INTRODUCTION
When it comes to surgically correcting gingival recession, treatment options are numerous, and there is presently a wide body of literature demonstrating various techniques and materials. Common causes of recession often cited include but are not limited to: toothbrush abrasion, occlusion, oral anatomy, periodontal disease progression, and trauma from injury. Problems often associated with recession include root sensitivity, caries, mobility, and poor aesthetics. Gingival recession may also be found in the presence of other mucogingival defects, such as deficiencies in keratinized or attached gingiva.
While considering the treatment for gingival recession and its effect on periodontal health, it is important to note that recession accounts for one of the 2 components in calculating the clinical attachment level, which is the sum of the probing depth and recession present. Therefore, while clinicians can improve their patients’ clinical attachment level and ultimately their periodontal health by helping them to reduce pocket depths, they may also do so by correcting recession defects.
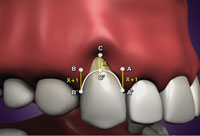
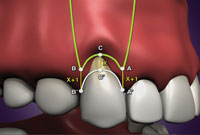
In the clinical setting, there are a number of nonsurgical and surgical treatment options for recession that are available to patients. The purpose of this article is to review these treatment options, and to present a case study to introduce a surgical technique for root coverage that possesses the advantages of minimizing pain, chair time, number of dental visits, costs, postoperative discomfort, and recovery time. This technique utilizes a coronally-advanced flap design (Figures 1 to 3) combined with a bone xenograft (PepGen P-15 Flow [DENTSPLY Tulsa Dental Specialties]). The surgical technique, clinical applications, and evaluation of results will be presented. Because this paper is a case study, the discussion will be limited to clinical applications.
Dental and Periodontal Problems Related to Gingival Recession
- Root sensitivity
- Poor plaque control
- Predisposition to caries
- Loss of clinical attachment level
- Compromised aesthetic result.
The above list is not all-inclusive but represents common clinical complications that may compromise the oral health of the patient.1 In addition to this list, however, there are a number of other clinical findings that are often found in addition to gingival recession. For example, recession may also be associated with a lack of keratinized and/or attached gingiva. In addition to the tissue quality surrounding recession defects, anatomical considerations such as frenum attachments and root dehiscences are also noted as well.
COMMON SURGICAL TREATMENT OPTIONS FOR RECESSION
When it comes to obtaining root coverage, there are a number of surgical techniques available to dentists, and the body of literature is vast in regards to the techniques involved: wound healing, nature of attachment, longevity, complications, etc. Here is a brief list of surgical options aimed at treating gingival recession:
- Guided tissue regeneration2-5
- Coronally repositioned flap6
- Free gingival graft7-10
- Subepithelial connective tissue graft11
- Acellular dermal graft12-14
- Vertical translation.15-16
In the authors’ practices, the decision on which of the above treatment options to perform for patients is a question of what is practical, reasonable, and of course, predictable for the patient. This criteria is mentioned only to point out that surgical options such as the subepithelial connective tissue graft (SECTG) are commonly used to treat gingival recession1 but may fail in regards to what we feel may be practical, reasonable, and predictable for the patient, depending on the severity of the recession and the number of teeth affected by recession.
The following case studies highlight patients who presented with various severities of recession, and for whom periodontal plastic surgery was successfully completed without the use of the patient’s palate as a donor site. Please note that it is not our intention to imply that the surgery technique performed on the patients in these case studies is the only acceptable form of treatment. It is our belief that there are often multiple modes of acceptable treatment that yield successful results.
Before presenting the case studies, it is important to note that the classification of recession used for the diagnoses was Miller’s classification.17 Below is a review of Miller’s classification:
Class I—Recession not extending to the mucogingival junction (MGJ). No interdental bone loss; 100% root coverage is possible.
Class II—Recession extends to or beyond the MGJ. No interdental bone loss; 100% root coverage is possible.
Class III—Recession extends to or beyond the MGJ. Interdental bone loss is present; only 50% to 75% root coverage is expected.
Class IV—Recession extends to or beyond the MGJ. Interdental bone loss is present that extends beyond the recession; no root coverage is expected.
CASE 1: GENERALIZED CLASS III RECESSION OF THE MAXILLA
A 51-year-old woman presented with generalized maxillary and mandibular Class III recession. As observed radiographically (Figure 4) and clinically (Figure 5), mild to moderate bone loss was evident, along with 3 to 7 mm of generalized recession. Her medical history was unremarkable, but her dental history was extensive. She had been diagnosed 20 years prior with generalized moderate chronic periodontitis. Combined with an aggressive tooth brushing habit, she had also experienced additional recession from osseous surgery for the reduction of periodontal pockets. Five years before, she had twice undergone periodontal plastic surgery in an attempt to cover the recession defects and restore the clinical attachment levels of her teeth. Unfortunately, both of these previous surgeries were unsuccessful in achieving her desired result, although it is unclear how much root coverage was actually gained from these previous root coverage procedures.
Pertinent findings from the periodontal examination revealed that no periodontal pockets were present, although the interproximal bone loss was moderate. In addition, the amount of keratinized and attached gingiva that was present measured approximately 2 mm and one mm, respectively. A high midline frenum attachment was observed between teeth Nos. 8 and 9.
Treatment Options
When deciding on treatment options for this patient, several choices were considered. During the examination process, she made it clear that because of her past experiences, she would not repeat the same procedures. Her objections were made due to finances and her lack of confidence in repeating the same procedures that had seemingly failed her before. Her first root coverage procedure was a SECTG taken from her palate and performed in all 4 quadrants during 4 visits. Her second root coverage procedure was an acellular dermal graft that was performed in the maxillary arch in only one visit.
 |
 |
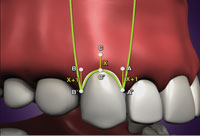 |
| Figures 1 to 3. Coronally advanced flap design. |
The patient’s past experience and present desires made treatment planning a challenge because of the body of research supporting the efficacy of both the SECTG11 as well as the acellular dermal graft.12-14 Without these 2 options, and inferring that any tissue taken from the palate was out of the question, the authors considered a relatively new, yet previously documented technique. We decided to attempt a root coverage procedure involving the use of PepGen P-15 Flow utilizing a coronally advanced flap (or vertical translation15-16) flap design (Figures 1 to 3).
What is PepGen P-15 Flow?
PepGen P-15 Flow is a peptide-enhanced anorganic bovine matrix xenograft that uses carboxy-methyl-cellulose as a carrier in a syringe delivery system. The use of PepGen P-15 flow has been found to improve the clinical outcomes of periodontal osseous defects,18 although its use in recession defects is relatively new.
When considering PepGen P-15 Flow as the material for this root coverage procedure, it is important to note that regenerative materials and their use in periodontal plastic surgery for recession have been documented previously.1,15-16 Although a curious concept at first, it is interesting to find that materials such as enamel matrix derivative15-16 and even the addition of growth factors such as rhPDGF-BB1 have been published previously to show the benefit of other materials besides autogenous tissue in correcting recession defects. However, unlike soft-tissue grafts, these relatively newer materials have demonstrated signs of regeneration while correcting recession defects.1,19 In regards to the use of the Pepgen P-15 Flow material itself, case studies have been previously published by the authors.20,21 The case reports primarily focus on root coverage as the outcome. The nature of the attachment to the root surface has not been studied.
Surgical Technique
Following local anesthesia with 4% articaine with 1:100,000 epinephrine, bleeding points were established with a periodontal probe that correlated to the amount of desired root coverage (Figures 1 to 3). These points equated to the tips of the “new” papillae that would be established. Next, using a No. 15 blade, 2 vertical incisions were made at the distal aspects of No. 3 and No. 14 (the terminal teeth for which root coverage is desired). These 2 incisions began at the bleeding points between Nos. 2 and 3 and Nos. 14 and 15 and extended apically beyond the mucogingival junction. A third incision was made that connected all of the bleeding points via a sulcular incision. A full-thickness mucoperiosteal flap was elevated to the MGJ. Beyond the MGJ, the flap was elevated via sharp dissection into the depth of the vestibule. Periosteal releasing incisions were also utilized to mobilize the flap. Note the severity of the root dehiscences once the flap was elevated (Figure 6). Using a No. 2 round diamond bur in a high-speed handpiece, the root surfaces were debrided with the goal of establishing clean root surfaces and to minimize (not eliminate) any root convexities that may have been present. The existing papillae were then de-epithelialized with the same No. 2 round diamond bur in order to expose the underlying connective tissue. The flap was then coronally advanced past the cemento-enamel junctions of the teeth and sutured with 4-0 Vicryl sutures using sling sutures (Figure 7). The distal vertical incisions were closed with the same suture material, utilizing interrupted sutures. In order to address the issue of the high frenum attachment between Nos. 8 and 9, as well as to provide an entry point for the delivery of the PepGen P-15 Flow bone graft, a frenectomy was performed next (Figure 8). Once the frenectomy incision was made, the bone graft material was introduced over the root surfaces using the syringe delivery system in which the bone graft is packaged (Figures 9 and 10). The frenectomy incision was then closed with a 4-0 chromic gut suture, achieving primary closure (Figure 11). The PepGen P-15 Flow material was then manually manipulated over the root surfaces.
 |
 |
|
Figure 4. Preoperative radiograph demonstrating moderate bone loss. |
Figure 5. Preoperative photo demonstrating severe recession. |
 |
 |
|
Figure 6. Flap reflection showing severe root dehiscences. |
Figure 7. Sling sutures aid the coronal advancement of the flap. |
 |
 |
|
Figure 8. Frenectomy performed immediately after suturing. |
Figure 9. Delivery of the PepGen P-15 Flow (DENTSPLY Tulsa Dental Specialties) bone graft. |
 |
 |
|
Figure 10. Graft in place. |
Figure 11. Final suturing. |
 |
 |
|
Figure 12. Two weeks postoperative. |
Figure 13. One year postoperative. |
The patient’s postoperative course was uneventful in regards to pain and discomfort. Minor bruising of the upper lip was reported. By the time the sutures were removed 14 days later, all bruising had disappeared (Figure 12). Pain control was achieved with Hydrocodone 5/500 (5 mg hydrocodone with 500 mg acetaminophen). The patient was also prescribed 0.12% chlorhexidine rinse to aid in plaque control. Specific oral hygiene instructions were no brushing on the facial surfaces of the grafted teeth, and a soft diet was recommended for the first week. The patient was provided with cotton tip applicators for plaque control. Two weeks after surgery, the sutures were removed (Figure 12). Normal brushing and flossing were not resumed until 8 weeks after surgery. The final evaluation of results was made after one year. As expected, 100% root coverage was not achieved, but a clearly large gain in clinical attachment was obtained and maintained at one year postoperatively (Figure 13).
CASE 2
 |
 |
|
Figure 14. Preoperative frontal view. |
Figure 15. Preoperative right side. |
 |
 |
|
Figure 16. Preoperative left side. |
Figure 17. Flap reflection revealing severe recession and root dehiscences. |
 |
 |
|
Figure 18. Coronal advancement of the flap secured by sling sutures. |
Figure 19. Frenectomy performed. |
 |
 |
|
Figure 20. PepGen P-15 Flow delivered to the upper right quadrant. |
Figure 21. PepGen P-15 Flow delivered to the upper left quadrant. |
 |
 |
|
Figure 22. Final suturing. |
Figure 23. Two-week postoperative of the maxillary arch and tooth No. 22. |
This young man presented to our office desiring to have his teeth “shortened” and “evened out.” He did not like the length of his teeth, and he felt that the asymmetry gave the illusion that his teeth were crooked. Upon clinical evaluation, it was observed that other than gingival recession on several teeth (Figures 14 to 16), this patient was in good periodontal health in regards to clinical parameters such as probing depths, bleeding upon probing, mobility, etc. Radiographically, no interdental bone loss was evident. Although there were several teeth with recession, he was primarily concerned with his upper teeth because of aesthetics. Upon further review, he became concerned with the recession on tooth No. 22 as well (Figure 14). Beyond the aesthetic concerns, the significance of the loss of clinical attachment level was reinforced to him. In addition, the other teeth with recession besides his maxillary teeth were identified for him as well. With so many teeth with recession, he was hoping that all of his procedures could be performed in one visit with one procedure. After considering the same treatment options mentioned previously, he ultimately decided on correcting the recession defects with PepGen P-15 Flow, utilizing the coronally advanced flap design in Figures 1 to 3. The same technique was followed as described in Case 1. The results that followed are pictured in Figures 17 to 24. The final result at one year after surgery demonstrates complete root coverage and the re-establishment of gingival symmetry and healthy gingiva (Figure 24).
CASE 3
 |
 |
|
Figure 24. One year postoperative. |
Figure 25. Preoperative frontal view revealing recession on teeth Nos. 8 to 12. |
 |
 |
|
Figure 26. Two weeks postoperative. Note that the final restorations have been delivered. |
Figure 27. Two years postoperative. Note the complete root coverage, despite poor oral hygiene and marginal inflammation. |
In the final case presented, the benefit of using PepGen P-15 Flow and a coronally advanced flap for the treatment of severe recession in improving the quality and results of restorative dentistry is highlighted. In this woman’s initial presentation, she was wearing provisional restoration on teeth Nos. 8 and 9 and demonstrated recession on teeth Nos. 8 to 12 (Figure 25). A Class V composite restoration was present on the facial of No. 11. In her restorative treatment plan were full coverage crowns on teeth Nos. 2 to 15 and 18 to 29. Before her crown preparations, she desired to have the gingival recession corrected in order to re-establish gingival symmetry and provide a more aesthetic result with her new restorations. Once again following the same technique that was outlined previously, Figure 26 shows the result of the root coverage surgery at 2 weeks postoperatively, just prior to having the sutures removed. At the 2-week visit, please note that the final restorations had already been delivered. Under normal circumstances, the authors recommend a healing period of 12 weeks following root coverage surgery before making final impressions. The final result in Figure 27 was taken at 2 years postoperatively. Despite less than optimum oral hygiene, the recession defects continue to be covered. Some plaque-induced marginal inflammation is noted around teeth Nos. 8 and 9 as well as around the lower incisors.
DISCUSSION
Periodontal plastic surgery procedures, such as root coverage surgery, provide the patient with several benefits, including decreased root sensitivity, decreased risk of root caries, clinical attachment level gain, and improved aesthetics. These results may be accomplished in several ways. Perhaps most commonly, the use of palatal tissue taken from the patient is transplanted from the palate to the recession defect.1 Common examples of palatal grafts include free gingival grafts and SECTGs. Although SECTGs have proven to be predictable, successful, and aesthetic, there are disadvantages that should be noted. First, palatal grafts require 2 surgical sites, which may contribute to increased morbidity and postoperative discomfort for the patient. Second, because of anatomical variances between patients, the amount of tissue that may be procured from the palate may be limited. This is especially important when considering the treatment of multiple recession defects such as those shown in this paper. Depending on the number of teeth to be treated or even the severity of the recession defects, both sides of the palate may be used, and oftentimes, multiple visits or procedures may be required.
The primary advantage of utilizing an allograft, or in the case of PepGen P-15 Flow, a xenograft, is the ability to treat multiple teeth of varying severity in a shorter amount of time, in fewer visits, while eliminating a second (or even a third) surgical site. As documented in previous papers and in this presentation, the results of the surgery are predictable, stable, and aesthetic. Moreover, in all 3 of the cases above, only one visit with one procedure was required. The bone graft material and the flap design described have anecdotally been very tolerable to patients, who typically report a quick recovery and minimal pain. Common events that are occasionally observed during the healing process include swelling, bleeding, and light bruising.
In regards to the nature of the attachment, the use of a bovine xenograft over recession defects is counterintuitive to the principles of periodontal regeneration. Please note that no claim has been made to suggest that any new bone, cementum, or periodontal ligament forms from this procedure. However, it is important to mention that regenerative products and materials have recently been found in the literature to demonstrate signs of regeneration when used over recession defects. One example of this is the use of enamel matrix derivative. Even more recently, the use of growth factors and tricalcium phosphate has been suggested to regenerate bone, cementum, and periodontal ligament fibers.1 Based on this new evidence, one area of future research with PepGen P-15 Flow will be to examine more closely the nature of the attachment to the root surface. Thus far, the clinical applications of PepGen P-15 Flow for correcting recession defects shows promise for the future.
CONCLUSION
Despite a plethora of periodontal plastic surgery techniques that are available for treating gingival recession defects, there are some cases in which the number of recession defects involved, the severity of their involvement, or simply patient desires make options such as techniques involving the palate impractical or unreasonable. In regards to being practical, reasonable, and predictable, the use of PepGen P-15 Flow improves the quality of patient care by successfully correcting defects while minimizing the amount of surgical trauma, time, and number of visits. Although an accurate and thorough diagnosis is necessary, PepGen P-15 Flow is a material that may be used to correct multiple severe recession defects. Besides the oral health benefits to patients, this technique also enhances the quality of restorative dentistry by correcting recession that would result in gingival asymmetry and disrupt the harmony of otherwise aesthetic dentistry.
References
- McGuire MK, Scheyer ET, Schupbach P. Growth factor-mediated treatment of recession defects: a randomized controlled trial and histologic and microcomputed tomography examination. J Periodontol. 2009;80:550-564.
- Tinti C, Vincenzi G, Cortellini P, et al. Guided tissue regeneration in the treatment of human facial recession. A 12-case report. J Periodontol. 1992;63:554-560.
- Cortellini P, Clauser C, Prato GP. Histologic assessment of new attachment following the treatment of a human buccal recession by means of a guided tissue regeneration procedure. J Periodontol. 1993;64:387-391.
- Harris RJ. A comparison of 2 root coverage techniques: guided tissue regeneration with a bioabsorbable matrix style membrane versus a connective tissue graft combined with a coronally positioned pedicle graft without vertical incisions. Results of a series of consecutive cases. J Periodontol. 1998;69:1426-1434.
- Pini Prato G, Tinti C, Vincenzi G, et al. Guided tissue regeneration versus mucogingival surgery in the treatment of human buccal gingival recession. J Periodontol. 1992;63:919-928.
- Bernimoulin JP, Lüscher B, Mühlemann HR. Coronally repositioned periodontal flap. Clinical evaluation after one year. J Clin Periodontol. 1975;2:1-13.
- Miller PD Jr. Root coverage using the free soft tissue autograft following citric acid application. III. A successful and predictable procedure in areas of deep-wide recession. Int J Periodontics Restorative Dent. 1985;5:14-37.
- Caffesse RG, Guinard EA. Treatment of localized gingival recessions. Part II. Coronally repositioned flap with a free gingival graft. J Periodontol. 1978;49:357-361.
- Matter J. Free gingival graft and coronally repositioned flap. A 2-year follow-up report. J Clin Periodontol. 1979;6:437-442.
- Maynard JG Jr. Coronal positioning of a previously placed autogenous gingival graft. J Periodontol. 1977;48:151-155.
- Langer B, Langer L. Subepithelial connective tissue graft technique for root coverage. J Periodontol. 1985;56:715-720.
- Harris RJ. The connective tissue and partial thickness double pedicle graft: a predictable method of obtaining root coverage. J Periodontol. 1992;63:477-486.
- Aichelmann-Reidy ME, Yukna RA, Evans GH, et al. Clinical evaluation of acellular allograft dermis for the treatment of human gingival recession. J Periodontol. 2001;72:998-1005.
- Harris RJ. A comparative study of root coverage obtained with an acellular dermal matrix versus a connective tissue graft: results of 107 recession defects in 50 consecutively treated patients. Int J Periodontics Restorative Dent. 2000;20:51-59.
- Chen L, Cha J, Ho CH. A three-point-translation technique for root coverage with 4-year follow-up. Dent Today. 2002;21:112-115.
- Chen L, Cha J, Guiha R, et al. Root coverage with enamel matrix derivatives. Compend Contin Educ Dent. 2002;23:797-808.
- Miller PD Jr. A classification of marginal tissue recession. Int J Periodontics Restorative Dent. 1985;5:8-13.
- Yukna RA, Krauser JT, Callan DP, et al. Multi-center clinical comparison of combination anorganic bovine-derived hydroxyapatite matrix (ABM)/cell binding peptide (P-15) and ABM in human periodontal osseous defects. 6-month results. J Periodontol. 2000;71:1671-1679.
- McGuire MK, Cochran DL. Evaluation of human recession defects treated with coronally advanced flaps and either enamel matrix derivative or connective tissue. Part 2: Histological evaluation. J Periodontol. 2003;74:1126-1135.
- Wong DH, Cha J. A periodontal-restorative approach to achieve an esthetic outcome in worn dentition. Cont Esthet Rest Pract. 2007;11:20-26.
- Wong DH, Chen L, Cha J. A review of the vertical translation technique for the successful treatment of recession: clinical applications. Cont Esthet Rest Pract. 2006;10:46-55.
Dr. Kendrick is in private practice in Midwest City, Okla, and is an instructor at the Tulsa Implant Institute. He can be reached via e-mail at skend22@hotmail.com.
Dr. Wong is in private practice in Tulsa, Okla, and is an instructor at the Tulsa Implant Institute. He is a Board Certified Periodontist and can be reached via e-mail at the address david@tulsagums.com.
Disclosure: The authors have not received any financial benefit for the submission of this article or the mention of any products.











