Part 1 of this 2-part report focused on caries diagnosis and introduced treatment concepts using the modern paradigm for caries management.1 In the past, with the surgical paradigm, treatment was to drill and to fill. To cut was to cure. However, we were not curing. We were dealing with the macroscopic end-result effects of the process (the cavitation) and ignoring the microscopic cause of the cavitation (the bacterial caries process). We were treating caries as a lesion and not as a disease process. For modern treatment of caries, we must switch to a medical model and arrest and reverse the process. This article (Part 2) will present a practical protocol for managing caries.
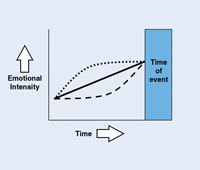
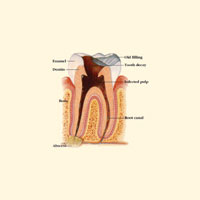
In Part 1, caries was defined using 2 criteria. First, caries is a bacterial infection caused by specific acidogenic bacteria in the tooth biofilm.2-8 Second, caries is a multifactorial process of tooth demineralization and remineralization, which until cavitation is reversible. Caries is the point at which the process of bacterial demineralization of tooth structure overwhelms the patient’s ability to remineralize tooth structure.9 It is a professional judgment. The factors in this process include bacteria and sugar levels (offense), salivary flow and salivary fluoride levels (defense), past dental history, and present medical status.10 The bacteria in the plaque on the intact tooth surface metabolize available sugar and produce acid. That acid penetrates the solid yet microscopically permeable tooth surface, driving calcium and phosphate out of the subsurface tissue, demineralizing it. The result is an initial white-spot lesion, which feels rough to explorer touch and appears chalky. The lesion progresses from the inside out until surface collapse (cavitation) occurs.
| Table 1. Risk Levels. |
|
• High-Risk Patient • Moderate-Risk Patient – Moderate risk factors
• Low-Risk Patient
|
Two features provide a diagnosis/prognosis leading to a treatment plan. Caries activity describes the process (demineralization or remineralization) on an individual tooth surface,11-13 while caries risk describes the status of the whole patient, defined as the likelihood of the patient getting a new cavitation (Tables 1 and 2). Combining these 2 features provides the basis for 7 groups of patients that we will discuss. Patients receive treatment using a medical model (Table 3) consisting of 4 steps:
| Table 2. Activity Analysis. | ||||||||||
|
|
Table 3. Treatment Plan Medical Model. |
|
1. Bacterial Control
2. Reduce risk level of at-risk patients 3. Reverse active sites/remineralization 4. Long-term follow-up and maintenance
|
(1) bacteria are controlled by using restorations (surgical approach/incision and drainage) and medications (chemotherapeutic combination of chlorhexidine, fluoride varnish, and xylitol gum); (2) risk levels of at-risk patients are reduced; (3) active sites are reversed by remineralization; (4) long-term follow-up and maintenance are performed at home and in the dental office.
TREATMENT BY RISK/ACTIVITY STATUS
We have now finished our quick review of the medical model for the treatment of dental caries. For a detailed look at the medical model and for references please refer to Part 1, which appeared in the February 2007 issue of Dentistry Today. Remember that the steps all flow together. Many of the individual parts can be done simultaneously.
So, how do we use this model to treat Mrs. Jones? The medical model gives us an overall conceptual framework. For any given patient, however, what is needed is a diagnosis/prognosis that can place her into a treatment group. By combining the 3 risk levels (Table 1) with the 2 caries activity states (Table 2) we get our 7 diagnosis/prognosis groups, which then become our 7 treatment groups. Each of these treatment groups has its own unique protocol. First let’s investigate the 7 treatment groups, which are listed in the left column of Table 4.First, there is the low-risk level (LR). This group will always be inactive.
Next, there is the moderate-risk level, which can be either active or inactive depending on the presence or lack of rough, chalky white spots. There are thus 2 moderate-risk treatment groups. In the presence of orthodontic brackets or xerostomia (moderate risk), but no rough, chalky white spots (activity), a patient would be classified as a moderate-risk inactive (MRI). If rough, chalky white spots are present, ie, a patient presents with activity, this patient would be classified as moderate-risk active (MRA). The MRA patient can present without any obvious risk factors. Upon closer investigation one or more risk factors can usually be identified.
We now come to the high-risk level, which can be broken down into 4 treatment groups. Remember that the high-risk patient has at least one cavitated lesion. We will assume in this article that the cavitated lesion is active. This gives us the high-risk active (HRA) category. If in addition to at least one cavity, a patient presents with rough, chalky white spots elsewhere, this patient will need more treatment than the high-risk active category. We will need to address the rough, chalky white spots in addition to any cavitations. Therefore, we have designated a second high-risk active category named high-risk active/active (HRA/A). We use the term active/active because of the 2 activities. The cavitation is active, and the rough, chalky white spot is active. There is a sixth category, high-risk inactive (HRI), which is for patients who have gone through the protocol and are not active any longer but need continued risk-reducing therapy. Patients are kept in this category for 3 years. Finally, for patients who present with 8 or more cavitated teeth, we have a category designated as very high risk (VHR).
As noted earlier, each of these treatment groups has its own unique protocol. By using the medical model and a treatment protocol table, we can decide upon the treatment for our Mrs. Jones.
Let’s look at the protocol. The column on the left in Table 4 lists the 7 treatment groups. The top row lists all of the individual parts of the treatment protocol. To identify which parts apply to any individual treatment group, identify the treatment group on the left column. Then follow along the row to the right and you will see the relevant protocol for that treatment group. A blank space means we do not use that treatment for that group. Numerals are used to represent the number of times treatment is repeated or the number of months involved. The details of the listed treatments have been covered in Part 1.
|
Table 4. Seven Treatment Groups. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
The actions listed on the top row of Table 4 are as follows: the first 3 items are fillings, temporary crowns, and sealants (surgical treatment). A “+” indicates that we do the listed treatment, while a blank box indicates that we do not apply that treatment. As we continue to the right, the next item listed is the number of fluoride varnishes applied when we first use this treatment (1 to 3 applications). The next item is the number of months that chlorhexidine rinse is used. Next is whether xylitol gum or GC America’s MI Paste or MI Paste Plus (fluoride added) is used. Continuing to the right, the next item shows in which month of the series of chlorhexidine treatments the CRT bacteria test (Ivoclar Vivadent) is administered. In the next column to the right the continuing care or recall interval in months is listed, followed by whether a fluoride varnish is done at that continuing care visit. Finally, we list the home fluoride protocol.
As you can see from Table 4, the low-risk patient requires a 6-month continuing care interval and regular over-the-counter toothpaste at 1,000 ppm. All this group needs is step 4 of the medical model. Remember, this is most of the patients in the average dental office.
The moderate-risk inactive group is treated with xylitol gum, MI Paste, or MI Paste Plus, a 6-month continuing care interval at which a fluoride varnish is applied, and 5,000-ppm toothpaste with 230-ppm rinses at home. This group receives care with step 2 and step 4 of the medical model. While this group does have risk factors, we have not as yet detected actual disease. This is, therefore, a preventive therapy group.
The moderate-risk active group is treated chemotherapeutically for the active disease process. After an initial fluoride varnish is applied, chlorhexidine is used once a day for one week per month for 6 months, and xylitol gum is used. You will recall this is step 1-B of the medical model (chemotherapeutic antimicrobial treatment). Step 1-A, surgical antimicrobial therapy (fillings), is unnecessary here as there are no cavitations. Steps 2, 3, and 4 follow. In Table 4 we see MI Paste (or MI Paste Plus) used for re-mineralization and the CRT test administered in month number 6. Continuing care/recall visits are every 3 months with a fluoride varnish treatment at each visit. Home care again consists of 5,000-ppm b.i.d. toothpaste and 230-ppm oral rinse during the day.
Recall that high-risk patients have at least one cavitation. As such they will need the entire medical model. High-risk active patients have at least one cavitation but no rough, chalky white spots. Beginning with surgical antimicrobial treatment (restorations) they are treated with fillings, temporary crowns, and sealants as needed. Since they have no active rough, chalky white spots we apply only one fluoride varnish at the first round of treatment. We use chlorhexidine for 6 months and xylitol gum to round out the chemotherapeutic antimicrobial treatment. Steps 2 and 4 follow. Notice that without the chalky white spots we do not need remineralization therapy. In Table 4 the rest of treatment can be seen as MI Paste (or MI Paste Plus), CRT test in month number 6, continuing care interval of 6 months, and a fluoride varnish at that continuing care visit. Home fluoride is as noted above.
High-risk active/active patients, in addition to at least one cavitated tooth, present with at least one rough, chalky white spot. They differ from high-risk active patients in that they do need remineralization therapy. They get the entire medical model. Looking at Table 4 one can see that they differ from high-risk active patients in only 2 respects. They get 3 fluoride varnishes at the first round and the continuing care interval is 3 months.
Let’s move to the very high-risk group. They get the entire medical model, intensified. Due to the risk of increased bio burden, all surfaces are sealed, including those with amalgams. Three fluoride varnishes are given in the first round. Chlorhexidine is used for 12 months, and the CRT test is administered at the end of that period of time. Continuing care is 3 months with fluoride varnish applied. Home fluoride is 5,000-ppm paste in a tray once a day and by toothbrush once a day in addition to rinses. Due to the high risk, a custom fluoride tray is used to ensure the best exposure of the surfaces of the teeth to fluoride.
Finally let’s look at the high-risk inactive group. This is the only high-risk group that does not have cavitations. This is a special group for patients who have been high risk and have gone through initial therapy and are presently inactive. They are, however, at increased risk for several years due to their history. With this group we want to prevent the return of the disease process. Notice that their protocol is exactly the same as the moderate- risk inactive group. This points out something very important in the new paradigm of caries management. We must take care to use precise terminology. We are confusing prevention and therapy. Prevention is before disease occurs. Therapy is after disease occurs. There has been a major shift.
In the past, prevention referred to preventing cavitations. Treatment consisted only of treating existing cavitations surgically (restorations). Now, we are preventing demineralization (fluoride, MI Paste or MI Paste Plus, xylitol). We are also treating existing demineralization chemotherapeutically, ie, by remineralization (fluoride, chlorhexidine, MI Paste or MI Paste Plus, xylitol). After remineralization or surgery, we once again try to prevent further demineralization (fluoride, MI Paste or MI Paste Plus, xylitol).
Notice that the medications used are virtually the same regardless of the purpose for which they are being used. This can introduce some confusion in our terminology. We are not remineralizing using preventive modalities. We are remineralizing using therapeutic modalities (chemo-therapeutics), even though 3 out of the 4 medicines are also used for prevention purposes. It is important to understand we have moved caries treatment to an earlier stage. We are no longer focused on cavitation; we are focused on demineralization as the key factor. We want to prevent demineralization in the first place (moderate-risk inactive patient). If demineralization (ie, the caries process) begins, then we treat the demineralization with remineralization and risk-reduction chemotherapeutics. If demineralization has led to cavitation, then we add restorative therapy. Then we prevent redemineralization (high-risk inactive patient). Now that is a paradigm shift!
CONCLUSION
This paradigm builds on the success the dental profession has had in the past. More importantly, it enables us to improve our understanding of the caries disease process. With this new understanding we are focusing on prevention and treatment of caries at an earlier stage than ever before. We’ve also developed protocols enabling us to treat higher risk patients effectively. These protocols can be implemented in any dental practice.
References
- Steinberg SC. A modern paradigm for caries management, part I: diagnosis and treatment. Dent Today. Feb 2007;26:134-139.
- Loesche WJ. Chemotherapy of dental plaque infections. Oral Sci Rev. 1976;9:65-107.
- Tanzer JM, Livingston J, Thompson AM. The microbiology of primary dental caries in humans. J Dent Educ. 2001;65:1028-1037.
- Caufield PW. Dental caries—a transmissible and infectious disease revisited: a position paper. Pediatr Dent. 1997;19:491-498.
- Tanzer JM. Dental caries is a transmissible infectious disease: the Keyes and Fitzgerald revolution. J Dent Res. 1995;74:1536-1542.
- Anderson MH, Molvar MP, Powell LV. Treating dental caries as an infectious disease. Oper Dent. 1991;16:21-28.
- Tinanoff N, Cantin R. Management of dental caries as an infectious disease. ASDC J Dent Child. 1986;53:359-363.
- Loesche WJ. Dental Caries: A Treatable Infection. Springfield, Ill: Charles C. Thomas; 1982.
- Jenson L. UCSF clinical guidelines for managing caries by risk assessment. Presented at: 7th Annual World Congress of Minimally Invasive Dentistry; August 19, 2006; Seattle, Wash.
- Reich E, Lussi A, Newbrun E. Caries-risk assessment. Int Dent J. 1999;49:15-26.
- Zero DT. Application of clinical models in remineralization research. J Clin Dent. 1999;10:74-85.
- Nyvad B, Fejerskov O. Assessing the stage of caries lesion activity on the basis of clinical and microbiological examination. Community Dent Oral Epidemiol. 1997;25:69-75.
- Nyvad B, Machiulskiene V, Baelum V. Reliability of a new caries diagnostic system differentiating between active and inactive caries lesions. Caries Res. 1999;33:252-260.
Dr. Steinberg received his DDS degree from the University of Illinois College of Dentistry. He completed a general practice residency at the University of Illinois and West Side Veterans Administration hospitals. An externship in geriatric dentistry was completed at the Long Island Jewish Hospital in New York. Dr. Steinberg practiced dentistry in Illinois from 1982 to 2005. He is currently a clinical consultant for the University of Illinois College of Dentistry Continuing Education Online course on dental caries. He was director of the Ark Dental Clinics in Chicago and currently serves on that organization’s board of directors. He is available to speak to groups large and small. He can be reached at (847) 800-5918, ssov@comcast.net, or by visiting cariesspeaker.com.
Disclosure: Dr. Steinberg has a paid lecture sponsorship with GC Am