INTRODUCTION
Sjögren’s Syndrome (SS) is a systemic autoimmune disease affecting the exocrine glands. It is characterized by intense lymphocytic infiltration that progressively destroys mainly salivary and lacrimal glands.1,2 SS is subdivided into 2 categories: primary, which includes dry eyes and hyposalivation, and secondary, which occurs in conjunction with other connective-tissue diseases (eg, arthritis and lupus erythematosus, among others).3 The etiology is unknown. It is suggested that an interaction between environmental factors (eg, viruses, stress, hormones) and patient genetics can lead to inflammatory responses against epithelial tissues.4,5
SS is the second most common connective tissue disease, affecting up to 3.1 million Americans, or approximately 1 in 70 people, according to the National Arthritis Data Workgroup. This number refers to those presenting with primary SS. It can be doubled if including patients presenting with secondary SS.6,7 It is more commonly found in women than in men (9:1) and is most often diagnosed during the fourth and fifth decades of life.5,8
Oral symptoms include dry mouth; cracked lips; angular cheilitis; mucosal sores; tongue depapillation; swelling of the salivary glands; oral infections, such as candidiasis; and difficulty in mastication, swallowing, and speech. Hyposalivation and changes in saliva composition can cause a burning sensation and an intolerance to the use of removable prostheses.9 Moreover, patients with xerostomia have a high incidence of caries, resulting in the extraction of teeth during their lifetimes.10 This oral agony impacts patients psychologically and emotionally, affecting their social interactions and quality of life.11
Early interdisciplinary intervention is recommended to provide long-term solutions for improving function, speech, aesthetics, and self-esteem.
Oral rehabilitation with implants is a possible solution since SS does not affect bone healing and osseointegration.2,5,12 Binon and Fowler13 presented a case report with mandibular-osseointegrated implants and a fixed prosthesis that remained functional and stable after 13 years of followup. Due to the difficulties SS patients have wearing removable prostheses, a fixed transitional prosthesis during the surgical stage is key. Drew et al14 proposed the stage approach, in which hopeless teeth are kept in strategic positions as abutments to support an interim fixed prosthesis during the surgical stage, making the transition from a terminal dentition to a full-arch reconstruction easier. Some of the advantages of this technique include increased patient comfort, soft-tissue management, protection of grafted areas, alveolar bone preservation, and surgical templates for the position of future implants.
Furthermore, the severity of caries makes the extraction of teeth a very common procedure affecting the alveolar ridge morphology. In general, the buccal vertical bone resorbed 2.2 mm after extraction, making the ridge augmentation procedure required before implant placement in most cases. Another option to avoid extraction in strategic sites is root preservation. Its requirements include prophylactic root canal therapy and removal of coronal tooth structure, leaving the root face below the crestal bone. This technique preserves the ridge form on pontic sites between teeth or implants, supports the soft tissue, and prevents epithelial down growth.15 The aim of the present case series is to show a simple way to restore these complex cases. Case 1 shows the sequence from a terminal dentition to full-mouth, implant-supported prostheses using the stage approach and the root banking technique. Case 2 shows the longevity of an SS patient after 15 years of followups using the staged approach.
CASE REPORTS
Case 1
A 59-year-old Caucasian female presented to the department of periodontics, Rutgers School of Dental Medicine, with the chief complaint of “All my teeth are breaking.” She was diagnosed with SS and rheumatoid arthritis in 2015. The patient was dissatisfied with her smile and came to the school to find a permanent solution. Intraoral examination revealed a partially edentulous maxilla and mandible, dry mouth, and subgingival carious lesions in the majority of her teeth with a decrease in the occlusal vertical dimension (OVD) (Figure 1). Radiographic examination revealed sinus pneumatization, recurrent and subgingival caries, and defective endodontic lesions (Figures 2 and 3). On the first visit, oral health was addressed by prescribing a high-fluoride toothpaste (PreviDent 5000 [Colgate Oral Pharmaceuticals]) to be used 3 times per day. A comprehensive evaluation of her case with a multidisciplinary team, including the prosthodontics and periodontics departments, determined that a full-mouth implant rehabilitation would be the best option for her. The patient was motivated and agreed to proceed with the treatment.

Figure 1a.

Figure 1b.

Figure 1c.

Figure 1d — Figure 1. (a to c) Initial clinical view. The patient presented with severe subgingival caries and remaining roots and missing several teeth. (d) Asymmetry in her smile that does not follow the lower lip, and several missing teeth in the posterior areas.
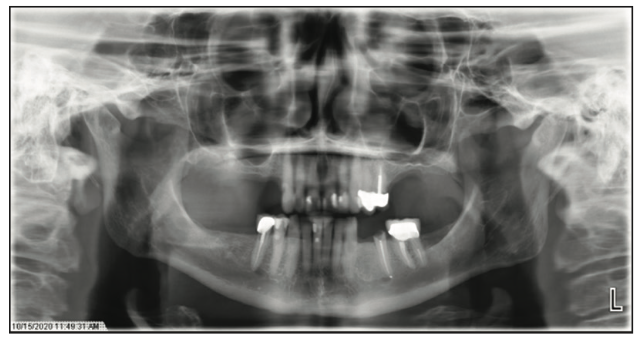
Figure 2. Initial panoramic radiograph showing the terminal dentition and bilateral pneumatization of the maxillary sinuses.
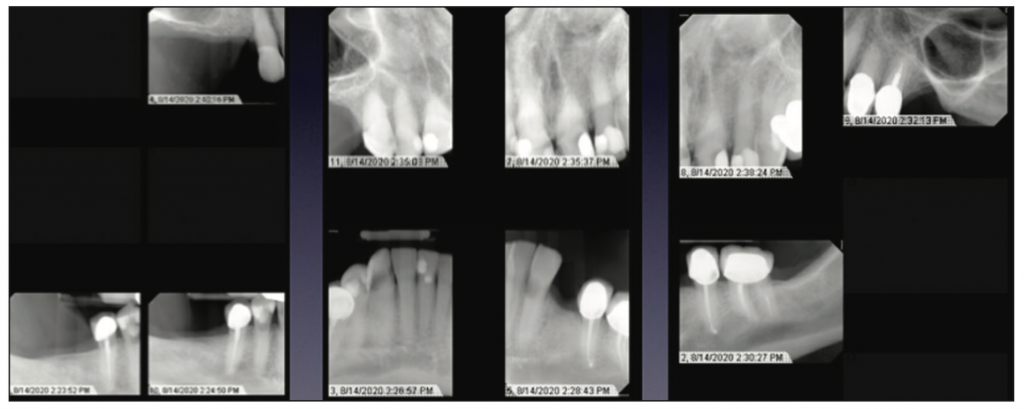
Figure 3. Initial periapical radiographs with recurrent and subgingival caries, missing teeth, and defective endodontic lesions.
Treatment was planned to have multiple phases. The first phase involved the abutment selection to hold the interim fixed prostheses. In the maxilla, the upper right canine, central incisors, and first upper left premolar were selected, and in the mandible, the lateral incisors, lower left first molar, and lower right second premolar were selected. These teeth presented a strategic position in the arches without periodontal involvement or mobility. Preliminary casts were articulated in centric relation, and diagnostic waxing was made with OVD increased, improving aesthetics and function.
The teeth were prepared, and hopeless teeth were decoronated (their pulp chambers were calcified). Subgingival carious lesions were excavated and restored with glass ionomer material. Then polymethyl methacrylate (PMMA) shells with metal reinforcements were relined with PMMA (ALIKE [GC America]) (Figures 4 to 6).
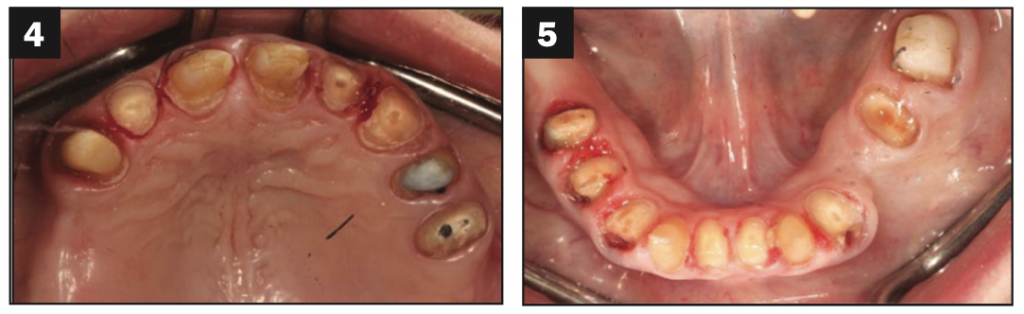
Figures 4 and 5. Temporary abutments were prepared.

Figure 6. Maxillary and mandibular interim full-arch prostheses inserted after teeth were prepared and hopeless teeth were decoronated.
The second step involved the surgical phase. Decoronated teeth were extracted and grafted with allograft (RegenerOss [ZimVie]) and resorbable membrane (Geistlich Bio-Gide [Geistlich Pharma AG]) to maintain the bony architecture for future implant placement (Figure 7). Four months later, CBCT was taken with guide stents. Implant planning was made with Romexis planning software (Planmeca Group), and tooth-borne surgical guides were fabricated (Figure 8). Five implants (ZimVie) were placed in each arch: In the maxilla, 4/3- × 10-mm upper right first premolar, 3.25- × 13-mm and 3.25- × 11.5-mm lateral incisors, 3.25- × 11.5-mm upper left canine, and 5/4- × 10-mm second premolar; and in the mandible, 4/3- × 8.5-mm implants in the lower left second premolar and canine, 3.25- × 10-mm between central incisors, and 4/3- × 10-mm in the lower right first premolar and first molar sites (Figures 9 and 10). After surgery, interim fixed prostheses were adjusted, and pressure was released against the tissues. Implant sites were uncovered after 4 months. Then digital scans were made (TRIOS [3Shape]) with scan bodies (BellaTek Encode Impression System [ZimVie]) (Figures 11 and 12). Scans were imported into a CAD/CAM software program (3Shape Dental System [3Shape]) to fabricate a new set of interim prostheses.

Figure 7. Hopeless teeth were extracted and grafted.
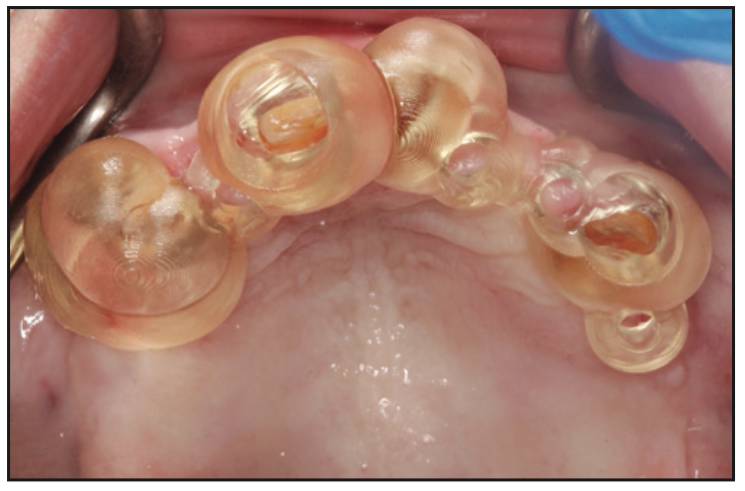
Figure 8. Implant placement with a tooth-borne supported surgical guide.
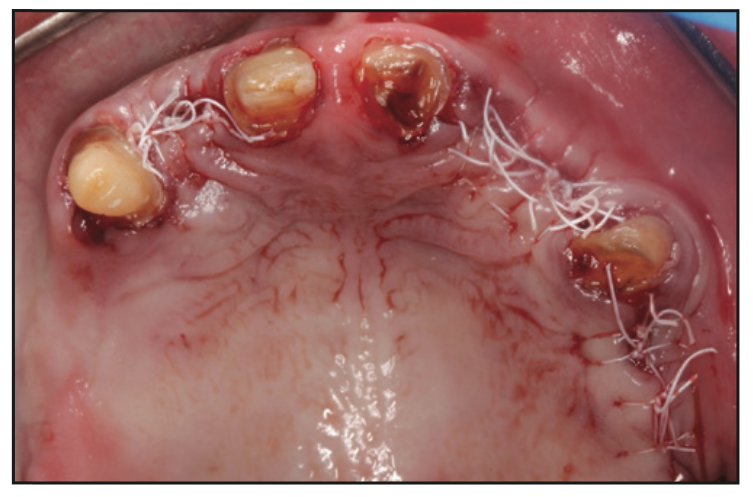
Figure 9. Five implants were placed and grafted.

Figure 10. Lower anterior area, implant placement with simultaneous soft-tissue grafting with Fibro-Gide (Geistlich USA) to change the soft-tissue phenotype.
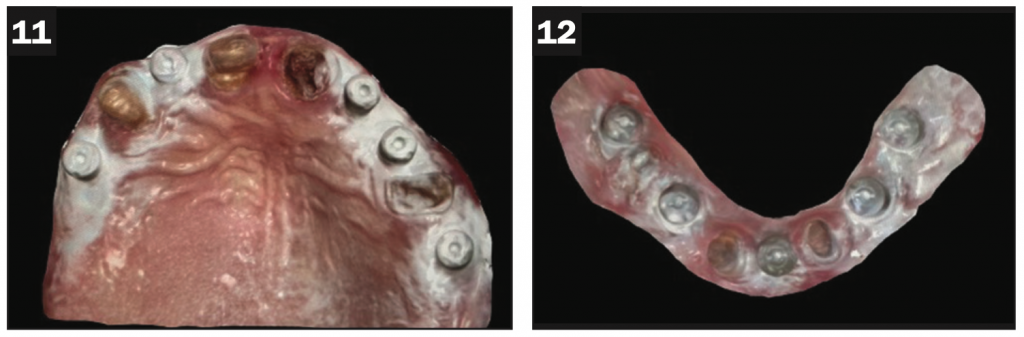
Figures 11 and 12. Scan bodies inserted to fabricate a new set of interim prostheses (implant-supported).
The third phase involved prophylactic root canal therapy in the upper right canine, central incisor, and lower lateral incisors. Root canal therapies were performed, the coronal gutta-percha was removed, and tapered preparation of the coronal canal space was made to facilitate the Geristore (DenMat) placement 2 mm below the crestal bone. A minimum of 5 mm of gutta-percha was maintained in the apical portion of the canal space to ensure an adequate apical seal. Geristore was placed in the tapered wall preparation with a small tip engaged at the level of the gutta-percha (Figure 13). The remaining teeth were decoronated, and full-arch, screw-retained prostheses were inserted, making the transition from tooth-borne interim prostheses to implant-supported interim prostheses. The upper left central incisor, second premolar, lower left first molar, and lower right second premolar were extracted and grafted with allograft (RegenerOss [ZimVie]).
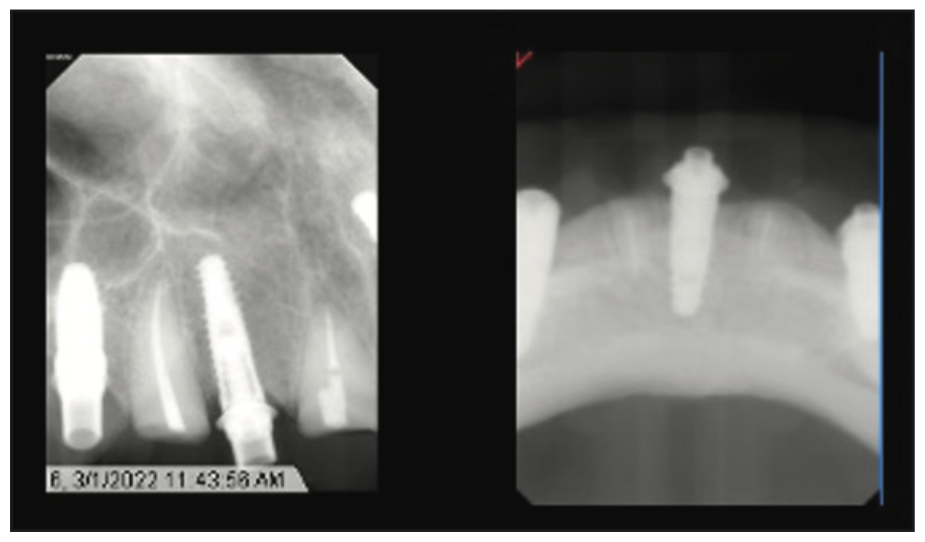
Figure 13. Prophylactic root canals were performed, gutta-perchas were removed, and tapered root spaces were filled with Geristore (DenMat).

Figure 14. Smile after delivering definitive prostheses.
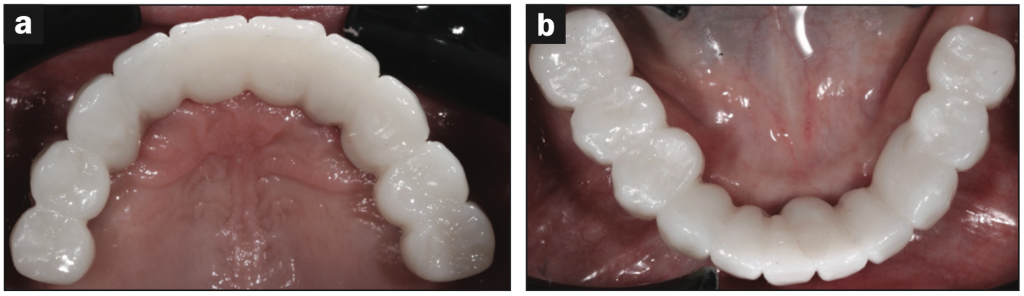
Figure 15. (a) Maxilla: occlusal view after cementation. (b) Mandible: occlusal view after insertion.
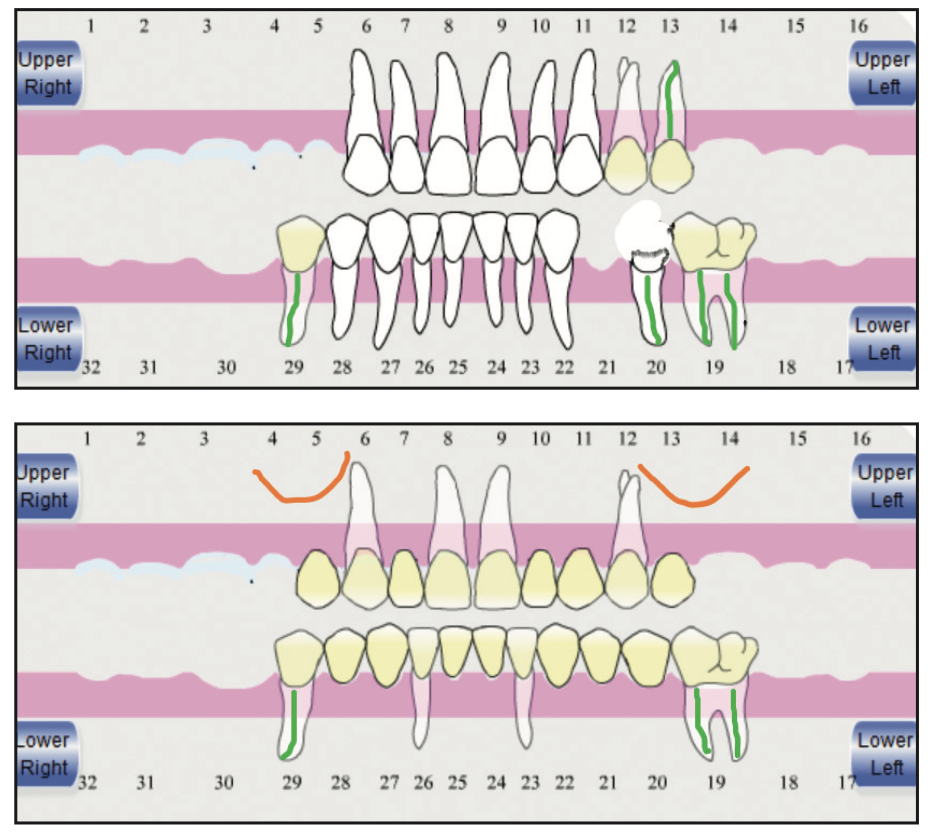
Figure 16. Schematic sequence, upper view: initial presentation. Lower view: selection of the strategic abutments to hold the interim prostheses.
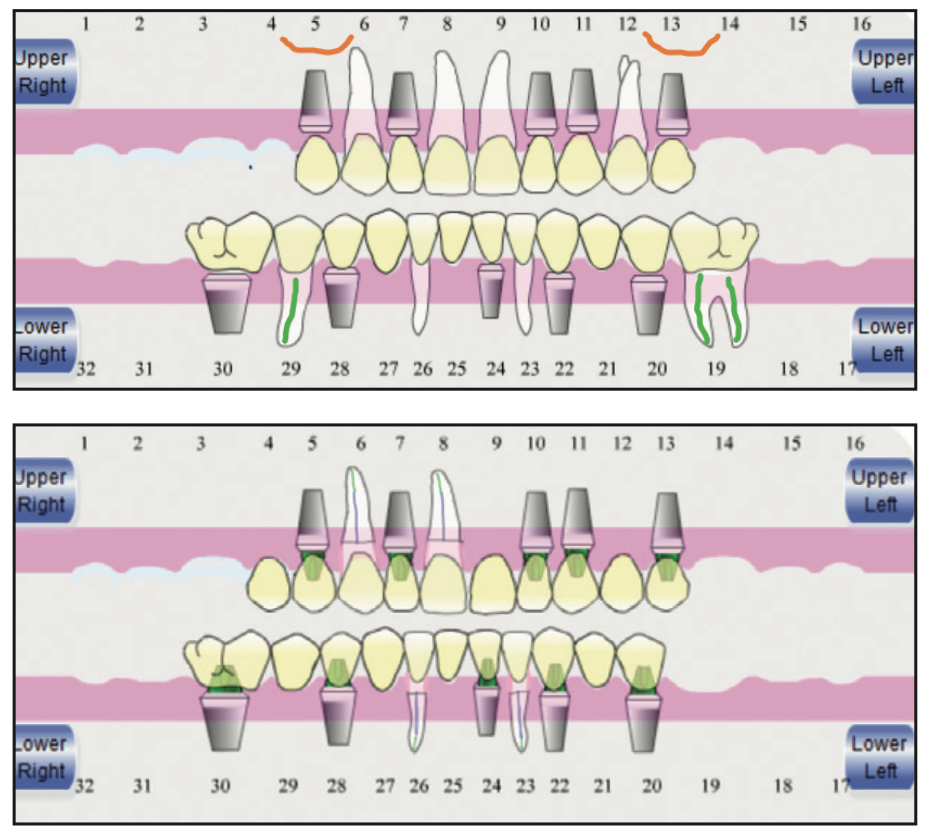
Figure 17. Upper view: Five implants were inserted in the maxilla and in the mandible. Internal sinus elevations were made with immediate implant placement in the premolar sites. Lower view: definitive full-arch, fixed prostheses. Root banking was made to preserve the buccal anatomy and maintain the bone for possible future implants.
The fourth step involved the restorative phase, in which maxillary and mandibular master casts were generated and verified. Gold-shaded titanium custom abutments (Atlantis [Dentsply Sirona]) were inserted in the maxilla, and multi-unit abutments were placed in the mandible. PMMA prototypes were inserted and adjusted. The patient stayed with the prototypes for 2 weeks to evaluate oral hygiene, phonetics, aesthetics, and function. All the corrections were made to them. After 2 weeks, prototypes were re-scanned in the laboratory. Definitive monolithic zirconia prostheses were delivered (Figures 14 and 15). An occlusal device was inserted with 4 months of recall appointments. A treatment plan sequence was summarized in the schematic view using Dental_Flash (Attachments International) (Figures 16 and 17).
Case 2
A 62-year-old white female presented to the periodontics department in August 2006. Her chief complaint was that she was “tired of fillings and root canal treatments.” Previous dental treatment included several extractions, root canals, implants, and a removable partial prosthesis that she did not tolerate. She stated she had been through several reconstructions that had failed due to caries on abutment teeth. She was diagnosed with SS and Lichen Planus many years ago. Intraoral examination revealed generalized gingival inflammation with bleeding on probing, crowns and bridges in the maxilla, subgingival caries, and defective restorations in the mandible (Figure 18). Radiographic examination revealed defective restorative materials, RCTs, carious lesions, and implants on the molars and premolar areas (Figures 19 and 20). After evaluation of all her factors and patient expectations, the option of implant-supported, fixed prostheses was offered to the patient. The stage approach was crucial in her case because she had poor tolerance of a removable prosthesis in the past. A schematic sequence using Dental_Flash briefly summarized her phases using the staging approach (Figures 21 and 22). The patient has been stable for the past fifteen years with 4-month recall appointments (Figure 23).

Figure 18a.

Figure 18b.

Figure 18c — Figure 18. (a to c) Initial presentation.
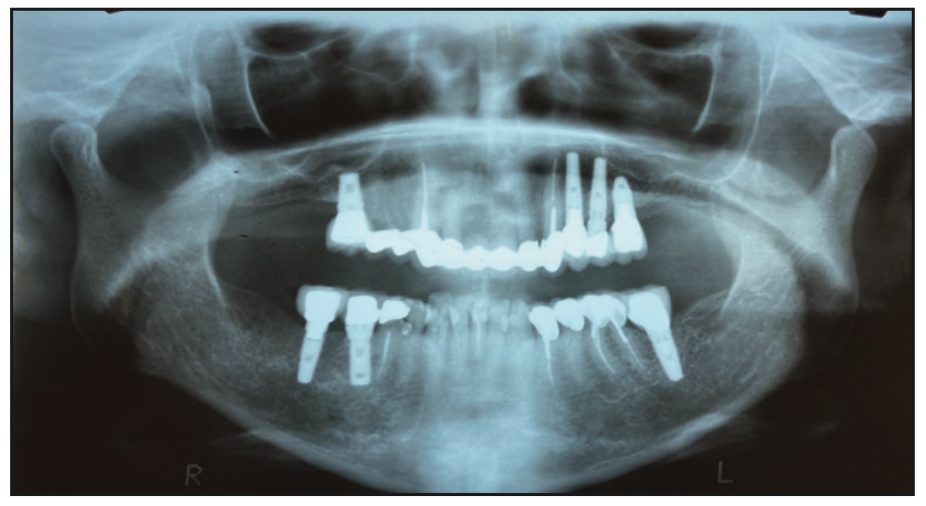
Figure 19. Initial panoramic radiograph.
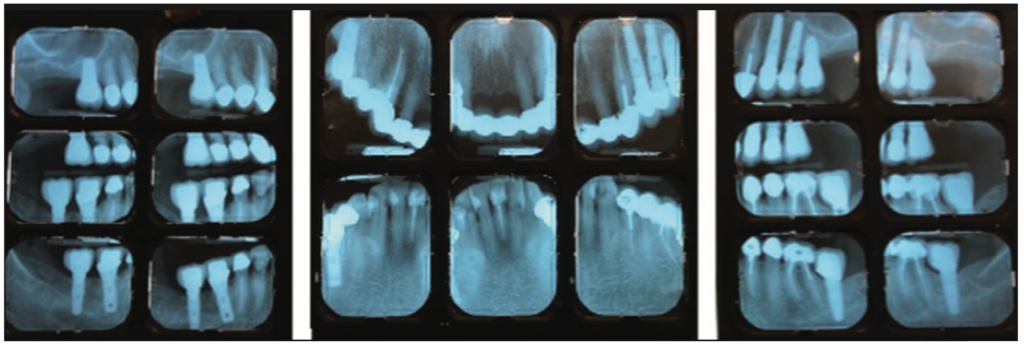
Figure 20. Initial periapical radiograph.
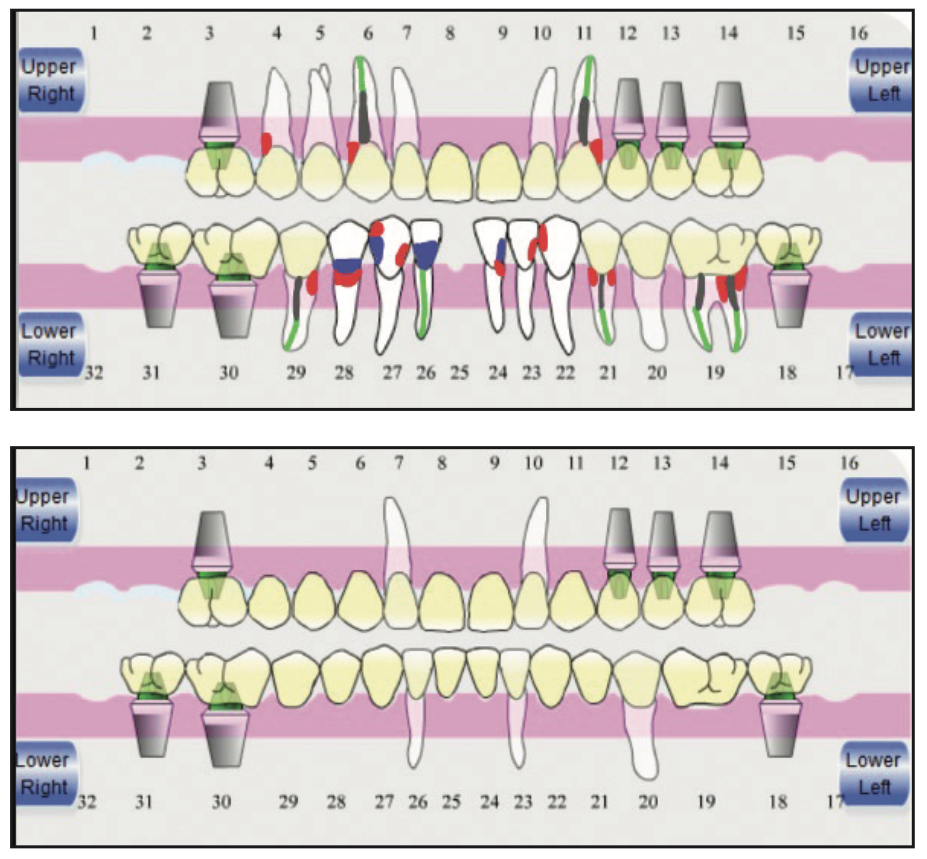
Figure 21. Upper view: initial presentation of the patient with several RCTs, subgingival caries, and defective restorations. Lower view: selection of the key abutments. Five natural abutments were preserved and connected with the poste- rior implants to stage the case. Hopeless teeth were extracted, and insertion of the fixed interim prostheses that were used during the entire treatment was done.
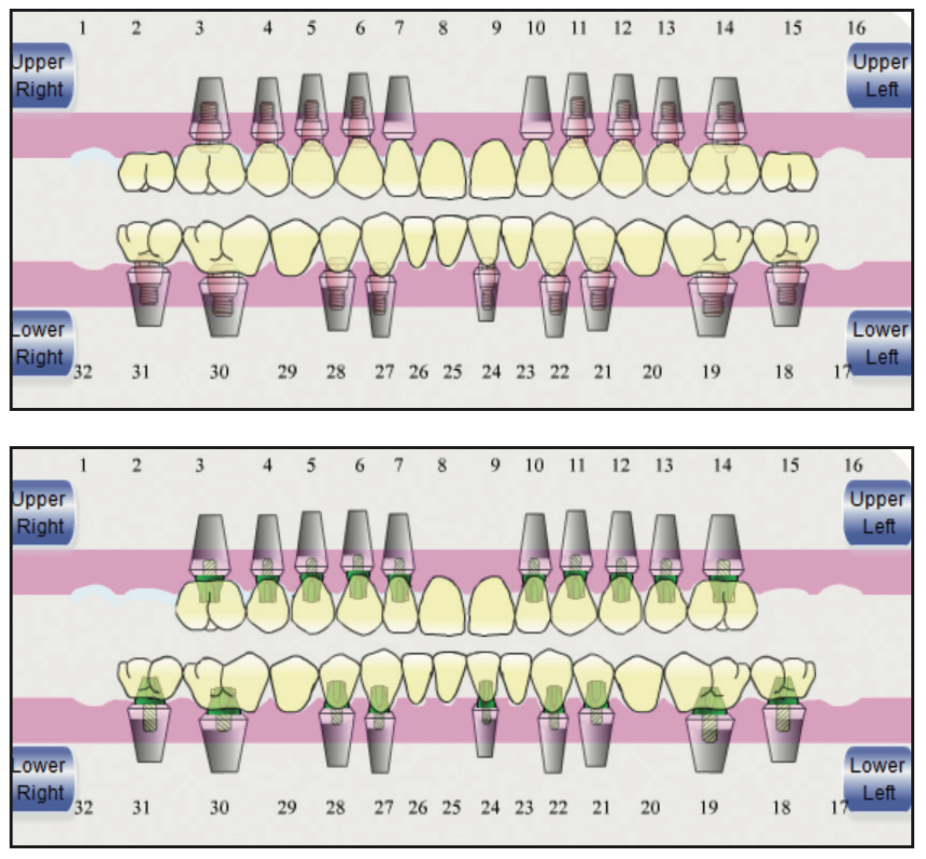
Figure 22. Upper view: Implants were placed as shown in the schematic. Four months after healing, abutment teeth were extracted with immediate implant placement of the lateral incisors. Lower view: The following final prostheses were planned: In the maxilla, posterior segments from first premolar to first molar; In the mandible, posterior segments from first premolar to second molar; and both anterior segments from canine to canine.
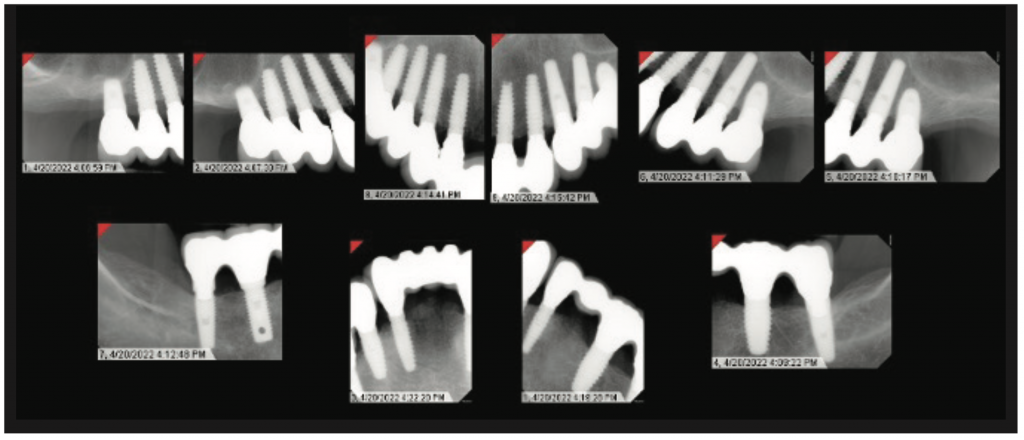
Figure 23. Fifteen-year followup: periapical radiograph of implants showing no bone loss after all those years of function.
DISCUSSION
SS patients show a high incidence of dental caries despite a recall frequency of 5 visits per year.16 One study found that SS patients with excellent oral hygiene, on 3- to 4-month recalls and fluoride dentifrices, had elevated levels of dental caries with premature tooth loss.7 This problem is a consequence of the decrease in salivary flow and changes in its composition.5 It also contributes to difficulties wearing removable prostheses because, in the absence of saliva, the protective layer is not present, making the mucosa susceptible to sores. Additionally, in a complete denture, low salivary volume can affect the retention of the prosthesis.9 Therefore, a different approach needs to be implemented with these patients.
The staged approach was followed to maintain a fixed interim prosthesis during the entire rehabilitation process. In 2010, Cordaro et al17 described a protocol to stage a patient. This protocol offers many benefits, such as avoiding removable prostheses, improving patient comfort, and soft-tissue management, among others.14 This technique can be performed with natural teeth or with transitional implants if natural teeth are absent.18 However, it can be more time-consuming to treatment plan, but lengthy treatment can be helpful for a patient’s financial planning.14,17,18
Furthermore, root banking was performed to preserve the shape of the alveolar bone, gingival tissue, and alveolar mucosa. It can be done with a coronally advanced flap or an autogenous soft-tissue graft to cover over the root surfaces, allowing new cementum and connective tissue to form above the coronal surface.19 Over time, there is a flattening of the crest, and the periosteum grows on top of the maintained roots. The periosteum is attached to the supracrestal interdental fibers, and bone grows crestal to the root.20 The rationale for preserving the root is to create potential future implant sites. To perform this technique, prophylactic root canal therapy with a final canal orifice restoration is needed. In 1997, the application of resin-ionomer restorative materials for the repair of external resorption defects in the cervical one-third of roots was presented. It showed high-power micrographs illustrating the close adhesion of fibroblasts and connective tissue to this dual-cure, self-adhesive resin-glass ionomer restoration.21 Placement of this material into the root canal space has been studied in the endodontic literature because of its ease of placement, fast setting time, and retro canal leakage qualities.22 In 2005, utilizing scanning electron microscopy, it was indicated that human gingival fibroblasts proliferate, attach, and spread when in contact with Geristore and maintain relatively normal morphology.23
Coronal tooth structure must be maintained during the time in which root canal therapy is performed. At this stage, placement of Geristore coronal seal maintains proper restoration at the occlusal cavosurface margin seal before tooth decoronation. It is critical that the placement depth of the Geristore restoration must extend below the anticipated horizontal root sectioning on the root face. Apical gutta-percha must maintain a minimum of 5 mm apical seal length for predictable root canal therapy success.
From the prosthodontics perspective, performing an aesthetic analysis before any intervention is paramount. In 2011, Bidra24 described all the parameters that must be evaluated when a fixed, implant-supported prosthesis is in mind. Lip position and gingival display are critical and must be evaluated during static and dynamic movement when the patient smiles.25 After this analysis, the possibility of adding pink ceramic to the final prosthesis was taken under consideration since after extractions and implant placement, some bone loss can cause a gingival recession that can be visible because of the amount of display of gingiva during a maximum smile. Therefore, using pink ceramic can allow adequate contours to be obtained, compensating for gingival recession and promoting aesthetics.26 When pink ceramic is expected, the prosthesis-tissue junction must be evaluated. As a rule, the crestal bone level must be apical to the maxillary lip-line at the time of maximum smile. If these parameters are not met during the preoperative evaluation, an aggressive presurgical procedure must be performed before implant placement.25
In addition, during the smile analysis, the necessity to restore the patient up to the first molar was evaluated. In case 1, during maximum smile, the patient showed up to the second premolars. Restoring the patient to the molar areas would have required external sinus lifts; therefore, it was decided to go with a shortened dental arch (SDA).27 In a 6-year follow-up study of oral function in SDAs, the authors concluded that SDAs provide durable occlusal stability.28 Likewise, Hattori et al29 indicated that during maximum voluntary clenching, SDAs never caused overloading in the TMJ, and Witter30 concluded that masticatory ability is generally sufficient when 20 or more teeth remain. Thus, the SDA protocol can be the most conservative treatment for high-risk patients without compromising oral functionality.27
In case 2, it can be appreciated how beneficial serial extractions can be for dentists and patients. Implementing this approach, the 2-stage implant placement procedure is simple to follow. In this case, natural teeth and implants were used as strategic abutments. Because other dentists placed those implants, the case was overengineered. Early reports suggested using as many implants as possible in the maxilla, from 6 to 10, and having 4 to 8 implants in the mandible being parallel to each other to support the full-arch prostheses.31 Recent studies suggest that the use of 6 or more implants in the maxilla and 4 to 6 implants in the mandible results in a high survival rate above 95%.32,33 Moreover, using the root banking technique allows us to use fewer implants, submerging roots in the pontic areas to preserve the alveolar bone for the future. Today, this case would be planned differently: 7 implants in the maxilla using the 4 implants in the posterior areas that the patient presented and adding implants for the upper right first premolar, central incisor, and upper left lateral, root banking both canines. In the mandible, recommended therapy would be to restore the case with 6 implants, including the 3 implants that patient presented with in the posterior areas and 3 additional fixtures in the bilateral cuspid areas and left second premolar area. We could also root bank bilateral first premolars and the left central incisor. In the 15-year sequential radiographs, it can be appreciated that the crestal bone around the implants remained stable, implant probing depths were 3 mm or less, and the tissues showed little change after 15 years of function. This patient maintains above average home hygiene with reinforced hygiene appointments every 4 months.
CONCLUSION
SS patients are immunocompromised with many negative impacts on their mouths, affecting their function, aesthetics, and social interactions. Thus, a multidisciplinary team is crucial to treat them. This clinical report shows how, with the use of selective terminal abutment teeth, a patient can be restored from a terminal dentition to a full-mouth, fixed rehabilitation. Since many SS patients have a history of dental failures, root banking can be a consideration to preserve the bone in the pontic sites for future implants. Fifteen years of followup indicates that the staging approach may be beneficial for the SS patient.
REFERENCES
1. de Mendonça Invernici M, Finger Stadler A, Nicolau G, et al. Management of Sjogren’s syndrome patient: a case report of prosthetic rehabilitation with 6-year follow-up. Case Rep Dent. 2014;2014:761251. doi:10.1155/2014/761251
2. Chrcanovic BR, Kisch J, Wennerberg A. Dental implants in patients with Sjögren’s syndrome: a case series and a systematic review. Int J Oral Maxillofac Surg. 2019;48(9):1250–9. doi:10.1016/j.ijom.2019.02.005
3. Jorkjend L, Johansson A, Johansson AK, et al. Periodontitis, caries and salivary factors in Sjögren’s syndrome patients compared to sex- and age-matched controls. J Oral Rehabil. 2003;30(4):369–78. doi:10.1046/j.1365-2842.2003.01088.x
4. Mavragani CP, Moutsopoulos HM. Sjögren’s syndrome. Annu Rev Pathol. 2014;9:273–85. doi:10.1146/annurev-pathol-012513-104728
5. González S, Sung H, Sepúlveda D, et al. Oral manifestations and their treatment in Sjögren’s syndrome. Oral Dis. 2014;20(2):153–61. doi:10.1111/odi.12105
6. Zero DT, Brennan MT, Daniels TE, et al; Sjögren’s Syndrome Foundation Clinical Practice Guidelines Committee. Clinical practice guidelines for oral management of Sjögren disease: Dental caries prevention. J Am Dent Assoc. 2016;147(4):295-305. doi:10.1016/j.adaj.2015.11.008
7. Cartee DL, Maker S, Dalonges D, et al. Sjögren’s syndrome: Oral manifestations and treatment, a dental perspective. J Dent Hyg. 2015;89(6):365–71.
8. Mathews SA, Kurien BT, Scofield RH. Oral manifestations of Sjögren’s syndrome. J Dent Res. 2008;87(4):308–18. doi:10.1177/154405910808700411
9. Bolstad AI, Skarstein K. Epidemiology of Sjögren’s syndrome—from an oral perspective. Curr Oral Health Rep. 2016;3(4):328–36. doi:10.1007/s40496-016-0112-0
10. Christensen LB, Petersen PE, Thorn JJ, et al. Dental caries and dental health behavior of patients with primary Sjögren syndrome. Acta Odontol Scand. 2001;59(3):116–20. doi:10.1080/000163501750266684
11. Enger TB, Palm Ø, Garen T, et al. Oral distress in primary Sjögren’s syndrome: implications for health-related quality of life. Eur J Oral Sci. 2011;119(6):474–80. doi:10.1111/j.1600-0722.2011.00891.x
12. Payne AG, Lownie JF, Van Der Linden WJ. Implant-supported prostheses in patients with Sjögren’s syndrome: a clinical report on three patients. Int J Oral Maxillofac Implants. 1997;12(5):679-85.
13. Binon PP, Fowler CN. Implant-supported fixed prosthesis treatment of a patient with Sjögren’s syndrome: a clinical report. Int J Oral Maxillofac Implants. 1993;8(1):54–8.
14. Drew HJ, Alnassar T, Gluck K, et al. Considerations for a staged approach in implant dentistry. Quintessence Int. 2012;43(1):29-36.
15. Choi S, Yeo IS, Kim SH, et al. A root submergence technique for pontic site development in fixed dental prostheses in the maxillary anterior esthetic zone. J Periodontal Implant Sci. 2015;45(4):152–5. doi:10.5051/jpis.2015.45.4.152
16. Chuang CJ, Hsu CW, Lu MC, et al. Increased risk of developing dental diseases in patients with primary Sjögren’s syndrome—A secondary cohort analysis of population-based claims data. PLoS One. 2020;15(9):e0239442. doi:10.1371/journal.pone.0239442
17. Cordaro L, Torsello F, Ribeiro CA. Transition from a failing dentition to a removable implant-supported prosthesis: a staged approach. Quintessence Int. 2010;41(5):371–8.
18. Papaspyridakos P. Full mouth implant rehabilitation with staged approach: 6-year clinical follow-up. J Esthet Restor Dent. 2015;27(4):213–23. doi:10.1111/jerd.12158
19. Salama M, Ishikawa T, Salama H, et al. Advantages of the root submergence technique for pontic site development in esthetic implant therapy. Int J Periodontics Restorative Dent. 2007;27(6):521–7.
20. O’Neal RB, Gound T, Levin MP, et al. Submergence of roots for alveolar bone preservation. I. Endodontically treated roots. Oral Surg Oral Med Oral Pathol. 1978;45(5):803–10. doi:10.1016/0030-4220(78)90158-5
21. Dragoo MR. Resin-ionomer and hybrid-ionomer cements: part II, human clinical and histologic wound healing responses in specific periodontal lesions. Int J Periodontics Restorative Dent. 1997;17(1):75–87.
22. Greer BD, West LA, Liewehr FR, et al. Sealing ability of Dyract, Geristore, IRM, and super-EBA as root-end filling materials. J Endod. 2001;27(7):441–3. doi:10.1097/00004770-200107000-00001
23. Al-Sabek F, Shostad S, Kirkwood KL. Preferential attachment of human gingival fibroblasts to the resin ionomer Geristore. J Endod. 2005;31(3):205–8. doi:10.1097/01.don.0000137650.61607.25
24. Bidra AS. Three-dimensional esthetic analysis in treatment planning for implant-supported fixed prosthesis in the edentulous maxilla: review of the esthetics literature. J Esthet Restor Dent. 2011;23(4):219–36. doi:10.1111/j.1708-8240.2011.00428.x
25. Bidra AS, Agar JR. A classification system of patients for esthetic fixed implant-supported prostheses in the edentulous maxilla. Compend Contin Educ Dent. 2010;31(5):366–8, 370, 372–4 passim.
26. Simon H, Raigrodski AJ. Gingival-colored ceramics for enhanced esthetics. Quintessence Dent Technol. 2002;25:155–72.
27. Armellini D, von Fraunhofer JA. The shortened dental arch: a review of the literature. J Prosthet Dent. 2004;92(6):531–5. doi:10.1016/j.prosdent.2004.08.013
28. Witter DJ, de Haan AF, Käyser AF, et al. A 6-year follow-up study of oral function in shortened dental arches. Part I: Occlusal stability. J Oral Rehabil. 1994;21(2):113–25. doi:10.1111/j.1365-2842.1994.tb01131.x
29. Hattori Y, Satoh C, Seki S, et al. Occlusal and TMJ loads in subjects with experimentally shortened dental arches. J Dent Res. 2003;82(7):532–6. doi:10.1177/154405910308200709
30. Witter DJ, Cramwinckel AB, van Rossum GM, et al. Shortened dental arches and masticatory ability. J Dent. 1990;18(4):185–9. doi:10.1016/0300-5712(90)90107-p
31. Daudt Polido W, Aghaloo T, Emmett TW, et al. Number of implants placed for complete-arch fixed prostheses: A systematic review and meta-analysis. Clin Oral Implants Res. 2018;29 Suppl 16:154–83. doi:10.1111/clr.13312
32. Gallucci GO, Avrampou M, Taylor JC, et al. Maxillary implant-supported fixed prosthesis: a survey of reviews and key variables for treatment planning. Int J Oral Maxillofac Implants. 2016;31 Suppl:s192–7. doi:10.11607/jomi.16suppl.g5.3
33. Heydecke G, Zwahlen M, Nicol A, et al. What is the optimal number of implants for fixed reconstructions: a systematic review. Clin Oral Implants Res. 2012;23 Suppl 6:217–28. doi:10.1111/j.1600-0501.2012.02548.x
ABOUT THE AUTHORS
Dr. Ramirez-Sosa received her BDS at Universidad Santa Maria in Venezuela, graduating in 2007. Then she broadened her expertise by completing a Certificate Program in Esthetic Dentistry from Universidad de Carabobo in 2010. For 7 years, she practiced dentistry in Venezuela, working in private and corporate sectors. Dr. Ramirez-Sosa continued her academic and professional journey at the Rutgers School of Dental Medicine (RSDM), where she completed her residency in prosthodontics in 2022. She can be reached via email at carmen.rsosa@gmail.com.
Dr. Shah is a board-certified periodontist working in New York. Dr. Shah completed her DDS at University of the Pacific in 2017. After completing dental school, she worked in private practice as a general dentist for 2 years. Then she continued to complete her periodontal residency at Rutgers University, graduating in 2023. During her postgraduate tenure, Dr. Shah presented at the Northeastern Implant Symposium, served as chief resident, and was awarded the Michael J. Deasy Endowed Scholarship. She can be reached at serenashahdds@gmail.com.
Dr. Howard J. Drew is a professor, director of implantology, and the vice-chairman in the Department of Periodontics at RSDM. He received his doctorate and degree in periodontics from RSDM. He has been awarded the RSDM Excellence in Teaching Award and Stuart Cook Master Educators Guild Award, and he received the prestigious American Academy of Periodontology Educator Award. Dr. Drew was inducted into the American College of Dentists, and he was awarded the RSDM Alumni Association Decade (1980s) Award. He has authored more than 30 publications and has lectured throughout the country. He was in full-time clinical practice for more than 25 years. He can be reached at drhjdrew@aol.com.
Dr. Alexander S. Drew is a maxillofacial prosthodontist with a private practice in Summit, NJ, limited to prosthodontics and restorative dentistry. He received his DMD degree from the University of Pennsylvania. After completing dental school, he earned a specialty certificate in prosthodontics and a masters of science degree from the Columbia University College of Dental Medicine where he was the chief resident. He then completed a subspecialty fellowship in maxillofacial prosthetics and was awarded a certificate from Memorial Sloan Kettering Cancer Center. Dr. Drew is a member of the American College of Prosthodontics and the ADA. He is an associate fellow of the American Academy of Maxillofacial Prosthetics and author to research publications in high-impact scientific journals. He can be reached at asdrew1@gmail.com.
Dr. Cappetta is the director of the postgraduate program of periodontics at RSDM. He received his doctorate from Rutgers University and his periodontics degree from Boston University. Dr. Cappetta has authored numerous publications in multiple periodontal journals, ranging from implant-supported prosthetics to novel mucogingival surgeries.He can be reached via email at cappeteg@sdm.rutgers.edu.
Dr. Falcon is a board-certified endodontist and director of the Advanced Specialty Education Program in Endodontics at RSDM in Newark, NJ. He has maintained private practice for 40 years. He has served nationally as District II Director on the American Association of Endodontists’ Board of Directors. He is presently President of the New Jersey Association of Endodontists. He can be reached at falconpa@sdm.rutgers.edu.
Disclosure: The authors report no disclosures.











