 |
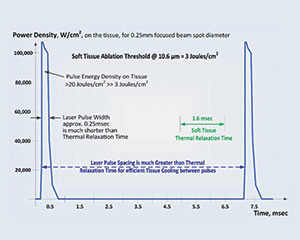
| Graph. SuperPulse explained: high-power, short laser-pulse duration maximizes soft-tissue removal rate and keeps adjacent tissue cool. (Courtesy of LightScalpel). |
INTRODUCTION
The plethora of high-tech dental instruments requires a disciplined evaluation prior to purchase and implementation. Instruments such as lasers, piezosurgical devices, CBCT, and so on, used to be relegated to a few offices. However, as studies elucidate the benefit/risk ratios, return on investment (ROI), and increased efficiency and better outcomes, practitioners are purchasing advanced technology and experiencing better results.
Background
Lasers have uses based upon the wavelength selected. Soft-tissue lasers are instruments that cut, coagulate, and provide hemostasis. When laser light interacts with cells intracellularly in the 10,000-nm spectrum (CO2 lasers), the water contained in the cells heat up and, because scatter of the laser light is low and absorption is high, the cells that are photo initiated will vaporize.1 Since the coagulation/hemostasis depth at CO2 laser wavelength just slightly exceeds the diameters of the gingival blood vessels, coagulation extends into a blood vessel to stop bleeding and does not extend excessively into the margins of the cut.1
With the ability to SuperPulse, the LightScalpel laser allows for the laser energy to be interrupted, allowing for a tissue relaxation time to avoid charring tissue and preventing tissue necrosis from prolonged irradiation. The tissue being treated can be excised/incised most efficiently when the laser pulse time is much shorter than the thermal relaxation time or SuperPulse mode (Graph).2
In selecting a CO2 laser versus a diode laser, the research is conclusive. At diode wavelengths around 1,000 nm, light scattering dominates the very weak absorption. When diode lasers are used, they do not cut optically. Instead, the glass tip of the diode fiber is charred and heats up to between 500°C to 900°C via heating of the char by the diode laser light. The hot charred/activated glass tip burns the soft tissue on contact. Dental diodes do not cut the tissue with photons, but with hot charred glass! The device that is closest to a diode that cuts on the same thermomechanical principle is electrocautery.1-3 Therefore, diodes are thermal contact ablation devices and not laser wavelength-dependent precise cutting instruments.1,3
Advantages of CO2 laser surgery include reduced scarring and wound contraction, minimal postoperative swelling, and edema; this is due to closure of lymphatic vessels, decreased lateral tissue destruction, and faster healing times with less postoperative pain.4 Additionally, the SuperPulse CO2 laser wavelengths allows for superficial ablation of bacterial biofilms, which is an important modality for extraction site decontamination.4-6
The following case studies will serve to highlight how the CO2 laser (10,600-nm LightScalpel) has been successfully integrated into my practice.
CASE 1
Extraction Site Decontamination, Ovate Pontic Development, and Hemostasis
In order for the switch to occur from electrosurgical procedures to laser-assisted procedures, there had to be a better patient experience and tangible benefits as a result of implementing this technology.
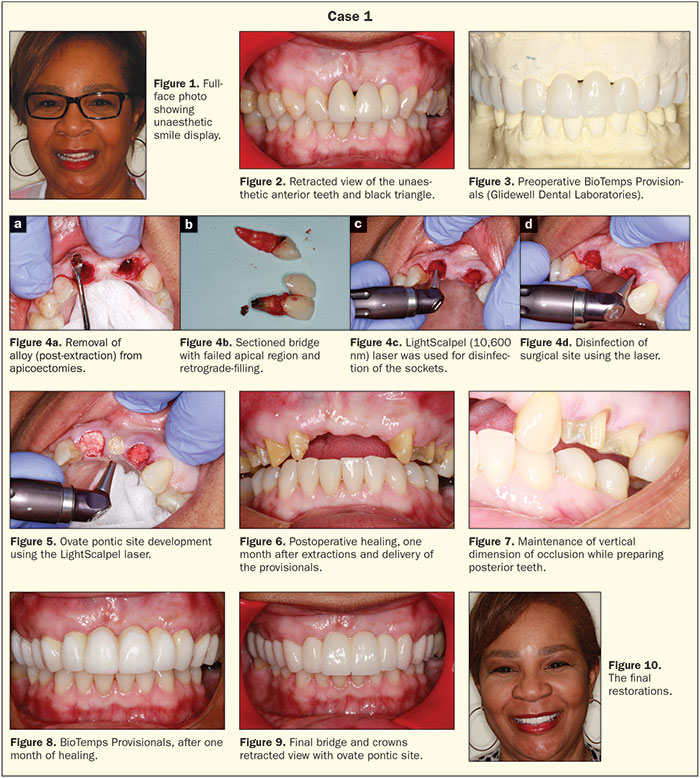 |
In this case, a woman was unhappy with her porcelain-fused-to-gold bridge (fixed partial denture [FPD]). This FPD was failing due to fracture of the abutment teeth and the development of an unaesthetic black triangle that was a result of failed endodontics and scar tissue from previous apicoectomies (Figures 1 and 2). BioTemps Provisionals (Glidewell Dental Laboratories) were fabricated to re-establish canine guidance and to guide soft-tissue remodeling prior to the fabrication of a new bridge and crowns from teeth Nos. 3 to 12. (Glidewell Dental Laboratories) (Figure 3). It should be noted that implants and block grafting were discussed with the patient and, with less than ideal space for placement of 2 implants, the patient chose the FPD option.
The existing FPD was sectioned and the laser was used for sulcular incisions around the teeth. The Physics Forceps (Golden Dental Solutions) was used to atraumatically remove the teeth; the proper use of this unique forceps allows the clinician to keep the buccal plate intact when extracting teeth. The laser was then used to remove granulation tissue within the sockets and to free any tissue from the bone as periapical lesions and cysts were present.
The sockets were carefully debrided and the old alloy was removed from the apicoectemy sites (Figures 4a and 4b). The sockets were decontaminated with the CO2 LightScalpel laser and ovate pontic site were developed (Figures 4c, 4d, and 5). Socket grafting was done using Foundation (J. Morita USA), and the soft tissue would be allowed to mature prior to the fixed prosthetic stage of the rehabilitation.
Upon removal of the BioTemps Provisionals at one month, the tissues were matured and keratinized tissue was present (Figure 6). The canines were not previously prepared to maintain the vertical dimension of occlusion; they were prepared at this juncture in the treatment sequence utilizing segmented Blu-Mousse (Parkell) bite registrations (Figure 7). The occlusion was controlled in the provisionals and canine guidance was achieved as well as guided tissue sculpting to recreate papillae (Figure 8). Approved occlusal construct and guidance was communicated to the dental laboratory team by making impressions of the approved provisionals so that a custom anterior guide table could be fabricated. The healed tissues at 1.5 months post-extraction, as well as the definitive porcelain restorations, elucidated the biologic symmetry and lack of black triangle. Idealized height to width ratios the patient had enjoyed in the well-crafted wax-up and BioTemps provisional restorations were also realized (Figures 8 to 10).
CASE 2
Implant Uncovery and Tissue Recontouring Around LOCATOR Attachments
This case involved a patient with partial edentulism who requested a LOCATOR Attachment (Zest Dental Solutions) overdenture. After evaluating her Panorex radiograph, and using barium sulfate markers in her treatment partial to locate the implant positions, the implant positions were transferred intraorally (Figure 11). Implants (BioHorizons) were placed to establish a stable base for the overdenture because she could not afford to place additional implants at that point in time (Figure 12). The concept of upgradeable dentistry (a term coined and used by the author that refers to dentistry done in preplanned stages as the patient can afford it) was explained to the patient.6 The future plan was to add implants, via CBCT guided implant surgery, to convert her case to a fixed detachable hybrid prosthesis.
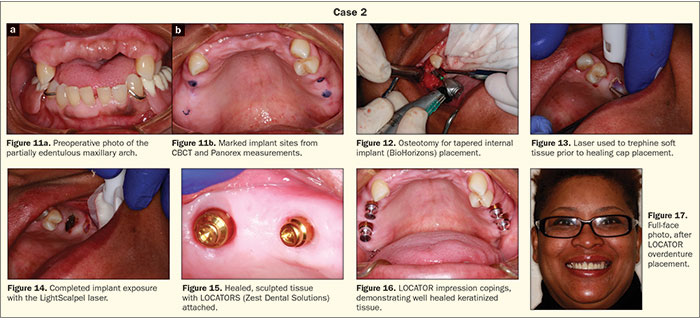 |
The implants healed uneventfully and plenty of keratinized tissue allowed for laser soft-tissue removal at the LOCATOR Attachment appointment. The LightScalpel laser was used to trephine the soft tissue while creating hemostasis and avoiding tissue necrosis (Figures 13 and 14). At the same time, the tissue was thinned, and a positive tissue architecture was sculpted to create even tissue thickness surrounding the LOCATORS and to assist the patient in keeping the areas clean (Figures 15 and 16). The postoperative full-face view with the metal-reinforced LOCATOR overdenture can be seen in Figure 17.
CASE 3
Crown Lengthening Using Laser
This patient presented with a fractured mesio-palatal cusp of an upper first molar. She did not wish to undergo extraction; socket preservation; and an implant, abutment, and crown procedure (Figure 18). While rescuing this tooth may be considered a compromised treatment, the patient wished to try to salvage her tooth. Since authors may talk about closed laser crown lengthening, it is this author’s contention that, if you can’t see and measure the true amount of bone removal and ensure that there is no root damage, then it is a blind procedure that could lead to less-than-ideal results. After achieving local anesthesia, the laser was used to remove excess soft tissue to allow for hemostasis and direct visualization of the fracture (Figure 19). The presets on the laser can all be customized; however, the presets for soft tissue removal, sulcular debridement, etc, are very accurate starting points. Next, a 170 XXL bur (Salvin Dental) was used to remove 4.0 mm of bone to allow for a 2.0 mm biologic width; the bone was feathered to allow for a positive bony architecture (Figure 20).
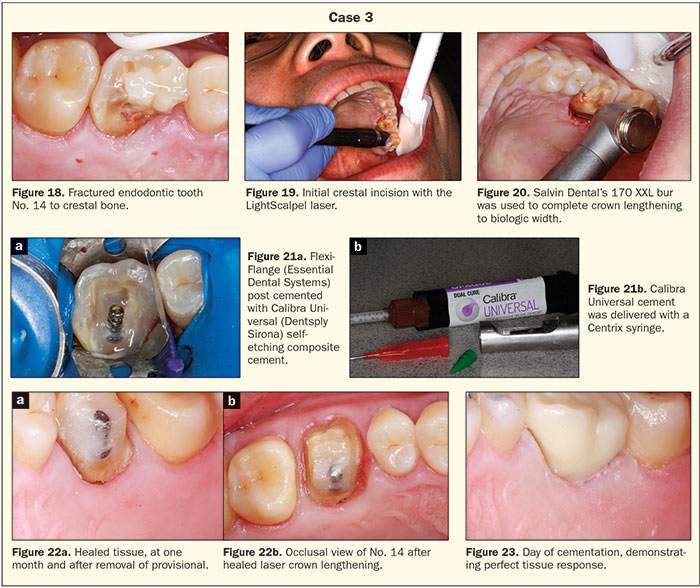 |
Endodontic therapy was performed, and the crown lengthening made the retention of the rubber dam retainer possible. A Flexi-Flange post (Essential Dental Systems) was used and cemented with a dual-cured self-etching resin cement (Calibra Universal [Dentsply Sirona]) that bonds with excellent strengths to both deep dentin and enamel (Figure 21). Prime&Bond Elect (Dentsply Sirona) was used as the bonding agent. Then, SureFil SDR (Dentsply Sirona) flowable composite resin was used to adapt to the surface of the post. TPH Spectra Universal Composite Restorative HV (Dentsply Sirona) was used to incrementally build up the tooth prior to crown preparation. The stress decreasing resin in SureFil SDR, along with the high adaptability of the TPH Spectra, make for an ideal crown build-up protocol (Figure 22). After crown provisionalization for one month, the final monolithic zirconia crown (BruxZir [Glidewell Dental Laboratories]) was cemented (Calibra Universal) (Figure 23).
CASE 4
Rescuing Teeth Versus Extraction
The last case illustrates a situation of a patient waiting years to crown endodontically treated teeth but has limited finances. In these cases, sometimes our goal should be to rescue the tooth to preserve bone for the placement of implants at a later time (Figure 24).
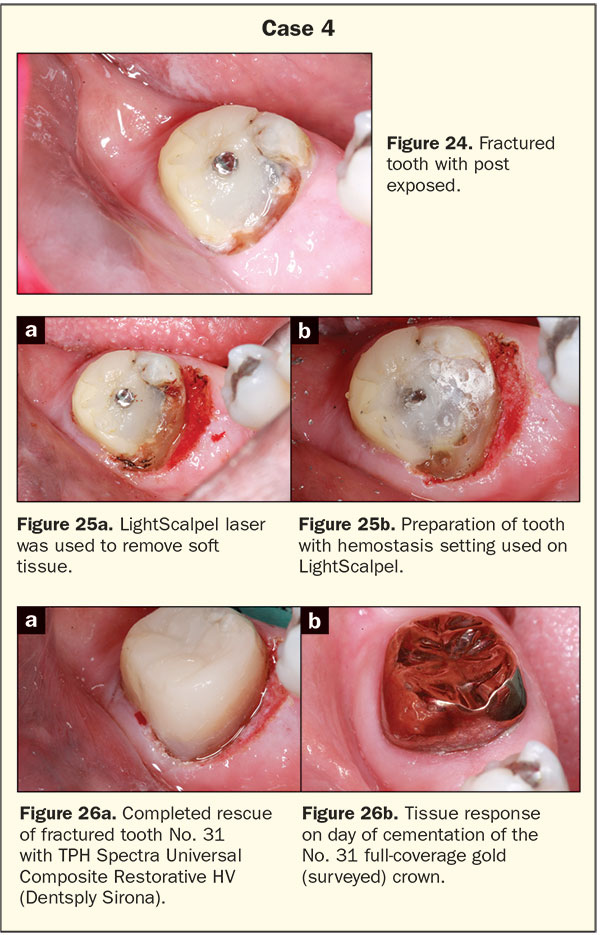 |
While this patient did not have the financial resources to remove this second molar and place an implant, he understood the value of bone preservation. Saving the bone at this point would allow for simplified implant treatment later if the patient’s finances improve. The LightScalpel was used to remove the hypertrophic tissue and allow for a positive emergence angle for the composite repair (Figure 25a). The post had been extending to the occlusal surface, which created a concentrated stress point and potential fracture vector. The post was ground down, tissue was feathered with the laser soft-tissue cutting setting, and then the hemostasis setting with a 0.4-mm laser spot size was used to coagulate the tissues and leave a bloodless field for the composite repair (Figure 25b). The repaired tooth highlights the respect that was paid to the periodontium through conservative laser crown lengthening which translated to a full gold surveyed crown with excellent margins, emergence angle, and profile (Figure 26).
CLOSING COMMENTS
These cases—along with frenectomies, soft-tissue lesion removal, removal of fistulas, peri-implantitis treatment, biopsies, and preprosthetic removal of hyperplastic tissue—are procedures that I have performed with the LightScalpel 10,600-nm laser.
While most articles on technology focus on the dollars and cents of the ROI, and these are important topics (worth mentioning is LightScalpel 10,600-nm laser is priced at a third of the price of its 9,300-nm competitor), this article focused on the scientific choice of a CO2 versus a diode and how it has allowed for a more comfortable and faster healing experience for my patients. The addition of procedures and efficiency of hemostasis highlights advantages to integration of this technology in a general dental setting.
References
- Levine R, Vitruk P. Laser-assisted operculectomy. Compend Contin Educ Dent. 2015;36:561-568.
- Fisher JC. Basic laser physics and interaction of laser light with soft tissue. In: Shapshay SM, ed. Endoscopic Laser Surgery Handbook. New York, NY: Marcel Dekker; 1987:96-125.
- Romanos GE. Diode laser soft-tissue surgery: advancements aimed at consistent cutting, improved clinical outcomes. Compend Contin Educ Dent. 2013;34:752-757.
- Lambrecht T, Stübinger S, Hodel Y. CO2 laser therapy for intraoral hemangiomas. Journal of Oral Laser Applications. 2004;4:89-96.
- Cobb CM, Vitruk P. Effectiveness of a super-pulsed CO2 laser for removal of biofilm from three different types of implant surfaces: an in vitro study. Implant Practice US. 2015;8:20-28.
- Winter R. Upgradeable dentistry: Part 1. Dent Today. 2009;28:82-87.
Suggested Readings
Catone GA, Alling CC. Laser Applications in Oral and Maxillofacial Surgery. Philadelphia, PA: WB Saunders; 1997.
Convissar RA, Massoumi-Sourey M. Recurrent aphthous ulcers: etiology and laser ablation. Gen Dent. 1992;40:512-515.
Schwarz F, Sahm N, Iglhaut G, et al. Impact of the method of surface debridement and decontamination on the clinical outcome following combined surgical therapy of peri-implantitis: a randomized controlled clinical study. J Clin Periodontol. 2011;38:276-284.
Zeinoun T, Nammour S, Dourov N, et al. Myofibroblasts in healing laser excision wounds. Lasers Surg Med. 2001;28:74-79.
Dr. Winter graduated from the University of Minnesota School of Dentistry. He holds a Mastership in the AGD; is a Diplomate in the American Board of Oral Implantology/Implant Dentists and the International Congress of Oral Implantologists; and is a Fellow in the American Academy of Implant Dentists, the International College of Dentists, and the Academy of Dentistry International. He lectures on advanced treatment planning, general dentistry as a specialty, and upgradeable dentistry and has published articles on advanced reconstructive implant and cosmetic rehabilitation. For information on his lectures and hands-on courses, email rick@winterdental.com or visit his website at hamptondentalassociates.com.
Disclosure: Dr. Winter reports no disclosures.
Related Articles
Rehabilitation of Mandibular Atrophy: The Case of the Prolonged Partial
Compromised Foundations Require Confident Conversation











