Restoration of the single maxillary central incisor is without doubt the most challenging aesthetic procedure in dentistry.1 Both anatomically and in a dental patient’s perception, the maxillary central incisors are front and center in a smile. More than any other pair of teeth in the mouth, these two set the tone for a person’s appearance, positively or negatively. This is why dental patients are more sensitive to any discrepancy between the full-coverage restoration of a single maxillary central incisor and its natural counterpart than with any other teeth.
Many different factors influence the successful outcome of such restorative procedures. Among them are the extant proximal hard-and soft-tissue status; tooth preparation design; materials used; skill of the involved laboratory technician(s); and the effectiveness of communication between the treating dentist and laboratory if a remote laboratory is used. Since only about 5.5% of all restorative dentists in the United States have an in-house laboratory (according to statistics available from the ADA Survey Center as of 2006), remote laboratories make the majority of these crowns.
The following is a case report describing each stage in restoring a lone maxillary central incisor.
Case Report
 |
 |
|
Figure 1. Patient presented with fractured crown on tooth No. 8. |
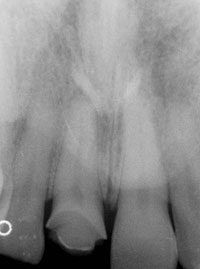
Figure 2. Radiograph revealed no periapical pathology or abnormalities. |
The patient was a 30-year-old male with no noteworthy medical conditions, save for an allergy to penicillin, who presented to our office for the first time with a chief complaint of a fractured crown of tooth No. 8 (Figure 1). A small fragment of the crown remained luted to its lingual surface, and the remainder was lost. He related a history of trauma in his mid teens to what had been a virgin tooth, which had necessitated placement of this porcelain jacket crown. It had functioned adequately for more than 15 years until fracturing on a foreign object in food just before his first visit with us. Tooth No. 7 had also suffered some comparatively minor damage at its incisal aspect from this trauma, but the patient and his parents had elected to restore only tooth No. 8 at the time.
On his initial comprehensive examination, the patient’s periodontal readings and occlusal analysis revealed no significant pathology. A full-mouth series of radiographs taken at this time identified no periapical pathology or other abnormalities, including tooth No. 8 (Figure 2). After gathering all clinical records, arriving at a diagnosis, and provision of routine preventive care, restorative treatment planning began. Besides operative treatment of incipient carious lesions at the occlusal and buccal surfaces of tooth No. 31, no other restorative needs were diagnosed at this examination. Vital tooth lightening and restoring the incisal of tooth No. 7 were discussed with the patient in conjunction with the retreatment of tooth No. 8, but he declined these options.
The mesiodistal dimension of the space that remained after the loss of tooth No. 8’s crown was equal to the same dimension of tooth No. 9, thus enabling the new crown’s form to be a mirror image of its natural complement. This in turn would allow for symmetrical contact point positioning and provide for an appropriate soft-tissue architecture, as sounding depths at both aspects of tooth No. 8 were less than 4 mm.2 The restoration of tooth No. 8 was now ready to proceed.
Deciding on the appropriate restorative material was the next step in this process. Since the patient exhibited no occlusal discrepancies or parafunctional habits, had a lighter stump shade at this site,1 and had been functioning acceptably for more than 15 years with a porcelain jacket crown, I decided on IPS Empress (Ivoclar Vivadent) as the material of choice. IPS Empress offers me unsurpassed aesthetics (the most critical factor in this decision), allows me to avoid gingival tissues with the restoration under the right conditions (when desired), and as a pressed ceramic is the easiest material with which to mimic the coronal hard tissues.3 The existing, just slightly supra-gingival preparation design also influenced my choice of materials in this case. In circumstances where occlusal, tooth preparation color,1 or periodontal considerations dictate another material, I would go with Captek (Precious Chemicals Company), as it is a stronger material and displays a higher resistance to the deposits that can cause periodontal disease.4 It can also be as aesthetic as any material on the market, as patients in one trial of multiple restorations fabricated for a single upper incisor unanimously chose the Captek units for definitive cementation.5
Having chosen the material I would use for this procedure, I then proceeded to redefine the existing crown preparation, removing what was left of the previous crown in doing so. This left the preparation essentially as it was when first cut—chamfered with just barely supragingival margins circumferentially. The final impression was taken in Examix NDS (GC America) along with all shade records before provisionalization, and was sent to the author’s dental laboratory for fabrication of the definitive IPS Empress crown.
 |
 |
 |
|
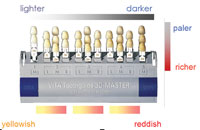
Figures 3 to 5. Digital photos helped to determine correct shade. |
Shade information is the most difficult to communicate with a remote dental laboratory,6 and in accurately reproducing the single maxillary central incisor it is absolutely critical. It has been my experience that patients will be less tolerant of a shade deviation in these situations than with any of the other parameters involved. Therefore, the methods used to record shade selection are equally vital, and over the years I have refined my technique from the single shade tab equivalents I was taught in dental school to the utilization of digital shade-matching devices with adjunctive photography to attain the best results. Such devices record and analyze tooth color information in the mouth to produce a computer file detailing the exact porcelain blends necessary to replicate the intended shade according to the Munsell color system parameters of hue, value, and chroma.6
Using my modified Olympus CZ3000 camera (Lester A. Dine), I first took digital photos of the different tabs I had chosen for the separate gingival, body, and incisal shades to match tooth No. 9 (Figures 3 to 5). I also took a stump shade photo of the finished preparation, which coincided with the body shade I had taken previously, as I have often found to be the case. These photos served to confirm the readings I would record with my ShadeVision (X-Rite) digital matcher and show the details of tooth No. 9’s surface texture along with any unusual characterizations that might be present. After carefully considering units from several different manufacturers, I found Shade-Vision to be the best combination of both user friendliness (on both ends of the dentist/CDT interface) and accuracy. Since I started using it, I have been able to realize dependably superior shade matches that leave little to be desired. I then took the ShadeVision measurement, attaching the previously obtained digital photographs to the file its software generates, and e-mailed all of this clinical information to the laboratory. After a virtual try-in, as allowed by the ShadeVision software, my office received the definitive restoration.7
 |
| Figure 6. Excellent shade match, but a small under-texturing on the labial aspect required modification in the laboratory. |
 |
 |
|
Figures 7 and 8. The unit was sent back to the laboratory for reconfiguration of the labial surface. |
 |
 |
|
Figures 9 and 10. Final aesthetic result. |
On trying in this unit, I found an excellent shade match whose only flaw was a small under-texturing of its labial aspect (Figure 6) that was not discernible with the virtual try-in. The surface texture of a porcelain restoration has a subtle but definite effect on a patient’s perception of its shade.6 The unit was sent back to the laboratory for reconfiguration of the labial surface, and its new contours were confirmed with digital photography via e-mail prior to its return from the laboratory (Figures 7 and 8).
At the patient’s next visit, this unit was tried in again, and the patient and author found it to be an accurate likeness of its counterpart regarding all essential criteria including shade, contour, proportion, and soft-tissue framework. A minimal enameloplasty was then performed at the mesioincisal of tooth No. 9 to smooth a rough edge. The crown was luted to place with RelyX Unicem Self-Adhesive Universal Resin Cement (3M ESPE) at the same visit, and a routine semiannual recall revealed a restoration that had satisfied the patient’s aesthetic expectations in full while having satisfactory function and periodontal health (Figures 9 and 10).
CONCLUSION
The aesthetic considerations in restoring any single anterior tooth are challenging,8 and they become even more demanding when that single anterior tooth is the maxillary central incisor.1 The standard in judging restorations of this type is that they should be undetectable when viewed at a conversational distance.9 To achieve this standard, the dentist must satisfy several qualities that depend on careful case selection and favorable clinical conditions. These include correctly recreating the shade, contour, proportion, and soft-tissue framework of the remaining natural upper central incisor. To do this, the dentist must properly evaluate the existing adjacent hard and soft tissues and utilize a suitable tooth preparation design and restorative material. He or she must also employ skilled laboratory technicians and effectively communicate the requisite clinical information to the dental laboratory, if a remote one is used. When this is done adroitly, an outcome will be realized that the vast majority of dental patients will be satisfied with, and that the treating dentist can be proud of.
References
- Kahng LS. Material selection and shade matching for a single central incisor. J Cosmet Dent. 2006;22:78-84. Available at: www.aacd.com/downloads/journal/22-1Kahng.pdf. Accessed June 15, 2007.
- Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol. 1992;63:995-996.
- Christensen GJ. Why all-ceramic crowns? J Am Dent Assoc. 1997;128:1453-1455.
- Goodson JM, Shoher I, Imber S, et al. Reduced dental plaque accumulation on composite gold alloy margins. J Periodontal Res. 2001;36:252-259.
- Nathanson D, Nagai S, Po S, et al. Preliminary evaluation of the effect of crowns on gingival color. Presented at: The IADR/AADR/CADR 82nd General Session; March 10-13, 2004; Hon-olulu, Hawaii. Abstract 1478. Available at: http://iadr.confex.com/iadr/2004Hawaii/techprogram/abstract_46508.htm. Accessed June 15, 2007.
- McArdle BF. Shade matching for single indirect restorations using a remote laboratory. Contemp Esthet. 2006;10:36-43.
- Laminates – virtual try-in technique. ShadeVision product page at X-Rite Website. August 26, 2005. Available at: http://www.xrite.com/product_overview.aspx?Industry=14&Segment=16&ID=428&Action=Support&SupportID=3338. Accessed September 18, 2006.
- Christensen GJ. Restoring a single anterior tooth: solutions to a dental dilemma. J Am Dent Assoc. 2004;135:1725-1727.
- McLaren E. Esthetics – implant and more. Presented at: The Seacoast Esthetic Dentistry Association; May 14, 2005; Portsmouth, NH.
Acknowledgment
The author would like to thank Josh Gall and his team of ceramists at Biotemps Dental Laboratory for their expertise in the fabrication of the restoration depicted in this article.
Dr. McArdle graduated from Tufts University School of Dental Medicine in 1985 and has been practicing general dentistry on the New Hampshire seacoast ever since. He has served on the active medical staff in dentistry of Concord Hospital in Concord, NH, and on the board of directors of Priority Dental Health (prioritydental.com), the New Hampshire Dental Society’s Direct Reimbursement entity. He is a co-founder of the Seacoast Esthetic Dentistry Association (dentalesthetics.com), which is headquartered in Portsmouth, NH. He is the founder of Seacoast Dental Seminars (seacoastdentalseminars.com), also headquartered in Portsmouth. He has authored numerous other articles both nationally and internationally in major peer-reviewed publications. He can be reached at (603) 430-1010, drmcardle@seacoastdentalseminars.com, seda@dentalesthetics.com, or by visiting mcardledmd.com.