INTRODUCTION
Osseointegration, as defined by Brånemark, is a direct structural and functional connection between ordered, living bone and the surface of a load-carrying implant.1 The process of osseointegration is very much dependent on the quantity and composition of osteoblast attachment to the implant surface. The quantity of osteogenic cells in contact with the titanium surface directly correlates to the amount of peri-implant bone and, as a result, the percentage of bone to implant contact (BIC). Extracellular proteins such as fibronectin are integral in the attraction and attachment of osteoblasts to the titanium surface.2 The aging of titanium results in the deposition of hydrocarbons on the surface, hydrophobicity, and conversion of the surface charge from positive to negative.3 This diminishes the bioactivity of the titanium so that proteins have less of an affinity for the implant surface and, consequently, inferior osteoblast proliferation, migration, and attachment compared to new titanium.3 The percentage of BIC is highly dependent on the bioactivity of the implant surface and its ability to interact biologically with the host’s mediators of osteogenesis.4,5 The osseointegration speed index (OSI), as measured by sequential implant stability quotients (ISQs), is also affected by the decreased bioactivity. This process has been researched and reported, and the ISQ is generally expected to be adequate at 3 to 6 months, depending upon the bone quality or type and characteristics of the implant surface.6-8 Implant surfaces have been modified over the years to enhance osseointegration by various methods, including plasma spraying, acid etching, or sandblasting the surface to gain improved adhesion, migration, and differentiation of osteoblasts, which increased the OSI and BIC.7,8 However, these modifications to the implant surface design do not prevent the accumulation of hydrocarbons on the titanium implant surface that occurs with aging.8-10 Aged titanium surfaces show less protein absorption (fibronectin, albumin) and consequently inferior osteoblast proliferation, migration, and attachment than a newly manufactured titanium implant.11 This results in a decrease in both the BIC and the biomechanical strength of the bone-titanium interface.10,12-14 A titanium implant that has aged has a BIC of 58%, whereas a newly manufactured implant has BIC of 90%.10,12-14
Modification of the aged implant surface is clinically desirable to increase the OSI and BIC through the reversal of titanium degradation caused by aging. A novel surface treatment termed photofunctionalization (PFZ) has been shown to accomplish this modification.10,14-22 The process of PFZ removes hydrocarbons, restores hydrophilicity, alters physiochemical properties, and restores bioactivity.
This article will present a case of UVCL treatment of a dental implant for the enhancement of the osseointegration process, reducing the functional osseointegration time from 12 to 16 weeks to 6 weeks.
CASE REPORT
A 47-year-old female patient reported to the Midwestern University College of Dental Medicine for replacement of her missing tooth No. 19. Restorative options, including fixed, removable, and implant-borne prosthetics, were presented, and the patient chose a dental implant. Her medical history was non-contributory, with no history of diabetes, tobacco use, or any immunosuppressant or anti-resorptive therapy and no past or present history of periodontal disease. She exhibited good oral home care and was committed to professional maintenance care every 4 months. She had lost tooth No. 19 from a periapical infection due to recurrent decay under a restoration she had received years ago. Tooth No. 19 was extracted without complication, followed by ridge preservation using mineralized/demineralized cortico-cancellous bone allograft (AlloOss [ACE Surgical Supply]) 7 months prior to implant placement surgery (Figure 1).

Figure 1. Residual ridge No. 19 seven months post extraction and ridge preservation.

Figure 2. CBCT scan showing residual ridge No. 19 seven months post extraction and ridge preservation.

Figure 3. The implant workup from the DIOnavi dental laboratory (DIO Implant).

Figure 4. Surgical guide fabricated for the case.

Figure 5. DIOnavi drilling sequence provided by the laboratory.

Figure 6. DIOnavi UVC vacuum light.

Figure 7. Implant with healing abutment immediately after placement.
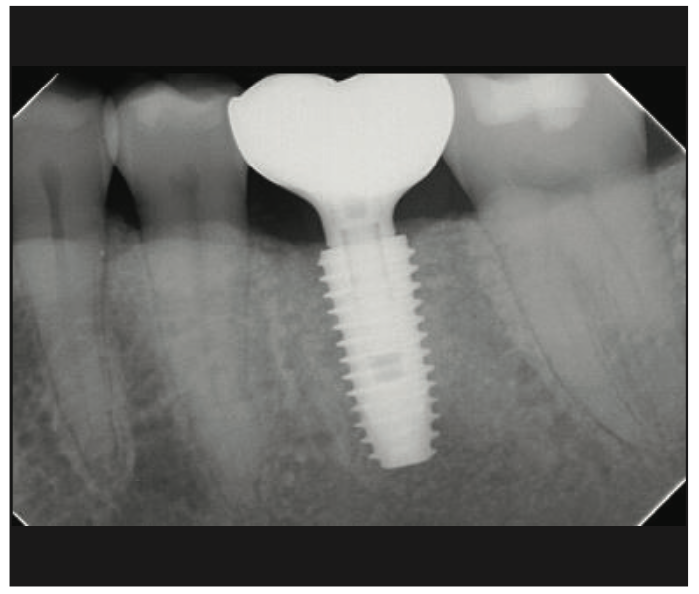
Figure 8. Restored implant.
A full maxillary and mandibular CBCT scan was acquired (3D Accuitomo 170 [J Morita]) (Figure 2) as well as intraoral scans (Emerald S scanners [Planmeca]), and the case was worked up in Romexis (version 6.3) implant planning software (Planmeca) to determine implant placement viability from a restoratively driven perspective. After that initial workup proved favorable, all data were electronically uploaded to the DIOnavi (DIO Implant, Busan, South Korea) portal for implant placement design and surgical guide fabrication (Figures 3 and 4). On the day of surgery, the DIO drilling protocol was followed (Figure 5). Before placement, the implant body was treated in a novel UVC vacuum light (DIO Implant) (Figure 6). A 5.0- × 11.5-mm DIO implant fixture was placed in site No. 19 with a seating insertion torque value of 50 Ncm. For investigative purposes, a CBCT scan was again taken on the day of implant placement (Figure 7), confirming the implant to be in a favorable position for restoration. At the 6-week mark, the patient returned; the healing abutment was removed; and ISQ readings were taken from the mesial, distal, buccal, and lingual, all registering at 85 (Osstell). The healing abutment was replaced, and the patient was then scheduled to begin the restorative phase of treatment at 6 weeks post implant placement. The final restoration is seen in Figure 8.
DISCUSSION
Ultraviolet light (UVL) is a form of radiation found on the electromagnetic spectrum. The spectrum consists of light types based on their wavelengths. These are radio, microwave, infrared, visible, ultraviolet A, ultraviolet B, ultraviolet C, x-ray, and gamma-ray waves. These wavelengths vary across the spectrum, with radio waves having the longest and gamma rays having the shortest. UVL is shorter than visible light, so it is invisible to most vertebrates, including humans, and the wavelengths range from 200 to 400 nm within this spectrum (Figures 9 and 10). In 1997, Wang et al,23 reported on the effects of UVL on the superhydrophilicity of TiO2, and applications were developed in many areas of industry, including anti-fogging, stain resistance, and antibacterial treatments, because of this research.24 Funato and Ogawa25 were the first to publish on the clinical application of PFZ to alter the surface of a titanium implant in 2013. Their study followed 7 implants that had micro-roughened surfaces that were photofunctionalized through exposure to UVL for 15 minutes chairside. All 7 implants were loaded early, and it was found that their ISQ values increased from insertion to loading. At one year, they found that all implants were integrated and under function after early loading. Funato et al26 researched the effects of PFZ through a retrospective study. They found that healing times can be shortened to 3.2 months from 6.6 months using PFZ, effectively increasing the OSI. The work of Suzuki et al27 has also shown that PFZ increases the OSI. While these reports showed clinical promise in the use of PFZ, 15 minutes to modify an implant chairside is not clinically applicable. However, research has continued, and a novel UVL activator (Figure 6) is now available to photofunctionalize implants chairside, according to the manufacturer (DIO Implant). This activator utilizes a 172-nm xenon excimer-generated vacuum ultraviolet light (VUV). The implants are stored in quartz ampules following manufacturing and subsequently modified in the VUV activator in these ampules as the quartz allows for the UVC light to exert maximum effect. This activator was tested against other commercially available devices, and it was found to accomplish greater than 90% decomposition of organic materials in the form of hydrocarbons.28 PFZ allows for the reversal of titanium degradation, and this restores the TiO2 layer, which restores bioactivity. Hydrocarbons are removed, hydrophilicity is restored, and the surface charge returns to positive. This, in turn, promotes protein adsorption, which enhances osteoblast migration, proliferation, and attachment to the implant surface. This results in improved biomechanical strength of the bone implant interface through increased BIC.29 By accomplishing this, the osseointegration stability curve is shifted to the left (Figures 11 and 12).

Figure 9. Partial light spectrum in nanometers.

Figure 10. Ultraviolet light spectrum information.

Figure 11. Typical stability curve associated with osseointegration.

Figure 12. Stability curve demonstrating the shift to left for UVL-treated implants.
CONCLUSION
This case demonstrates the successful implementation of a novel UVL activator in modifying a dental implant surface. In addition, this shows that it may be clinically applicable to photofunctionalize dental implants chairside and, as a result, increase the BIC and the OSI, effectively shortening treatment time and providing predictable results.
REFERENCES
1. Park NI, Kerr M. Chapter 2: Terminology in implant dentistry. In: Resnick R, ed. Misch’s Contemporary Implant Dentistry. 4th ed. Elsevier; 2020:20–2.
2. Hori N, Att W, Ueno T, et al. Age-dependent degradation of the protein adsorption capacity of titanium. J Dent Res. 2009;88(7):663–7. doi:10.1177/0022034509339567
3. Sugita Y, Saruta J, Taniyama T, et al. UV-pre-treated and protein-adsorbed titanium implants exhibit enhanced osteoconductivity. Int J Mol Sci. 2020;21(12):4194. doi:10.3390/ijms21124194
4. Lian Z, Guan H, Ivanovski S, et al. Effect of bone to implant contact percentage on bone remodelling surrounding a dental implant. Int J Oral Maxillofac Surg. 2010;39(7):690–8. doi:10.1016/j.ijom.2010.03.020
5. Pyo SW, Park YB, Moon HS, et al. Photofunctionalization enhances bone-implant contact, dynamics of interfacial osteogenesis, marginal bone seal, and removal torque value of implants: a dog jawbone study. Implant Dent. 2013;22(6):666–75. doi:10.1097/ID.0000000000000003
6. Colnot C, Romero DM, Huang S, et al. Molecular analysis of healing at a bone-implant interface. J Dent Res. 2007;86(9):862–7. doi:10.1177/154405910708600911
7. Davies JE. Understanding peri-implant endosseous healing. J Dent Educ. 2003;67(8):932–49.
8. Misch C. Dental Implant Prosthetics. 2nd ed. Mosby; 2015.
9. Albrektsson T, Zarb G, Worthington P, et al. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986;1(1):11-25.
10. Att W, Ogawa T. Biological aging of implant surfaces and their restoration with ultraviolet light treatment: a novel understanding of osseointegration. Int J Oral Maxillofac Implants. 2012;27(4):753–61.
11. Att W, Hori N, Takeuchi M, et al. Time-dependent degradation of titanium osteoconductivity: an implication of biological aging of implant materials. Biomaterials. 2009;30(29):5352–63. doi:10.1016/j.biomaterials.2009.06.040
12. Hori N, Att W, Ueno T, et al. Age-dependent degradation of the protein adsorption capacity of titanium. J Dent Res. 2009;88(7):663–7. doi:10.1177/0022034509339567
13. Att W, Hori N, Takeuchi M, et al. Time-dependent degradation of titanium osteoconductivity: an implication of biological aging of implant materials. Biomaterials. 2009;30(29):5352–63. doi:10.1016/j.biomaterials.2009.06.040
14. Hirota M, Ozawa T, Iwai T, et al. UV-mediated photofunctionalization of dental implant: a seven-year results of a prospective study. J Clin Med. 2020;9(9):2733. doi:10.3390/jcm9092733
15. Takeuchi M, Anpo M. Effect of UV light irradiation of different wavelengths on the surface wettability of titanium metal for dental implants. J Mater Sci Res. 2018. doi:10.29011/ JMSR-109/100009
16. Huang Y, Zhang H, Chen Z, et al. Improvement in osseointegration of titanium dental implants after exposure to ultraviolet-C light for varied durations: an experimental study in beagle dogs. J Oral Maxillofac Surg. 2022;80(8):1389–97. doi:10.1016/j.joms.2022.04.013
17. Chang LC. Clinical applications of photofunctionalization on dental implant surfaces: a narrative review. J Clin Med. 2022;11(19):5823. doi:10.3390/jcm11195823
18. Arroyo-Lamas N, Arteagoitia I, Ugalde U. Surface activation of titanium dental implants by using UVC-LED irradiation. Int J Mol Sci. 2021;22(5):2597. doi:10.3390/ijms22052597
19. Tabuchi M, Hamajima K, Tanaka M, et al. UV light-generated superhydrophilicity of a titanium surface enhances the transfer, diffusion and adsorption of osteogenic factors from a collagen sponge. Int J Mol Sci. 2021;22(13):6811. doi:10.3390/ijms22136811
20. Sugita Y, Saruta J, Taniyama T, et al. UV-pre-treated and protein-adsorbed titanium implants exhibit enhanced osteoconductivity. Int J Mol Sci. 2020;21(12):4194. doi:10.3390/ijms21124194
21. Camolesi GCV, Somoza-Martín JM, Reboiras-López MD, et al. Photobiomodulation in dental implant stability and post-surgical healing and inflammation. A randomised double-blind study. Clin Oral Implants Res. 2023;34(2):137–47. doi:10.1111/clr.14026
22. Suzuki S, Kobayashi H, Ogawa T. Implant stability change and osseointegration speed of immediately loaded photofunctionalized implants. Implant Dent. 2013;22(5):481–90. doi:10.1097/ID.0b013e31829deb62
23. Wang R, Hashimoto K, Fujishima A, et al. Light-induced amphiphilic surfaces. Nature. 1997;388:431–2. doi:10.1038/41233
24. Aita H, Hori N, Takeuchi M, et al. The effect of ultraviolet functionalization of titanium on integration with bone. Biomaterials. 2009;30(6):1015–25. doi:10.1016/j.biomaterials.2008.11.004
25. Funato A, Ogawa T. Photofunctionalized dental implants: a case series in compromised bone. Int J Oral Maxillofac Implants. 2013;28(6):1589–601. doi:10.11607/jomi.3232
26. Funato A, Yamada M, Ogawa T. Success rate, healing time, and implant stability of photofunctionalized dental implants. Int J Oral Maxillofac Implants. 2013;28(5):1261–71. doi:10.11607/jomi.3263
27. Suzuki S, Kobayashi H, Ogawa T. Implant stability change and osseointegration speed of immediately loaded photofunctionalized implants. Implant Dent. 2013;22(5):481–90. doi:10.1097/ID.0b013e31829deb62
28. Suzumura T, Matsuura T, Komatsu K, et al. A novel high-energy vacuum ultraviolet light photofunctionalization approach for decomposing organic molecules around titanium. Int J Mol Sci. 2023;24(3):1978. doi:10.3390/ijms24031978
29. Pyo SW, Park YB, Moon HS, et al. Photofunctionalization enhances bone-implant contact, dynamics of interfacial osteogenesis, marginal bone seal, and removal torque value of implants: a dog jawbone study. Implant Dent. 2013;22(6):666–75. doi:10.1097/ID.0000000000000003
ABOUT THE AUTHORS
Dr. Beals earned his BS, MS, and DDS degrees at The Ohio State University. He remained at Ohio State to complete a residency in oral and maxillofacial surgery, then relocated to Phoenix, where he entered private practice. He is currently a clinical associate professor at Midwestern University Dental Institute in Glendale, Ariz. He can be reached at dbeals@midwestern.edu.
Dr. Francis is a clinical associate professor at the College of Dental Medicine, Midwestern University in Glendale. He can be reached at jfranc@midwestern.edu.
Dr. Barber is a clinical associate professor at the College of Dental Medicine, Midwestern University. He can be reached at hbarbe@midwestern.edu.
Dr. Siu is a clinical associate professor at the College of Dental Medicine, Midwestern University. He can be reached via email at tsiu@midwestern.edu.
Dr. Cianciola is a clinical assistant professor at the College of Dental Medicine, Midwestern University. He can be reached at jcianc@midwestern.edu.
Disclosure: The authors report no disclosures.










