The biggest challenge with patients today is getting them to understand their dental problems fully and get them treated! One can use the most sophisticated computer systems or imaging, but if you don’t build rapport and trust with the patient, then the rate of case acceptance will decrease. Because of this, my main goal in an initial examination is getting to know the patient and understanding his or her needs. In fact, my initial conversation with a patient may have nothing to do with teeth or dentistry. It may be about the patient’s children or family or even the field in which he or she works. Whatever the topic, it is important to really listen and get to know your patients.
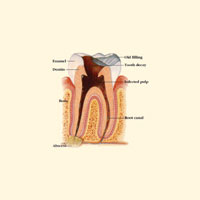
Once the relationship between patient and provider has been established, it is important for patients to visualize and understand their dental condition. An easy way to illustrate their condition is through use of an intraoral or digital camera. These images will enhance patients’ understanding of their condition very quickly. However, since patients don’t have a dental background or an understanding of tooth anatomy, these images of cavities may simply appear as stains to them. Cracks in failing amalgam restorations may just appear as “wear” in their eyes. They really don’t understand what is going on inside the tooth or under the gumline.
Having used many different case acceptance tools over the years, I realized 2 very important concepts. The first was that I, the provider who had established rapport with the patient, needed to explain the dental condition and proposed treatment…not some automated software or computer. Secondly, I needed a method of visual explanation that was accurate, concise, and easy to implement. Drawings and pictures seemed to work well, however patients in my practice appeared to respond even better to anatomical models.
CASE STUDY
 |
 |
|
Figure 1. Failing amalgam restorations on teeth Nos. 18 to 21. |
Figure 2. DemoDent patient education model. |
 |
 |
|
Figure 3. Close-up view of cracked tooth demonstration. |
Figure 4. Recurrent decay evident upon amalgam removal. |
 |
|
Figure 5. Crown restorations on teeth Nos. 18 to 21. |
A male patient presented to the office with discomfort on the lower left side. After a thorough clinical examination and necessary radiographs, it was apparent that some of these teeth had recurrent decay, open margins, and cracks. He complained of hot and cold sensitivity as well as discomfort on biting. An intraoral image was taken of teeth Nos. 18 to 21 and shown to the patient (Figure 1). The patient was asked how long ago he thought these restorations were placed. The patient replied that these restorations were placed more than 20 years ago. A thorough explanation of what the patient was experiencing with teeth Nos. 18 to 21 was provided using the DemoDent (DemoDent) patient education anatomical model (Figure 2). As seen in the close-up section of the model shown in Figure 3, an open or failing margin allows food and/or bacteria to leak underneath the existing restoration, resulting in recurrent decay. Once the patient understood his dental condition, he was eager to have the teeth restored to proper form and function before endodontic treatment was ultimately necessary. Treatment consisted of cores and crowns for teeth Nos. 18 to 21.
When the patient returned for treatment, he was administered local anesthetic. Amalgam removal was achieved using a Samurai carbide bur (Simple Dental) in a quick and efficient manner. Once the existing restorations were removed, an image was taken of teeth Nos. 18 to 21 (Figure 4). There was indeed recurrent decay that had extended underneath the amalgam restorations. Using the DemoDent anatomical model, the patient was again educated about the process of the failing restorations and what was needed to restore the teeth. In fact, the patient commented on how quickly he would like to have the other areas of his mouth restored since he had seen the pictures and understood the progression of tooth decay on the Demo-Dent model.
Using a No. 4 round bur, any remaining caries was removed from the teeth. Since the preparations were deep and in close proximity to the pulp, a self-etching bonding agent was used. Core buildups were created with composite material, and the teeth were prepared for full-crown restorations. The patient returned 2 weeks later for placement of the definitive crowns on teeth Nos. 18 to 21 (Figure 5).
CONCLUSION
There are many ways to educate patients in order for them to understand their dental concerns and get them treated. One of the most effective ways is to show the patient visually what is going on and then describe the condition and its effects using an anatomical model. Anatomical models allow the patient to visualize the tooth 3-dimensionally in a clear and concise manner. Once patients understand their condition, they value the importance of the treatment necessary to restore their mouth to proper function and health. In return, the dental provider can feel confident that he or she has completely educated and served the patient.
Dr. Nazarian is a graduate of the University of Detroit-Mercy School of Dentistry. Upon graduation, he completed an AEGD residency in San Diego, Calif, with the US Navy. He is a recipient of the Excellence in Dentistry Scholarship and Award. Currently, he maintains a private practice in Troy, Mich, with an emphasis on comprehensive and restorative care. His articles have been published in many of today’s popular dental publications. Dr. Nazarian also serves as a clinical consultant for the Dental Advisor, testing and reviewing new products on the market. He has conducted lectures and hands-on workshops on aesthetic materials and techniques throughout the United States. He can be reached at (248) 457-0500 or at drnazarian@premierdentalcenter.com.
Disclosure: Dr. Nazarian is the creator of the DemoDent patient education model system.