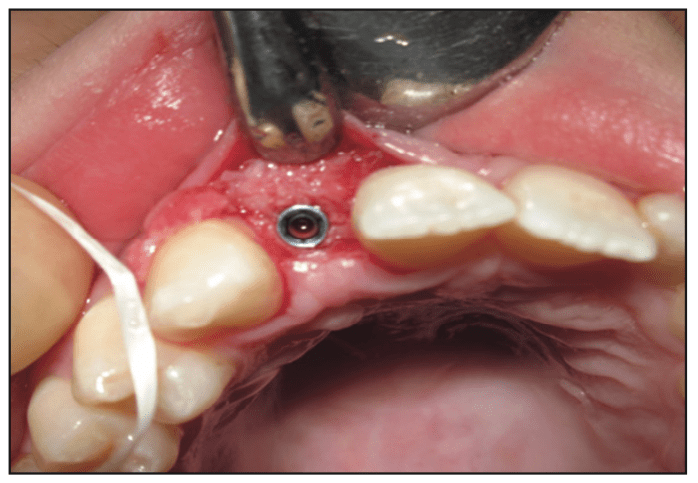
Figure 12. A 3.2- × 13-mm SBM Legacy2 implant (Implant Direct).
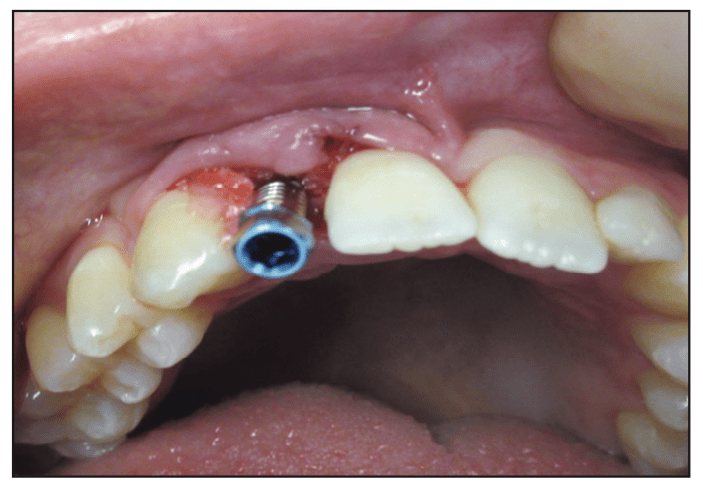
Figure 13. Impression transfer pin.
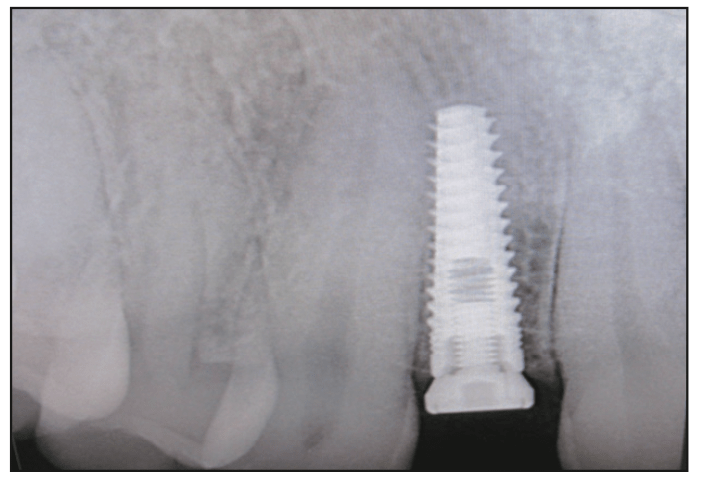
Figure 14. Periapical radiograph of the 2-mm healing collar.
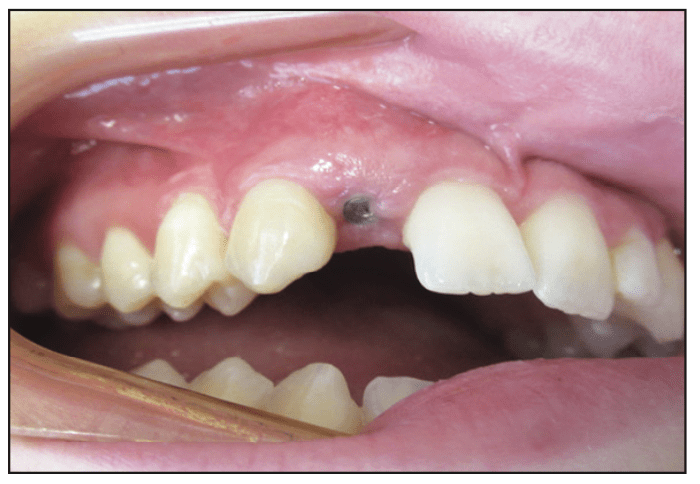
Figure 15. Healing collar after 4 months of healing.
The restorative stage was initiated 4 months post-implant fixture placement (Figure 15). After infiltration anesthesia, the 2-mm healing collar was removed with a 1.25-mm hex tool to expose the fixture (Figure 16). A titanium abutment was placed, a periapical radiograph was taken, and an abutment screw was torqued at 30 N/cm twice over a 5-minute time interval (Figures 17 and 18). The final porcelain-fused-to-metal crown was permanently cemented with zinc oxide phosphate cement (Figures 19 and 20).
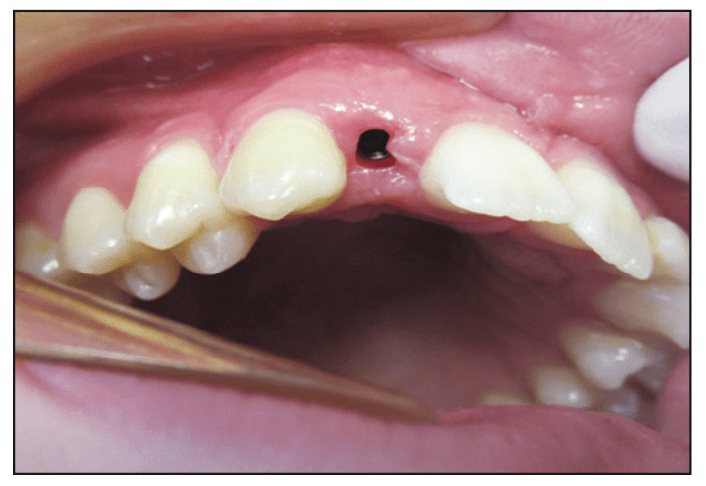
Figure 16. The fixture at 4 months.
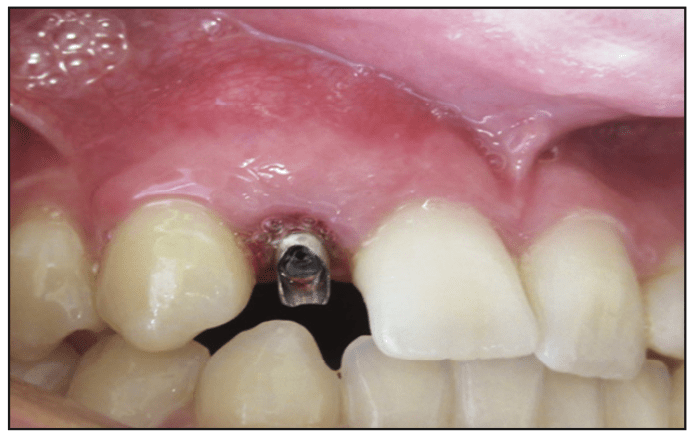
Figure 17. Titanium abutment.
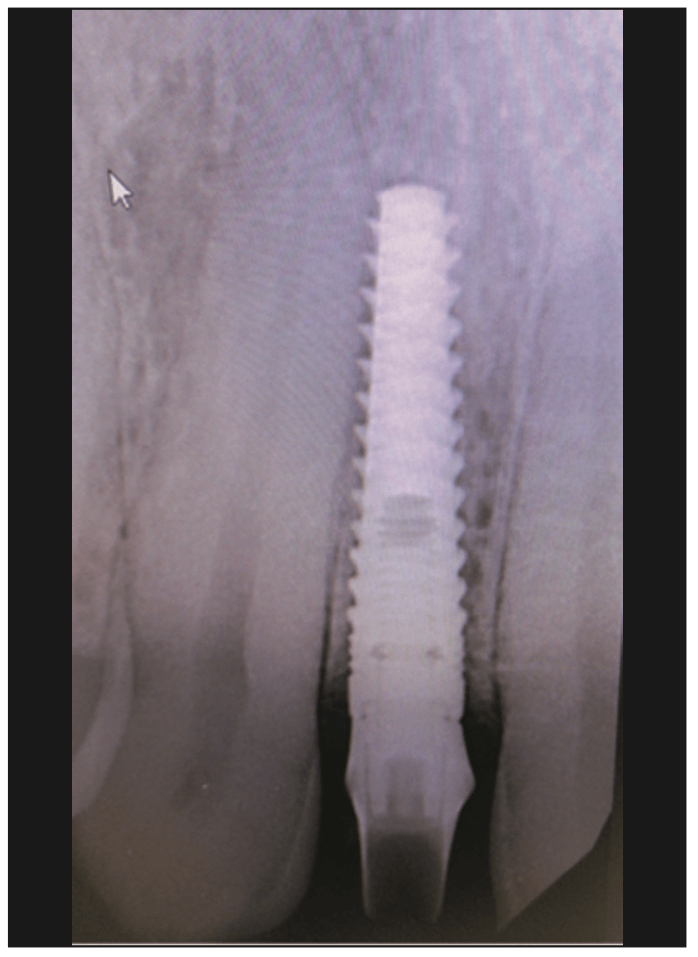
Figure 18. Periapical radiograph of the abutment/implant.
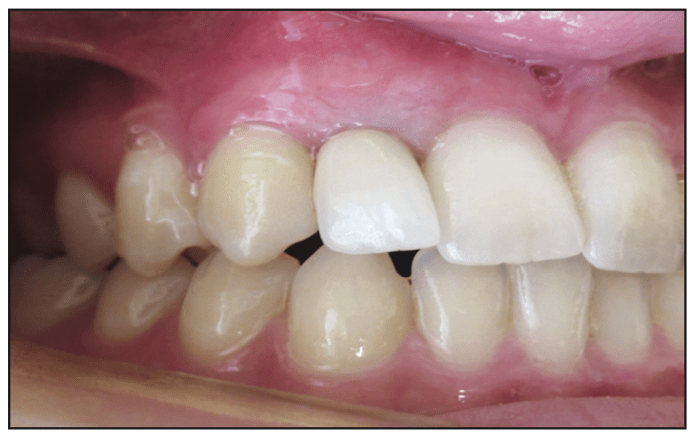
Figure 19. Final prosthesis, a porcelain-fused-to-metal crown (lateral view).
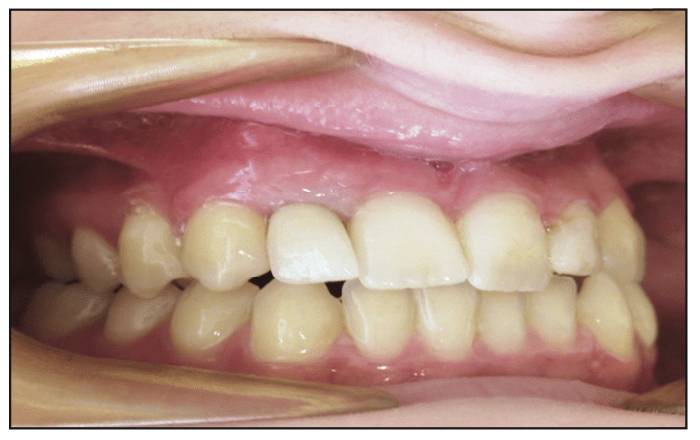
Figure 20. The porcelain-fused-to-metal crown (facial view).
DISCUSSION
Implant dentistry has provided many individuals with the opportunity to reconstruct lost oral structures.1 The need to reconstruct a deficiency in hard and soft tissue prior to the placement of dental implants is a common prerequisite.11 Many treatment approaches have been described in the literature, such as ridge expansion, GBR, and autogenous and allographic block grafts.12 The selection of a specific technique is based on the volume of alveolar ridge reconstruction needed or whether a staged or simultaneous implant placement can be achieved.
The utilization of block grafting for the reconstruction of a horizontal ridge deficiency has demonstrated high success rates.13,14 Autogenous block grafting is considered the gold standard because all bone development processes are involved in regeneration.15 Autogenous block grafts can be harvested from intraoral sites, such as the symphysis, ramus, or maxillary tuberosity.16 Extraoral sites utilized for grafting are the iliac crest, calvarian, and tibia. Autogenous grafts exhibit a high incidence of morbidity, paresthesia, devitalization of teeth, hospitalization, and costs.
Allogenic block grafts have become widely used in implant dentistry due to reduced morbidity and advances in processing for sterilization.17 Allogenic block grafts meet the pass criteria for bone regeneration development described by Wang and Boyapati.18 The cortical-cancellous nature of the block creates physical space, including porosity to foster vascularity to develop within the graft. The block can be fixated to the host site to create stability needed for bone growth. Allogenic block grafts have demonstrated high success rates histologically by the amount of vital bone growth they’ve enhanced.19 Furthermore, high implant survival rates are exhibited when implants are placed in allogenic block grafts.
This case report utilized a cortical-cancellous block graft sterilized via gamma radiation at 2.5 to 3.8 mrad to kill bacteria, viruses, and cells, and it was provided in a hydrated form. The hydrated form and cancellous component allow for compression with less breakage during the fixation process. The block graft is procured from the vertebra column exhibiting a curved anatomical shape.12,20
The techniques of the block graft procedure depend highly on the execution of the flap and block protocols.21 A tension-free closure is needed, requiring vertical releasing incisions and release of the periosteum. Release of collagen from the periosteum and elastin fibers in the mucosa is required to coronally advance the flap for a tension-free closure. The allogenic block is placed in a surgically developed area to enhance a positive seat in the host bone. The host bone is decorticated with multiple perforations to release growth factors via the regional acceleratory phenomenon.22
A Ti-machined fixation screw is placed through the block and into the host bone to eliminate any movement of the block graft. It is paramount that the block graft is in close approximation with the recipient site. The voids that exist around the block are filled in with particulate MIRB allograph and PRP.23,24 PRF bioactive and collagen type 1 membranes are utilized to cover the allogenic block and particulate graft. The membranes serve to promote soft- and hard-tissue healing as well as prevent epithelial migration into the allogenic block graft sites.25,26
The resorption of allogenic and autogenous block grafts has been under discussion for several years. Systematic reviews demonstrate minimal resorption of both types of grafts after 12 months and that they remain stable for 5 years.27 More importantly, implant survival rates in block grafts have been higher than 95%.28 Further studies have exhibited the presence of new bone formation histologically after 4 months, with a diminished residual graft bone. These studies are confirmed by the presence of osteogenic markers such as bone morphogenic protein (BMP), osteocalcin, and alkaline phosphate.29
Patient evaluation prior to block grafting is critical in developing a proper diagnosis. A diagnosis will guide the clinician in decision making concerning which horizontal ridge augmentation technique will accomplish a favorable outcome. A prophylaxis of adjacent teeth and an evaluation of the amount of keratinized tissue should be performed. A CBCT scan is ideal for evaluating the buccal palatal volume and shape of the ridge.30 The 3D image is helpful in determining the amount of bone regeneration needed to place an implant in the ideal position. Most importantly, it assists the clinician in making the proper decision on the surgical approach. The patient was prescribed a Cephalosporin (Keflex) antibiotic, ibuprophen, and chlorhexidine prior to surgery. The patient in this report was taking the medication Escitapram (Lexapro). Individuals prescribed selective serotonin reuptake inhibitors have exhibited a higher risk for implant failure. A study has demonstrated twice the failure rate for individuals taking the medication vs non-users. The clinical failure is evident at second-stage surgery or at the restorative stage, suggesting a negative biological remodeling effect.31
Platelet concentrates and allographic bone serve as a synergistic combination for bone growth. A single platelet contains an excess of 1,000 growth factors, including BMP, platelet-derived growth factor, insulin-derived growth factor, endovascular growth factor, and fibroblast growth factor. Growth factors enhance the recruitment and differentiation of cells associated with soft- and hard-tissue development.32 BC-PRP, utilized in this case with an allographic block and particulate bone, provides osseoinductive and osseoconductive properties for bone development. The graft utilized for this report was derived from the human vertebral column and gamma-irradiated at 2.5 to 3.8 mrad to sterilize the graft from viruses, bacteria, and cells. It was provided in a hydrated form that maintained flexibility, thereby preventing fracture during the fixation stage.
The implant surgical stage is performed after 4 months of healing. Studies have determined that approximately 45% of the graft is replaced with new vital bone after this time interval.29,33 In this case, the fixation screw was visible but not perforated through the mucosa. Although some resorption was evident around the head of the screw, the overall volume of the block was sufficient for implant placement. The osteotomy procedure was performed utilizing an osseodensification method due to a lower degree of drill chatter. The osteotomy was not undersized but developed using a hard-bone protocol to reduce internal forces during implant placement. This approach is utilized to prevent disturbance of the allograph and host-bone interface, which could potentially dislodge the grafted bone. The restorative stage was initiated at implant surgery due to a fixture stability of greater than 35 N/cm.
After a 4-month osseointegration period, second-stage surgery was performed with simultaneous placement of the final abutment and crown placement. Implant occlusal principles were completed prior to the patient being discharged.34
ACKNOWLEDGMENTS
The author wishes to acknowledge Tatyana Lyubezhanina, DA, and LeeAnn Klots, DA, for their assistance in preparation of this article.
REFERENCES
1. Albrektsson T, Brånemark PI, Hansson HA, et al. Osseointegrated titanium implants. Requirements for ensuring a long-lasting, direct bone-to-implant anchorage in man. Acta Orthop Scand. 1981;52(2):155–70. doi:10.3109/17453678108991776
2. Van der Weijden F, Dell’Acqua F, Slot DE. Alveolar bone dimensional changes of post-extraction sockets in humans: a systematic review. J Clin Periodontol. 2009;36(12):1048–58. doi:10.1111/j.1600-051X.2009.01482.x
3. Leonetti JA, Koup R. Localized maxillary ridge augmentation with a block allograft for dental implant placement: case reports. Implant Dent. 2003;12(3):217–26. doi:10.1097/01.id.0000078233.89631.f8
4. Starch-Jensen T, Deluiz D, Tinoco EMB. Horizontal alveolar ridge augmentation with allogeneic bone block graft compared with autogenous bone block graft: a systematic review. J Oral Maxillofac Res. 2020;11(1):e1. doi:10.5037/jomr.2020.11101
5. Elgali I, Omar O, Dahlin C, et al. Guided bone regeneration: Materials and biological mechanisms revisited. Eur J Oral Sci. 2017;125(5):315–37. doi:10.1111/eos.12364
6. Sakkas A, Wilde F, Heufelder M, et al. Autogenous bone grafts in oral implantology-is it still a “gold standard”? A consecutive review of 279 patients with 456 clinical procedures. Int J Implant Dent. 2017;3(1):23. doi:10.1186/s40729-017-0084-4
7. Lampert RC, Braidy HF, Zweig BE, et al. Intraoral augmentation vs allogenic block graft to preparation for dental implants placement: A retrospective cohort study. J Oral Maxillofac Surg. 2015;73:E30–1. doi:10.1016/j.joms.2015.06.050
8. Peleg M, Sawatari Y, Marx RN, et al. Use of corticocancellous allogeneic bone blocks for augmentation of alveolar bone defects. Int J Oral Maxillofac Implants. 2010;25(1):153–62.
9. Motamedian SR, Khojaste M, Khojasteh A. Success rate of implants placed in autogenous bone blocks versus allogenic bone blocks: A systematic literature review. Ann Maxillofac Surg. 2016;6(1):78-90. doi:10.4103/2231-0746.186143
10. Petrungaro PS, Amar S. Localized ridge augmentation with allogenic block grafts prior to implant placement: case reports and histologic evaluations. Implant Dent. 2005;14(2):139–48. doi:10.1097/01.id.0000163805.98577.ab
11. Tolstunov L. Classification of the alveolar ridge width: implant-driven treatment considerations for the horizontally deficient alveolar ridges. J Oral Implantol. 2014;40 Spec No:365–70. doi:10.1563/aaid-joi-D-14-00023
12. Troeltzsch M, Troeltzsch M, Kauffmann P, et al. Clinical efficacy of grafting materials in alveolar ridge augmentation: A systematic review. J Craniomaxillofac Surg. 2016;44(10):1618–29. doi:10.1016/j.jcms.2016.07.028
13. Fretwurst T, Nack C, Al-Ghrairi M, et al. Long-term retrospective evaluation of the peri-implant bone level in onlay grafted patients with iliac bone from the anterior superior iliac crest. J Craniomaxillofac Surg. 2015;43(6):956–60. doi:10.1016/j.jcms.2015.03.037
14. Keller EE, Tolman DE, Eckert S. Surgical-prosthodontic reconstruction of advanced maxillary bone compromise with autogenous onlay block bone grafts and osseointegrated endosseous implants: a 12-year study of 32 consecutive patients. Int J Oral Maxillofac Implants. 1999;14(2):197-209.
15. Nkenke E, Neukam FW. Autogenous bone harvesting and grafting in advanced jaw re5sorption: morbidity, resorption and implant survival. Eur J Oral Implantol. 2014;7 Suppl 2:S203-17.
16. Misch CM. Comparison of intraoral donor sites for onlay grafting prior to implant placement. Int J Oral Maxillofac Implants. 1997;12(6):767–76.
17. Fuglsig JMCES, Thorn JJ, Ingerslev J, et al. Long term follow-up of titanium implants installed in block-grafted areas: A systematic review. Clin Implant Dent Relat Res. 2018;20(6):1036–46. doi:10.1111/cid.12678
18. Wang HL, Boyapati L. “PASS” principles for predictable bone regeneration. Implant Dent. 2006;15(1):8-17. doi:10.1097/01.id.0000204762.39826.0f
19. Waasdorp J, Reynolds MA. Allogeneic bone onlay grafts for alveolar ridge augmentation: a systematic review. Int J Oral Maxillofac Implants. 2010;25(3):525–31.
20. Tatum OH Jr. Osseous grafts in intra-oral sites. J Oral Implantol. 1996;22(1):51–2.
21. Kleinheinz J, Büchter A, Kruse-Lösler B, et al. Incision design in implant dentistry based on vascularization of the mucosa. Clin Oral Implants Res. 2005;16(5):518–23. doi:10.1111/j.1600-0501.2005.01158.x
22. Frost HM. The regional acceleratory phenomenon: a review. Henry Ford Hosp Med J. 1983;31(1):3-9.
23. Rutkowski JL, Thomas JM, Bering CL, et al. Analysis of a rapid, simple, and inexpensive technique used to obtain platelet-rich plasma for use in clinical practice. J Oral Implantol. 2008;34(1):25-33. doi:10.1563/1548-1336(2008)34[25:AAOARS]2.0.CO;2
24. Soni R, Priya A, Agrawal R, et al. Evaluation of efficacy of platelet-rich fibrin membrane and bone graft in coverage of immediate dental implant in esthetic zone: An in vivo study. Natl J Maxillofac Surg. 2020;11(1):67-75. doi:10.4103/njms.NJMS_26_19
25. Omar O, Elgali I, Dahlin C, et al. Barrier membranes: More than the barrier effect? J Clin Periodontol. 2019;46 Suppl 21(Suppl Suppl 21):103–23. doi:10.1111/jcpe.13068
26. Machtei EE. The effect of membrane exposure on the outcome of regenerative procedures in humans: a meta-analysis. J Periodontol. 2001;72(4):512–6. doi:10.1902/jop.2001.72.4.512
27. Novell J, Novell-Costa F, Ivorra C, et al. Five-year results of implants inserted into freeze-dried block allografts. Implant Dent. 2012;21(2):129–35. doi:10.1097/ID.0b013e31824bf99f
28. Schlee M, Rothamel D. Ridge augmentation using customized allogenic bone blocks: Proof of concept and histological findings. Implant Dent. 2013;22(3):212–8. doi:10.1097/ID.0b013e3182885fa1
29. Correa LR, Spin-Neto R, Stavropoulos A, et al. Planning of dental implant size with digital panoramic radiographs, CBCT-generated panoramic images, and CBCT cross-sectional images. Clin Oral Implants Res. 2014;25(6):690–5. doi:10.1111/clr.12126
30. Wu X, Al-Abedalla K, Rastikerdar E, et al. Selective serotonin reuptake inhibitors and the risk of osseointegrated implant failure: a cohort study. J Dent Res. 2014;93(11):1054–61. doi:10.1177/0022034514549378
31. Bölükbaşı N, Yeniyol S, Tekkesin MS, et al. The use of platelet-rich fibrin in combination with biphasic calcium phosphate in the treatment of bone defects: a histologic and histomorphometric study. Curr Ther Res Clin Exp. 2013;75:15-21. doi:10.1016/j.curtheres.2013.05.002
32. Schlee M, Rothamel D. Ridge augmentation using customized allogenic bone blocks: proof of concept and histological findings. Implant Dent. 2013;22(3):212–8. doi:10.1097/ID.0b013e3182885fa1
33. Jun CM, Yun JH. Three-dimensional bone regeneration of alveolar ridge defects using corticocancellous allogeneic block grafts: Histologic and immunohistochemical analysis. Int J Periodontics Restorative Dent. 2016;36(1):75-81. doi:10.11607/prd.1950
34. Misch CE. Chapter 31: Occlusal considerations for implant-supported prosthesis. In: Misch CE, ed. Contemporary Implant Dentistry. 2nd ed. Mosby;1993:705–33.
ABOUT THE AUTHOR
Dr. Jackson graduated from Utica University with a BS degree in biology, cum laude. He received his DDS degree at the State University of New York at Buffalo School of Dental Medicine. He completed postgraduate training at St. Luke’s Memorial Hospital Center’s General Practice Residency Program. He completed his formal implant training through the New York AAID MaxiCourse in oral implantology at the New York University College of Dentistry. He is board-certified and a Diplomate of the American Board of Oral Implantology/Implant Dentistry and an Honored Fellow of the American Academy of Implant Dentistry (AAID). Dr. Jackson is the past president of the AAID. He is attending staff dentist for Faxton St. Luke’s Healthcare General Practice Residency Program. He is a member of the ADA and director of the AAID Boston MaxiCourse in oral implantology and the East Coast Implant Institute. Dr. Jackson has published several articles in peer-reviewed journals on the topic of oral implantology and implant dentistry. He can be reached via email at bjjddsimplant@aol.com.
Disclosure: Dr. Jackson is a speaker for Implant Direct but did not receive compensation for this article.











