INTRODUCTION
In the realm of contemporary dental practice, intricate cases often provide opportunities to demonstrate the integration of innovative technology and comprehensive clinical management. This case study presents a nuanced account of a patient who presented with a challenging dental scenario necessitating a multifaceted approach to restoration. The primary aim of this study is to illuminate the diagnostic process, treatment planning, and execution of a complex dental reconstruction supported by state-of-the-art techniques and equipment.
CASE REPORT
Patient Presentation
A female patient sought dental care at our clinic with a notable dental challenge. She presented with a previously placed 3-unit bridge on teeth Nos. 8 through 10 that had deteriorated to the point of being non-restorable (Figures 1 and 2). The cause of this bridge failure was attributed to a combination of a deep bite and occlusal trauma. Adding to the complexity, tooth No. 7 displayed mobility as a result of prior periodontal disease, rendering it unsuitable as a viable abutment for a new bridge (Figure 3).

Figure 1. Preoperative patient smile. Note the high smile-line and fractured teeth Nos. 8 and 10.

Figure 2. Pre-op image showing the deep bite contributing to fracture.

Figure 3. Pre-op x-ray showing minimal bone around No. 7 and a fractured root tip on No. 8.
Of note, the patient had been employing an Essix Appliance for more than a year and a half before discovering our practice. The Essix Appliance, a form-fitting, transparent shell, had been instrumental in maintaining tooth positions and aiding retention.
Despite recognizing the need for treatment, the patient hesitated to seek care due to her specific requirements. She was determined to find a dentist capable of comprehensively managing her case without the need for referrals to multiple specialists. Moreover, she was adamant about receiving care that incorporated the latest advancements in dental technology.
Remarkably, the patient sought our practice for more than just clinical expertise. She was drawn by our practice’s reputation for housing state-of-the-art technology and, importantly, a singular dentist capable of orchestrating every facet of her care. The patient’s insistence on avoiding multiple offices underscored the appeal of having a unified approach to her treatment, encompassing the roles of the restoring doctor, surgeon, and even lab technician, all under one roof.
Treatment Plan
Upon thorough examination, it became evident that attempting to restore the compromised bridge would yield a poor prognosis. As such, a decision was reached to extract teeth Nos. 7, 8, and 10 and to promptly replace them with implants at position Nos. 7 and 10. This intervention would involve employing partial extraction therapy and grafting techniques.
Utilizing a combination of preoperative CAD/CAM data and CBCT scans obtained through Orthophos SL 3D (Dentsply Sirona), a meticulous implant placement strategy was formulated with the aid of SICAT software (Figure 4). This software not only facilitated precise planning but also guided the creation of a surgical guide designed using the CEREC inLab system (Dentsply Sirona) and subsequently produced via a Primeprint 3D Printer (Dentsply Sirona).
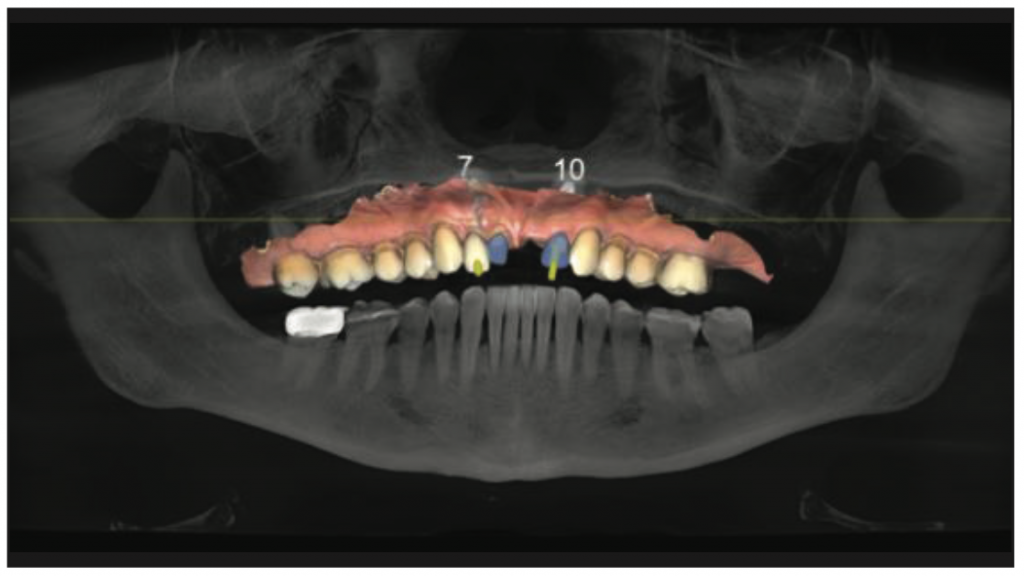
Figure 4. SICAT planning software with CAD/CAM imaging correlated.
Following the healing period, an intraoral scan would then be captured using Primescan technology (Dentsply Sirona) and employing intraoral FLO scan bodies. This digital scan would serve as the foundation for the design and fabrication of custom Atlantis abutments (Dentsply Sirona). Subsequently, a provisional bridge would be generated through 3D printing.
As the pontic sites matured, the final fixed bridge spanning teeth Nos. 7 to 10 would be crafted using the innovative KATANA Zirconia ONE material (Kuraray Noritake). The overarching treatment objective was twofold: to reinstate the patient’s missing teeth and, crucially, to rectify the deep bite surgically and restoratively. This comprehensive approach aimed to mitigate unfavorable occlusal forces on the new implant-supported bridge.
Treatment Execution and Clinical Outcomes
The foundation of our treatment approach rested on comprehensive records that provided us with invaluable insights. High-quality clinical photography, supplemented by intraoral x-ray images, allowed for a detailed assessment of the patient’s oral condition. However, the key to precision lies in the utilization of advanced imaging modalities. CBCT scans provided intricate 3D reconstructions, granting a deeper understanding of the patient’s bone structure and aiding in implant placement planning.
The integration of CAD/CAM technology was pivotal. Diagnostic wax-ups were meticulously crafted, facilitating visualization and communication of the intended treatment outcomes. This stage was particularly crucial for establishing the desired occlusal relationships and guiding the subsequent steps of the treatment plan. Precise calculations were conducted to determine the optimal bone reduction necessary to address the gummy smile and ameliorate the deep bite, ensuring a harmonious final result.
Dental Extractions and Immediate Implant Placement
With a comprehensive treatment plan in hand, dental extractions were performed, accompanied by partial extraction therapy to preserve the alveolar bone architecture. This meticulous approach was coupled with bone grafting to augment the sites for future implant placement. Immediate implant placement was executed at position Nos. 7 and 10, laying the groundwork for the eventual implant-supported bridge (Figures 5 and 6). To maintain the gains achieved during this phase, an Essix retainer was employed. This interim measure provided stabilization while minimizing the potential for undesirable tooth movement.
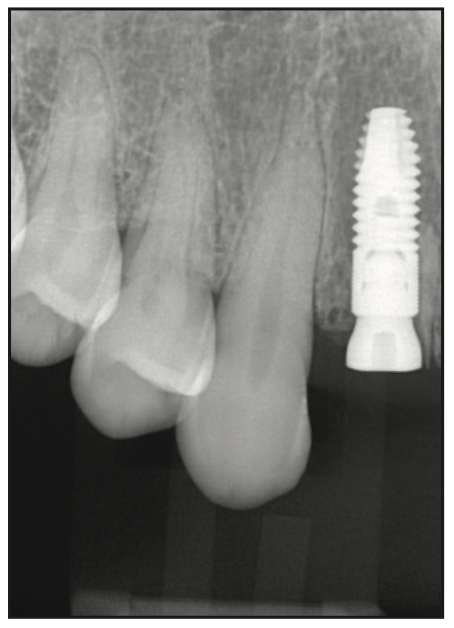
Figure 5. Implant placed on No. 7.
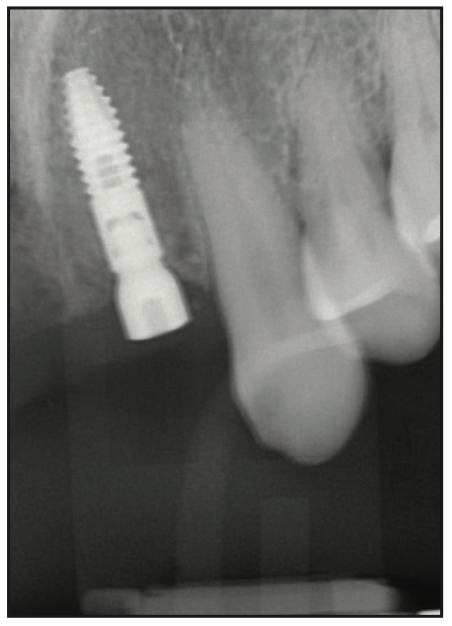
Figure 6. Implant placed on No. 10.
Uncovering and Healing Abutments
After the healing period, uncovering of the implants was undertaken. Healing abutments were positioned, enabling unimpeded tissue healing and facilitating the emergence profile.
Abutment Fabrication
Precision at every stage was our guiding principle. To this end, intraoral FLO scan bodies were integrated into the workflow, and digital scans were obtained for the design and fabrication of custom Atlantis abutments (Figure 7). These abutments, crafted from gold-hue titanium, were meticulously designed to ensure optimal fit and emergence profile, reinforcing the aesthetic and functional goals of the treatment (Figure 8).
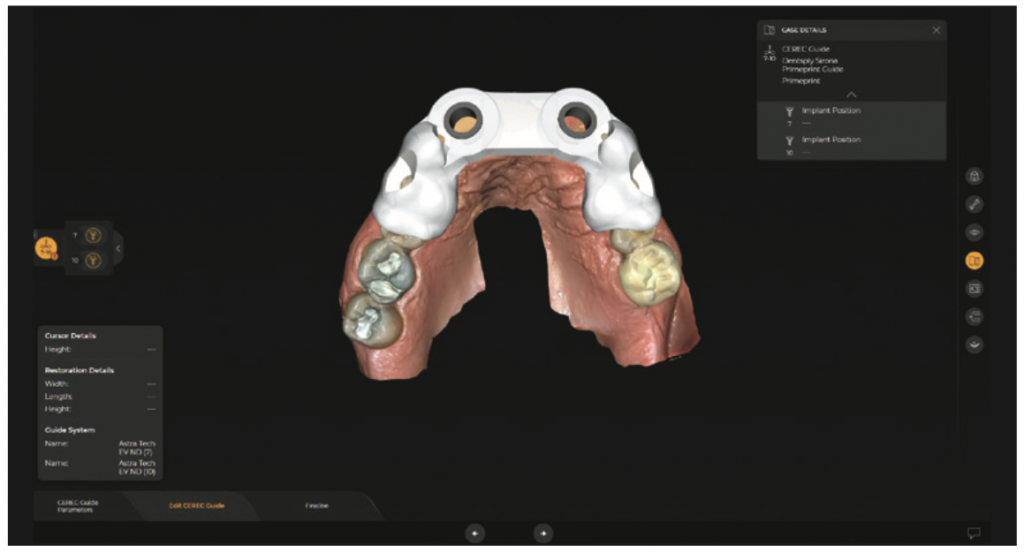
Figure 7. Surgical guides designed with inLab Software (Dentsply Sirona).
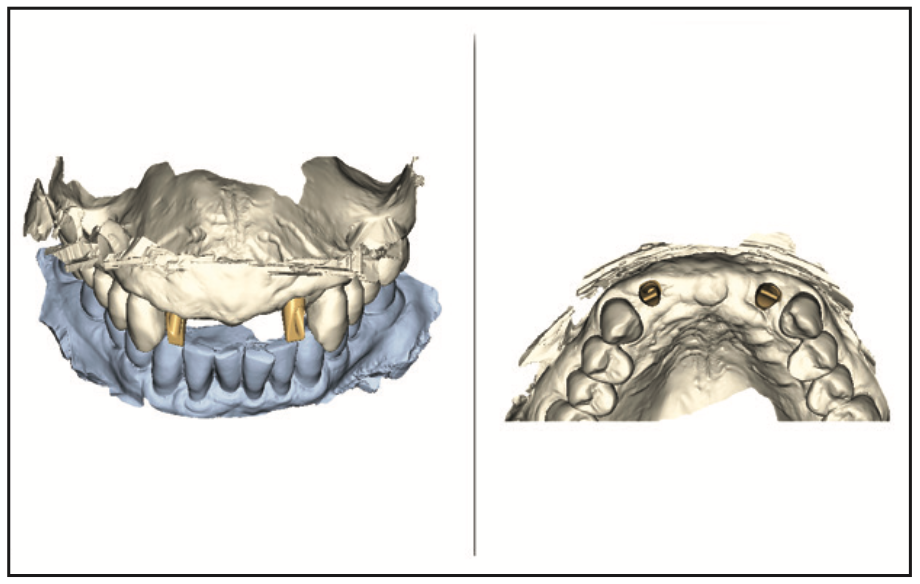
Figure 8. Custom abutments designed with Atlantis Editor (Dentsply Sirona).
Provisional Bridge Design and Fabrication
An integral stage of the treatment plan involved the design and fabrication of a provisional bridge to develop the pontic sites (Figures 9 and 10). Leveraging 3D printing technology through our Primeprint 3D printer, a provisional bridge was crafted. This intermediary step allowed for precise pontic development, ensuring optimal soft-tissue contours and enhancing the overall aesthetic outcome.

Figure 9. A temporary bridge for pontic development was 3D printed with Primeprint (Dentsply Sirona).

Figure 10. Pontic sites developed and ready for the final bridge.
Final Bridge Design and Fabrication
The penultimate stage heralded the transition to the fabrication of the final fixed bridge spanning teeth Nos. 7 to 10 (Figure 11). Iterative modifications to the design were meticulously carried out, culminating in a digital blueprint that captured the desired functional and aesthetic considerations. Milling, contouring, and glazing of the KATANA Zirconia ONE bridge were undertaken in-house, facilitated by the collaborative use of lab technologies. The final product seamlessly married form and function, delivering an exceptional final result (Figures 12 and 13).
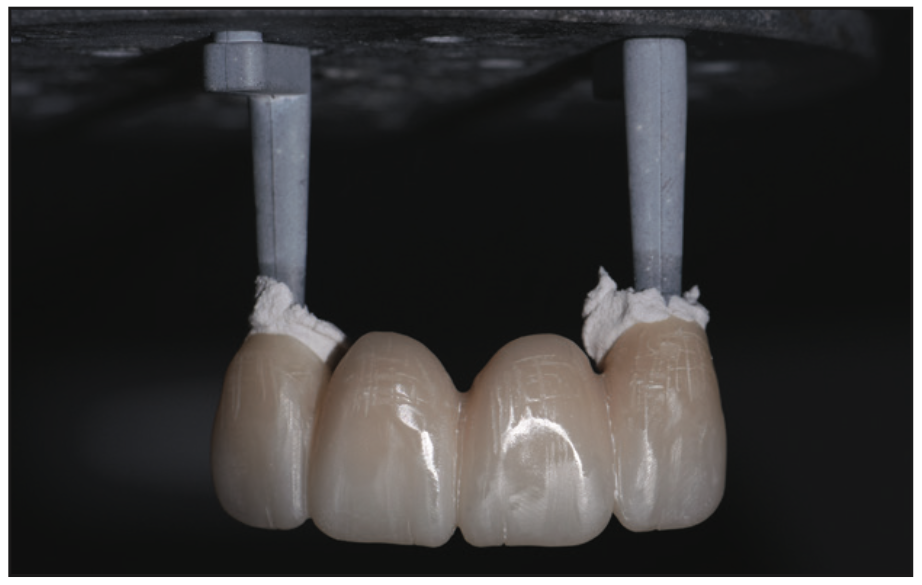
Figure 11. The 4-unit bridge (post-sinter) made with KATANA Zirconia ONE (Kuraray Noritake).

Figure 12. Final bridge.

Figure 13. Postoperative smile.
CONCLUSION
In conclusion, this intricate and multifaceted treatment journey underscores the power of technology-enabled dentistry. The judicious integration of advanced imaging, CAD/CAM systems, 3D printing, and collaborative lab technologies not only facilitated precision and efficiency but also contributed to patient confidence and acceptance.
The seamless orchestration of each step under a single practitioner’s guidance exemplified our commitment to holistic, patient-centered care, while the culmination of efforts in the form of a meticulously designed and crafted bridge bore testimony to the synergy between art and science in modern dental practice.
The patient’s satisfaction with the treatment was evident, reflecting the favorable outcomes and streamlined process of the intricate treatment plan. Her contentment resonated not only with the achieved results but also with the systematic and effective navigation through the comprehensive therapeutic regimen. This positive response underscored the synergy between advanced dental techniques and meticulous clinical management, exemplifying the convergence of patient-centric care and contemporary dentistry.
While the role of technology undoubtedly streamlined the delivery of this intricate treatment, the patient’s agreement with the proposed plan was heavily influenced by the perception of our practice’s technological capabilities. Beyond the treatment itself, effective communication of our practice’s technology-focused approach played a pivotal role in fostering patient trust and case acceptance.
Furthermore, the integration of technology into our workflow was contingent on its ease of use and compatibility with our established processes. This consideration extended to the meticulous selection of equipment, ensuring that each component seamlessly contributed to a patient-centered and efficient treatment journey.
ABOUT THE AUTHOR
Dr. Apekian graduated from the University of California (UC), Davis, with a degree in neurobiology, physiology, and behavior. She earned her DDS degree from UC, San Francisco (UCSF), where she graduated top of her class. She is active in the Sacramento District Dental Society, serving as the legislative committee chair, as well as serving on the Continuing Education, Ethics, and Leadership Committees. She has also represented Sacramento at the California Dental Association (CDA) House of Delegates. Dr. Apekian is an active member of the CDA, ADA, and UCSF Alumni Association. She recently built and designed one of the most technologically advanced dental offices, utilizing CAD/CAM technologies, 3D imaging, state-of-the-art infection control systems, and full digital integration. She is a graduate of the Sacramento Implant Continuum and utilizes the latest technology for guided implantology. She also serves as a mentor and trainer for Dentsply Sirona’s CEREC CAD/CAM technology throughout the Sacramento, Calif region. She teaches fellow dentists how to utilize the technology to design and produce complete restorations, surgical guides, and appliances for prosthetics, implantology and orthodontics. She can be reached at gotfloss@gmail.com.
Disclosure: Dr. Apekian has financial interests in Kuraray Noritake and Dentsply Sirona.












