INTRODUCTION
A patient enters your practice looking unhappy and says she’s ashamed to smile. Do you immediately ask to see her teeth and possibly comment on them? You have a choice to make. In this author’s opinion, the most important thing to do when a patient enters a practice is to begin creating a relationship with the patient. Experience tells me case acceptance is directly related to knowing the patient’s goals for his or her mouth, building trust with the patient, and helping him or her feel understood.
Background
This patient previously had a full-mouth rehabilitation done elsewhere and said, “I’m unhappy with the way my teeth look” (Figures 1 and 2). I didn’t say “Let me see your teeth,” but rather asked if it would be okay to ask her some questions. Getting permission to ask questions changes the doctor-patient dynamic and levels the playing field between doctor and patient, as if to say to the patient, “We’re in this project together.” The patient begins to know he or she is important, and in the many years I’ve asked that question, I never had a patient reply “No.” I needed to find out what she meant by “unhappy with the way my teeth look” and patiently listened to her answers.

Figure 1. Preoperative retracted view.

Figure 2a. Pre-op right lateral view. Figure 2b. Pre-op left lateral view.
My questions were not simply “yes” or “no” questions. Instead, they were designed to find out what she liked and disliked about her smile. I also asked her, “How do you think you’d feel if you were happy with your smile?” Notice the key words have to do with emotions. This dialogue with a patient can also create a sense of hope.
Another important technique in the initial interview is scaling. While it has the same name as the periodontal procedure, it is a way of finding out the strength of the emotions the patient described. I asked, “On a scale of 1 to 10, with 1 being slightly unhappy and 10 being so unhappy with your smile that you cover your mouth or refrain from smiling completely, what number would you give it?” She said “10!”
I had not examined her yet, and she remarked that she already felt better being in my office. In this author’s opinion, knowing more about a patient as a person, and not simply as a mouth to rehabilitate, is critical. We spoke about her hobbies, her family, where she grew up, etc. She did most of the talking, and I did more of the listening. In a short amount of time, we were able to establish a relationship that led to building trust, an essential ingredient for happy patients and practice growth. Finally, I said, “Let’s take a look at your situation.”
CASE REPORT
Examination included oral cancer screening, including a VELScope (LED Dental) subsurface tissue survey, TMJ palpation, appropriate x-rays, impressions for diagnostic models with Silganat alginate substitute (Kettenbach LP), and bite registration with O-Bite (DMG America). Models were poured with COECAL stone (GC America) and mounted on a hinge articulator. Existing restorations, periodontal pocket measurements, and restorations I thought she needed for function and appearance were noted in her record. Photographs, including portraits and intraoral images (Figure 3), were made using a Canon/PhotoMed Clinical System (PhotoMed International).
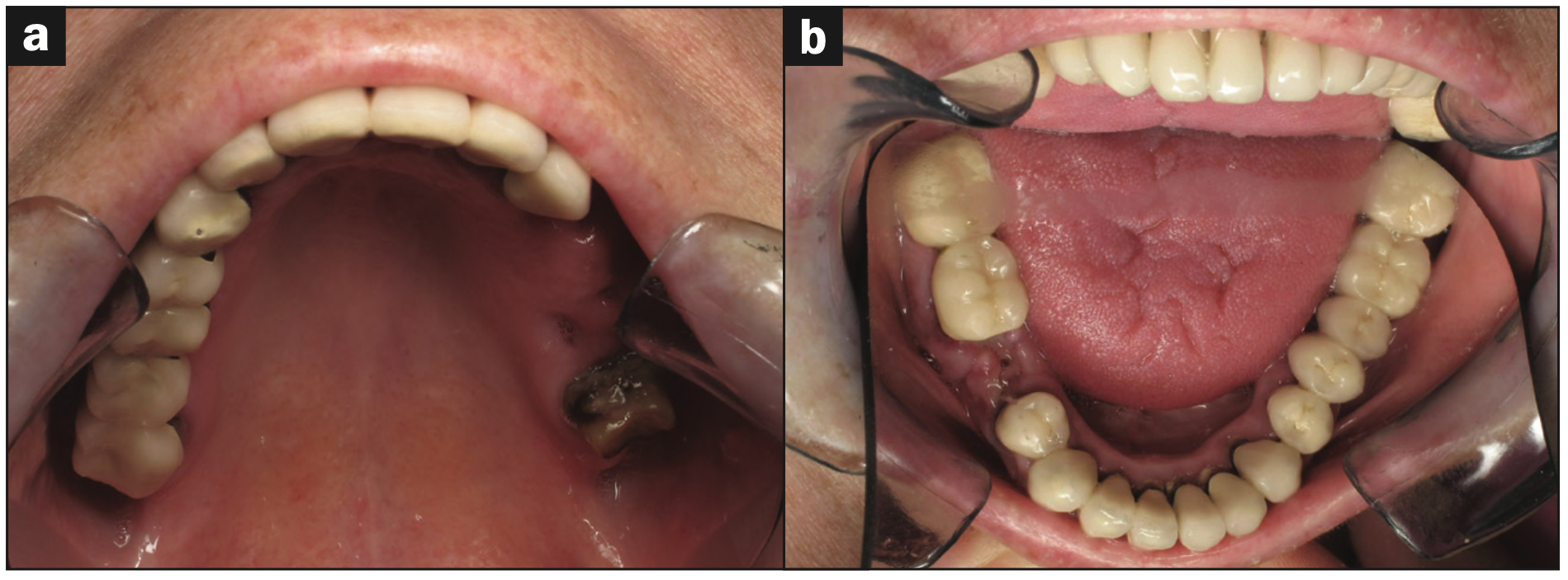
Figure 3a. Pre-op upper arch occlusal view. Figure 3b. Pre-op lower arch occlusal view.
Prior to our next visit, I had a treatment plan consultation with my laboratory technician.1 For full-mouth rehabilitation cases, I find it helpful to speak with my technician prior to presenting treatment plans to patients. There can be technical aspects and challenges with the fabrication of restorations I might not see. The goal was to bring the patient back to a healthier state and give her a smile she could enjoy and be proud of. My laboratory was a critical partner in achieving this goal.
At a subsequent visit, we discussed a plan, and all patient questions were answered. She understood that there were some problems that could appear as we moved forward because I couldn’t know what might lay under her existing crowns. The plan included potential root canals, posts, cores, extractions, and implants and a potential sinus lift. Approximate costs were presented only for what I knew I’d have to do. The approximate costs for treatment that could become necessary would be determined sometime in the future. She acknowledged that she understood and looked forward to our next treatment conversation to update her after all her old crowns were removed and her teeth were temporized.
Treatment Plan
We planned to restore her dentition with PFM crowns and bridges in most areas. A semi-precision interlock between teeth Nos. 5 and 6 was suggested by my lab technician, Steve Killian, CDT (Killian Dental Ceramics, Irvine, Calif). Broken-stress measures serve as “safety valves” against the tremendous leverage forces created by the rigid attachment to 2 or more teeth.2,3 Further, a rigid connector may not be an ideal choice due to differences in the physiological tooth movement of different teeth. Curvature of the arch, the facio-lingual movement of an anterior tooth, occurs at a considerable angle to the facio-lingual movement of molar teeth. These movements can create stress on the abutments in long-span prostheses. Some means must be used to neutralize the effects of these forces.4
Lithium disilicate IPS e.max (Ivoclar Vivadent) crowns were planned for the lower incisors. Implants and a fixed bridge in the upper left quadrant were planned using 2 implants and tooth No. 15 as abutments. As we moved forward, we’d find out what else might be needed.
Chairside
All upper restorations were resected with coarse #850-016 Piranha diamonds (SS White Dental) for the porcelain and Great White #2 Gold Series carbides (SS White Dental) for the metal. The existing crowns and bridges were then removed with a Wynman Crown Remover (Integra Miltex). Tooth No. 7 was no longer savable and was extracted. Immediately after extraction, a BioTemps bridge (Glidewell) was relined to fit the preparations and cemented with GC TEMP ADVANTAGE (GC America). A piece of fibrous tissue remained on the buccal of the No. 7 edentulous area several months later. A reduction guide typically used for tooth preparations was created for the excess fibrous tissue and was placed to remove the fibrous tissue with a Microlaser NV (DenMat) (Figures 4 and 5).

Figure 4. Reduction guide for fibrous tissue removal.

Figure 5. Tissue removed with an NV Laser (DenMat).
The lower arch was treated with PFM bridges in the posteriors. Teeth Nos. 23 to 26 were prepared for the IPS e.max crowns using a Piranha diamond #856-018 (SS White Dental). The closest stump shade was provided to the lab with a photo (Figure 6) so the technician could see any differences between the shade tab and the actual preparations. An impression was made using Identium Medium Body and Light Body (Kettenbach LP). Traxodent (Premier Dental) (Figure 7) retraction paste was used prior to impressioning. The final mandibular full-arch rehabilitation is seen in Figures 8 and 9.

Figure 6. Ivoclar Stump Shade Guide for IPS e.max restorations (now called IPS Natural Die Material shade guide).

Figure 7. Traxodent (Premier Dental) prior to placing compression caps.

Figure 8. IPS e.max crowns bonded in with Panavia V5 (Kuraray Noritake Dental) immediately postoperatively.
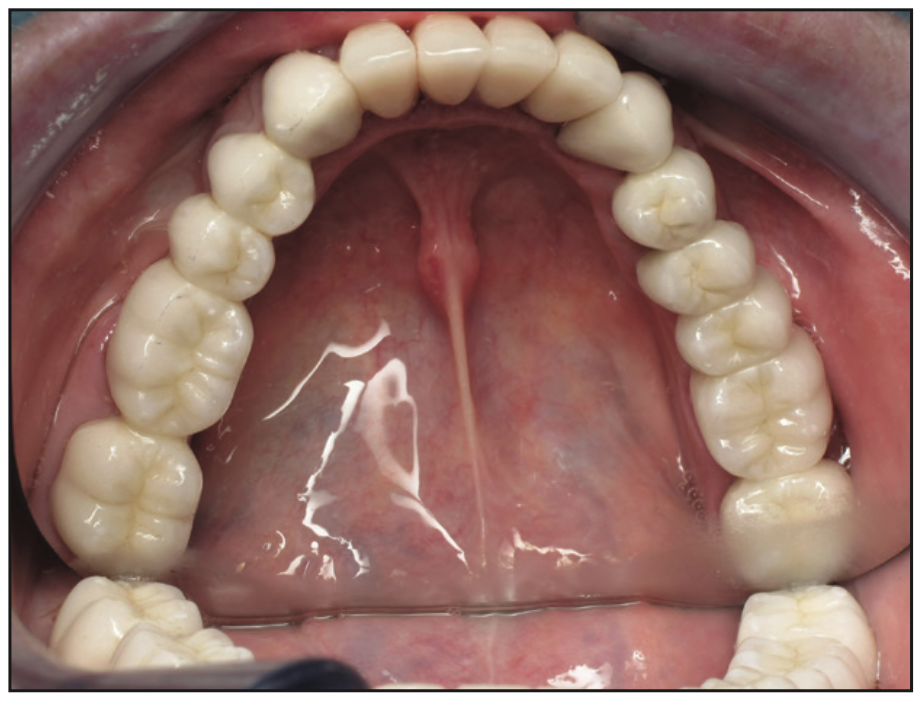
Figure 9. Lower arch rehabilitation post-op.
The upper bridge frame from Nos. 2 to 11 was tried in for fit and occlusal clearance, and the interlock between Nos. 5 and 6 was evaluated (Figure 10). A bite registration was made with O-Bite (DMG America), and a counter lower arch impression was made with StatusBlue (DMG America).

Figure 10. Try-in of 2-section frame with a semi-precision interlock.
The final upper rehabilitation from Nos. 2 to 11 was inserted with GC Fuji PLUS resin-modified glass ionomer cement (GC America) (Figure 11). A new interim partial with prosthetic teeth on the upper left was inserted to use until implants were placed and ready for restoration in the Nos. 12 and 13 areas.
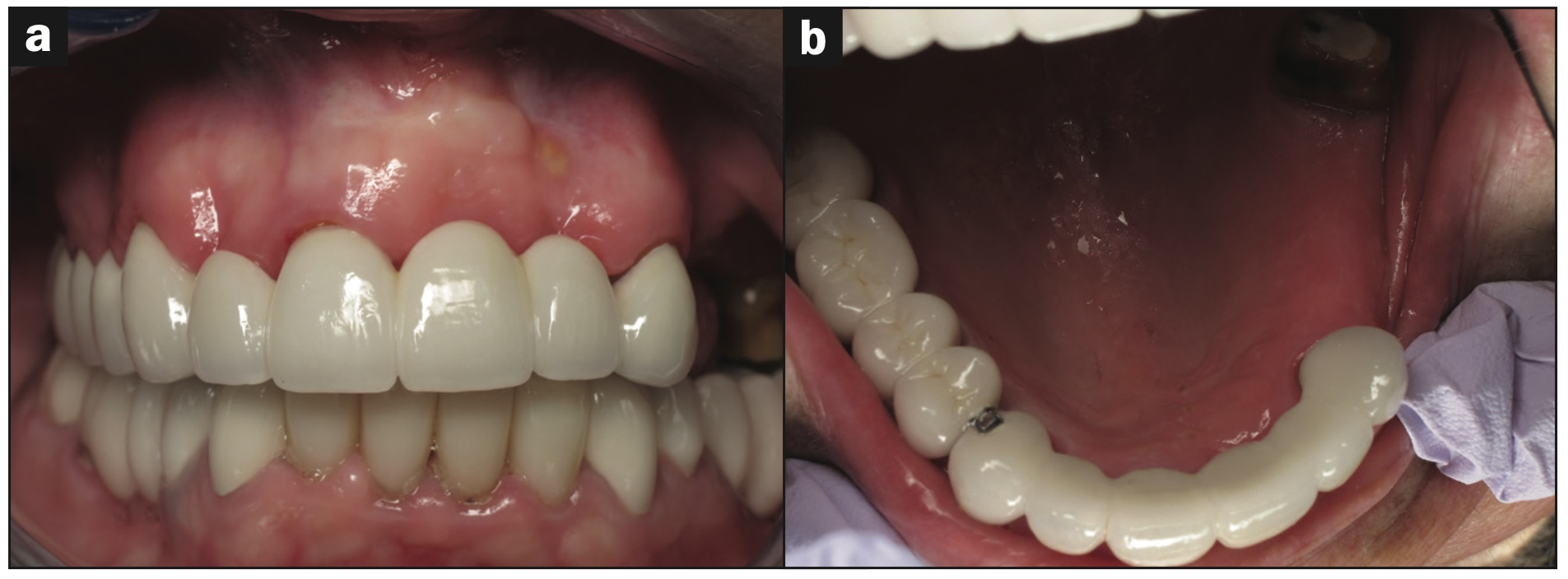
Figure 11a. Upper arch ready for implant placement in upper left bicuspid region. Figure 11b. Upper arch rehabilitation prior to implant placement in the Nos. 12 and 13 areas.
Sadly, a few weeks later, the patient fell face-forward, and the blunt force trauma fractured much of the porcelain over the Nos. 6 to 8 area (Figure 12). The patient was told it was improbable that a repair would work due to the seriousness of the fracture. Nevertheless, she asked me to try to fix it. I tried to remove the fractured porcelain and restore it with CLEARFIL Universal Bond Quick (Kuraray Noritake Dental) and CLEARFIL MAJESTY ES-2 composite (Kuraray Noritake Dental). After multiple attempts over several visits, it was clear the patient would need a new bridge from Nos. 6 to 11. Fortunately, the rest of the arch was preserved: The semi-precision interlock saved us. Finally, Nobel Replace Select Implants (Nobel Biocare) were placed in areas of Nos. 12 and 13 and covered to integrate.
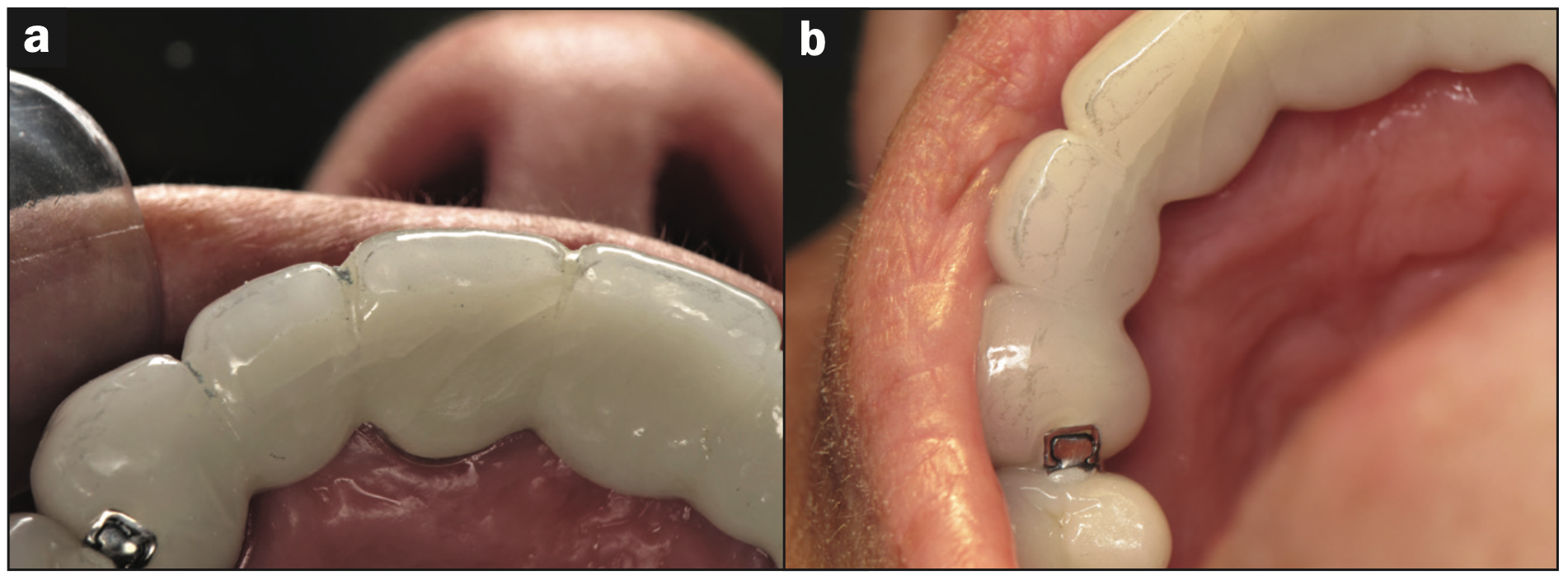
Figure 12a. Blunt force trauma caused major fracture in the porcelain of the Nos. 6-to-11 bridge. Figure 12b. Blunt force trauma caused major fracture in the porcelain of the Nos. 6-to-11 fixed bridge.
Within 3 months, our patient took ill and had an extended hospitalization for several months. During that time, she lost bone around the fully integrated Nos. 12 and 13 implants (Figure 13), leaving some threads on the implants exposed. A second new interim partial made of Lucitone 199 (Dentsply Sirona) and wrought wire clasps was fabricated to fit over the exposed implants and the No. 14 prepped tooth (Figures 14 and 15).
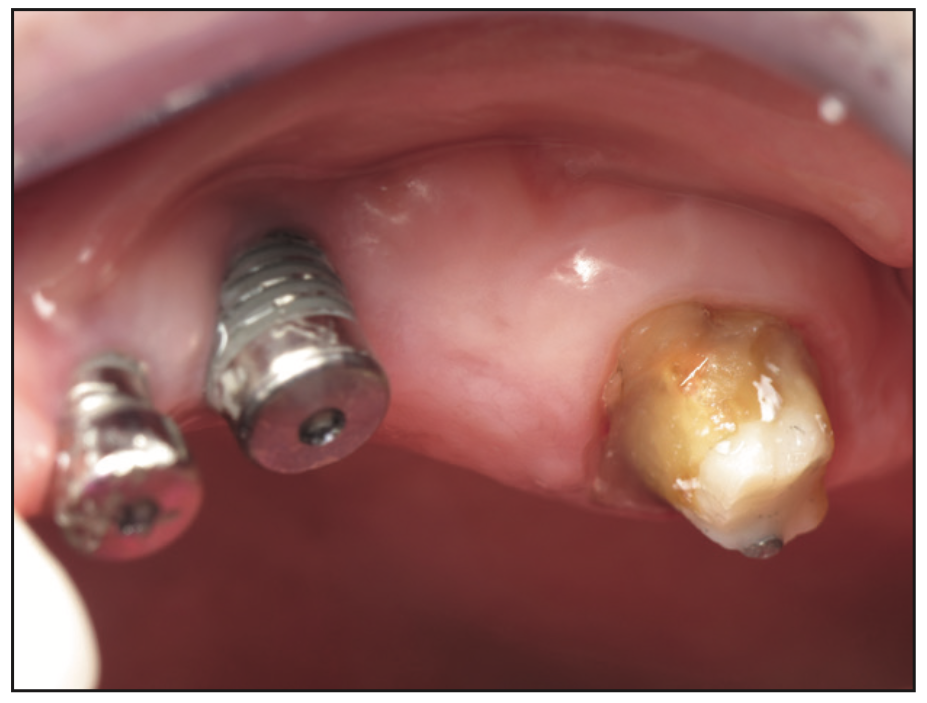
Figure 13. Nobel Biocare implants with healing caps after prolonged medical problems and hospitalization.

Figure 14. Lucitone 199 (Dentsply Sirona) flipper to be worn over healing abutments with exposed threads.

Figure 15. Post-op photo with new interim partial inserted.
An impression was made with Identium Medium and Light Body for a fixed bridge from Nos. 12 to 15 to be supported by 2 implants and a natural tooth. Although this wasn’t my first choice, the situation dictated that this was the best treatment option. The bridge was returned and fitted using Occlude Aerosol Marking Spray (Pascal Company) (Figure 16). Gingival embrasures of the bridge were refined to make them cleansable and polished with Dialite Knife Edged Discs (Brasseler USA) (Figure 17). Waxed dental floss (Oral-B Glide [Procter & Gamble]) loops with slipknots were placed in the embrasures to facilitate cement removal after seating the bridge (Figure 18). It would be easy to open the slipknot with an explorer and then run the floss buccolingually, ensuring no cement was left behind. The bridge from Nos. 12 to 15 was cleaned with a MicroEtcher IIA (Zest Dental Solutions), and the cementation was done with Panavia V5 (Kuraray Noritake Dental).

Figure 16. Fitting the upper left bridge with Occlude Aerosol Marking Spray (Pascal).
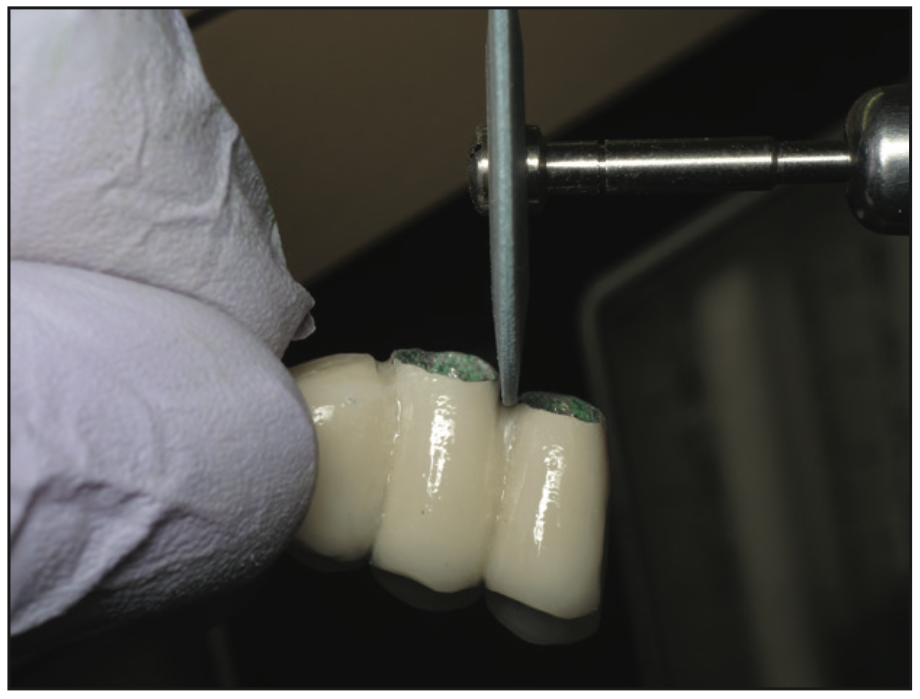
Figure 17. Polishing gingival embrasures with Dialite discs (Brasseler USA).
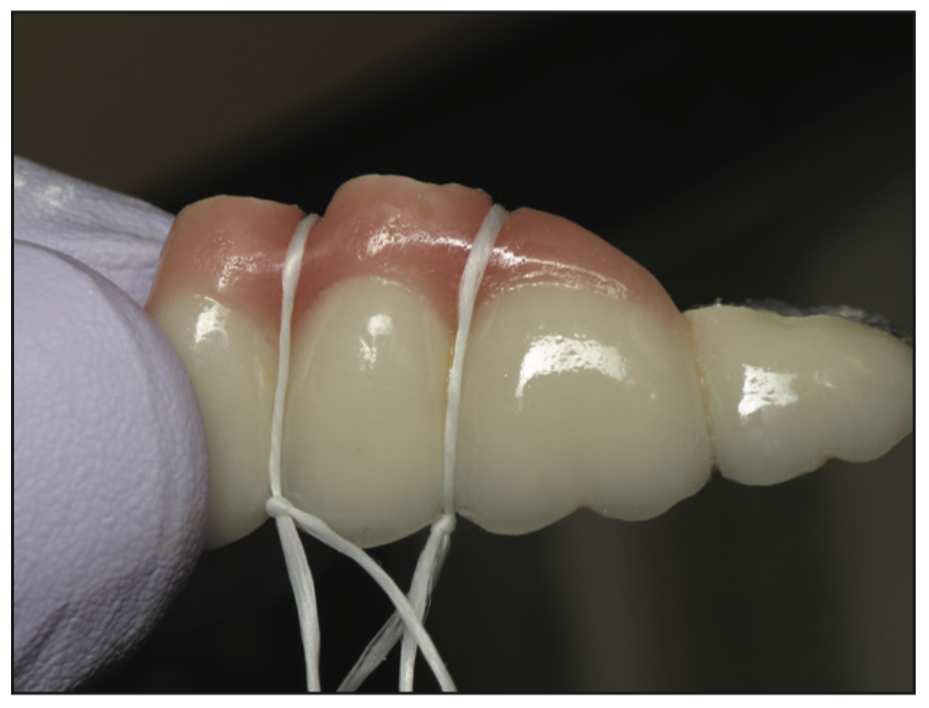
Figure 18. Slipknot loops to facilitate embrasure cement cleanup.

Figure 19. Final post-op photo.
Tooth vs Tooth and Implant-Supported Bridge
There has been much discussion and no consensus about cementing fixed bridges that are tooth- and implant-supported. Frank Spear said that whether or not it is acceptable to connect an implant to a tooth or teeth in a restoration is one of the most misunderstood areas of implant dentistry. The reason so much confusion exists is simple: There isn’t one correct answer. With the risks of overloading the implant and intrusion of the teeth, it would seem reasonable to ask why you would want to connect an implant and a tooth, but there are times when it may be necessary and sometimes even desirable.5 Al-Omiri et al6 concluded that further long-term randomized clinical studies with large sample sizes are required to determine the viability of this treatment paradigm. In this author’s opinion, for this case, in the upper left posterior quadrant, combining 2 implant abutments with one natural tooth abutment was indicated.
CONCLUSION
Dentists and their teams have the power to change a person’s life, whether with appearance-related procedures, by restoring function, or with a combination of both. So long as a patient doesn’t have pain, swelling, or bleeding, I believe it’s important to talk with him or her about his or her goals for oral health and appearance, ie, his or her smile. Sometimes achieving the desired results is a smooth and short journey; other times, it’s long with unexpected challenges along the way. As the Beatles song title says, it can be a “long and winding road.” And when doing a full-mouth rehabilitation, we ought to keep the words of the dental icon Dr. Peter Dawson in mind. He said the longest distance between 2 points is a shortcut.7
This patient came in excitedly for a final visit that she called her “dental photo shoot.” She reported everything in her mouth felt fine and that she could smile and eat without hesitation. The final photo (Figure 19) shows how much the treatment meant to her. Much has been written about a smile. “Everyone smiles in the same language” has been attributed to the famous comedian, George Carlin. Mother Teresa said “Peace begins with a smile.” The Broadway hit musical Annie has a famous song titled “You’re Never Fully Dressed Without a Smile.”
At our final visit, I asked this patient to tell me what it meant to her to have her smile changed and give her what she once had. She told me, “All the work we put in to change my smile was life-changing. When I used to hide my smile for many, many years, I didn’t realize how debilitating that was. Today I smile with courage—I am encouraged. There’s nothing that stops me anymore because of my smile.” I concluded by asking her if her new smile was infectious. She replied, “That’s what I’m told.”
ACKNOWLEDGMENT
The author extends his heartfelt thanks to the late Stephen Killian, CDT; John Hunzicker; and the entire team at Spectrum Killian Dental Ceramics in Irvine, Calif.
REFERENCES
1. Fier MA. Patient-centered treatment planning: part 1. Dent Today. 2007;26:56-61.
2. Markley MR. Broken-stress principle and design in fixed bridge prosthesis. J Prosthet Dent. 1951;1(4):416-23. doi:10.1016/0022-3913(51)90027-3
3. Sivakumar S. Management of partial edentulism using nonrigid connectors as a treatment modality: a case report. Cureus. 2020;12(4):e7790. doi:10.7759/cureus.7790
4. Yaqoob A, Rasheed N, Ashraf J, et al. Nonrigid semi-precision connectors for FPD. Dent Med Res. 2014;2:17-21.
5. Spear F. Connecting teeth and implants: Yes, no, maybe? Spear Education. 2018.
6. Al-Omiri MK, Al-Masri M, Alhijawi MM, Lynch E. Combined implant and tooth support: an up-to-date comprehensive overview. Int J Dent. 2017;2017:6024565. doi:10.1155/2017/6024565
7. Hedlund A. How to avoid mistakes during treatment planning. Dawson Academy Whitepaper. 2014.
ABOUT THE AUTHOR
Dr. Fier is a practicing clinician and a clinical associate professor at the Touro College of Dental Medicine. He is the executive vice president of the American Society for Dental Aesthetics. He teaches continuing education courses nationally and internationally at dental schools, major conventions, and study clubs. Dr. Fier is a Diplomate of the American Board of Aesthetic Dentistry, a Fellow of the American College of Dentists, the International College of Dentists, and the Academy of Dentistry International. He can be reached at (845) 354-4300 or via email at docmarv@optonline.net or marvin.fier@touro.edu.
Disclosure: Dr. Fier receives lecture support from some of the companies mentioned in this article.












