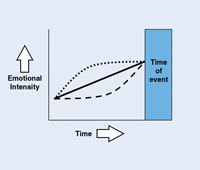
Turn on the television or the radio. Open a newspaper or magazine. Visit a few online sites. What do you find? Ads. Wherever there are consumers, there are advertisements for products. We’re inundated with recommendations that we purchase a particular car, consider a new cosmetic, wear a stylish line of clothing, install a new appliance. We are flooded with snippets of information that we quickly cast off or never even see because we’re not ready to consider them, relegating each to wallpaper be-hind far more pressing details that have immediate relevance to our lives.
But when the time comes and our car is showing the wear and tear of many miles, or we’re noticing the little lines curl around our smile, or the refrigerator is no longer adequate for our wants and needs, then we begin to open ourselves up to the messages around us. We pause to consider the new car promotions. Those antiaging creams capture a bit more of our attention, and we just might listen to that Best Buy advertisement on television rather than hit the mute button. We are now open to learning more.
 |
| Illustration by Brian C. Green |
Such is the case when the emergency patient sits in your chair. Up until this moment, that person may not have been interested in what you have to offer. But his or her situation has prompted consideration not only of immediate treatment but, quite possibly, comprehensive care as well. Yet dental teams miss this opportunity time and again. According to the industry standard, 80% of all emergency patients should be converted to comprehensive exams. If yours is lower, then it’s time to develop a plan to seize the “teaching moments” that emergency cases present.
GOOD CALL OR BAD?
Patients and staff often view emergency appointments as negative and potentially problematic. Consequently, practices commonly send the wrong message to those pa-tients with whom they must interact under pressure. The person is squeezed into an already full schedule. Although it’s probably not intentional, the emergency patient is frequently viewed as an annoyance and an interruption to the day rather than an opportunity.
When the emergency patient calls your office, what’s the reaction? Irritation? Frustration? Increased stress? Depends on the time and the day? Here’s what happens in many offices. The scheduling coordinator takes the call and scans the already full schedule. With a labored sigh, he or she tells the patient it’s going to be very difficult for the practice to work the appointment in, but it will. Oh, and doctor expects payment up front. Within the first 60 seconds of contact with that emergency patient, your practice is laying the groundwork for conversion to a comprehensive exam…or not.
No matter what the circumstances—full schedule, stressful situations, etc—emergency patients must be treated with compassion and understanding. Each day the dental team should identify where emergency patients are to be placed in the schedule; this way, there are no surprises for the clinical staff, and the scheduling coordinator knows exactly where emergencies are to be placed.
Next, increase awareness among your team. Business staff members, who tend to be more task oriented and are much more comfortable when the day runs according to a specific plan and schedule, occasionally need to be reminded that emergency patients are likely to require more empathy and concern than they may typically convey in their day-to-day patient communication. The emergency patient should feel that your practice is one that is understanding and helpful—not punitive.
Listen to how the emergency patient calls are handled. Are these conversations warm and welcoming? How would you feel if you were an emergency patient calling your office? Would you be glad you chose this practice or would you feel that the practice’s primary concern is the payment rather than the patient?
I recommend that dental teams develop phone scripts to help them effectively communicate with emergency patients from the very first word. The script provides a general guide to assist all staff, no matter who picks up the phone, in gathering necessary information, conveying essential details, and continuously expressing a helpful and caring tone and attitude throughout the exchange.
Welcome the patient when he or she enters the practice and greet him or her with a smile. Assure the patient that the clinical team is excellent and will provide very good care. Let the patient know approximately how long the wait will be. Ask if the patient would like assistance completing his or her paperwork. If the patient is in con-siderable discomfort, then take him or her into a consultation room or other quiet area, where a staff member can assist with completing practice medical forms and other documents. The focus should be on making the process as easy and comfortable as possible for the patient.
READ THE CUES
Each member of the team plays an important role in putting the patient at ease as well as gathering information that will be essential in understanding the likely barriers to future treatment. Pay attention to cues the patient is giving. The conversation that the assistant has with the individual can be particularly useful in identifying those issues that will need to be addressed in order for the patient to consider further care. Does the patient appear anxious or fearful? Does the patient comment that he or she is concerned about the cost of the treatment, or the pain, or the time the procedure is going to require? Is the patient apologizing because it’s been such a long time since he or she has been in for an appointment? Has the patient had a negative dental experience in the past? Is the patient angry or frustrated?
In talking to the patient, the assistant should be able to identify the most likely obstacles the dental team will encounter when encouraging this patient to pursue comprehensive care.
PREPARE FOR THE COMMON BARRIERS
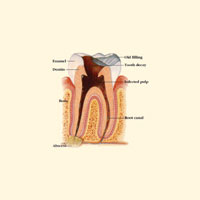
Track the most common reasons why emergency patients wait until there is a problem before coming into the practice. Understanding the “why” behind patient reticence is essential to addressing it. From there the team can develop a patient communication strategy through the use of scripts and educational materials to overcome those barriers. Just as scripts are essential at the front desk when answering phones, they are also critical when educating patients about the value of ongoing dental care. Moreover, they are a safety net that prepares the staff to know what to say, how to say it, and when to say it. If the patient is highly anxious, then team members should have a specific script and protocol that they follow to put the patient at ease. If the patient is concerned because he or she doesn’t understand why a specific procedure is needed, then the staff should be prepared to respond through educational videos, printed materials, dental models, etc. Companies such as ADA Intelligent Dental Marketing offer several short, patient-friendly videos covering numerous topics, including dental hygiene, implants, crown and bridge, endodontics, and much more.
Anticipating patient concerns and being prepared to address them enables staff to educate patients confidently and consistently, to seize the teaching moments effectively. Staff members aren’t in a situation in which they have to think on their feet; they have anticipated the barrier and have a plan to address it. What’s more, patients appreciate the ef-fort to address their concerns and help them understand. Dental team members aren’t just trying to get the patient out of the chair as quickly as possible so that they can return to their regular schedule.
EFFECTIVE SCRIPTS AND ROLE PLAYING
Set aside time during the weekly or monthly staff meetings to develop scripts. Don’t get bogged down in ad-dressing every possible scenario immediately. Pick a couple of key barriers and address those initially. The doctor and team should work together to fine-tune the documents over time and to develop an easy and natural flow. Once you feel confident in using those, create a few more.
Keep in mind that the best scripts use words, phrases, and questions that prompt patients to respond the way you want them to respond. Those who are able to use scripts most effectively understand the message they need to convey. They know the information and material thoroughly. They are not reciting the copy verbatim; rather, they are able to use the scripts as a guide and adapt them so they come across naturally, as if they were chatting with the patient over coffee. What’s more, teams that use scripts to their full advantage practice, practice, practice, and regularly engage in role-playing.
Role-playing is essential to help staff members with average communication skills raise their level of performance. In addition, it enables the team to determine how best to phrase questions and determine the most appropriate sequence for statements and questions. For example, business staff would carefully script where they place questions involving insurance or statements regarding the practice’s financial policy so as not to send un-intended messages to emergency patients.
What’s more, role-playing enables team members to pay close attention to their tone and how their words come across to others. Are they perceived as being warm and caring, yet still assertive? Do they seem tim-id and easily flustered or manipulated? Or might they appear abrupt and cold? Listening to responses and coaching each other on how to improve those responses ensures that team members are well prepared to handle emergency patient communication. Moreover, it en-ables the doctor to hear how staff would react in specific situations and to redirect that approach if it is inconsistent with practice protocol or policies.
LASTING IMPRESSION
After the treatment, escort patients to the front desk and impress upon them once again the importance of on-going care. Explain to the scheduling coordinator that the patient needs an ap-pointment for a comprehensive exam. Time should be set aside in the schedule to allow emergency patients to be scheduled for comprehensive exams as soon as possible, not in 6 weeks or 6 months, but preferably within the next week.
That evening or the next, the doctor follows up with a phone call to check on the patient and express the doctor and staff’s appreciation for the opportunity to provide care. A few days later the patient should receive a package in the mail with printed information about your practice and your services. Attached to that is a handwritten note from the doctor’s assistant that speaks specifically to the patient’s experience, expresses concern for his or her well-being, and indicates that the staff is looking forward to seeing the patient again for a comprehensive exam on the designated date. Encourage the patient to learn more about the office and the team by visiting the practice Web site, and urge the patient to call with any questions.
CONCLUSION
In stressful situations, people remember not necessarily what you did but rather how you made them feel. Nothing could be truer when caring for an emergency patient. Take steps to make sure you make your emergency patients feel good about your staff, your care, and their decision to choose your practice. Seize the teaching moments and watch your conversion rate increase significantly.
Sally McKenzie, certified management consultant, is a nationally known lecturer and author. She is CEO of McKenzie Management, which provides highly successful and proven management services to dentistry and has since 1980. McKenzie Management offers a full line of educational and management products, which are available on its Web site, mckenziemgmt.com. In addition, the company offers a vast array of practice enrichment programs and team training. Ms. McKenzie is the editor of the e-Management newsletter and The Dentist’s Network newsletter sent complimentary to practices nationwide. To subscribe, visit mckenziemgmt.com and thedentistsnetwork.net. Ms. McKenzie welcomes specific practice questions and can be reached toll free at (877) 777-6151 or at sallymck@mckenziemgmt.com.