INTRODUCTION
For patients who present with Stage IV advanced periodontitis, comprehensive management of their dental conditions can be challenging because the goal of therapy is not only to address their periodontal condition and help patients return to health but to also address the aesthetic and functional rehabilitation of their condition and long-term maintenance to ensure continued health. Patients with Stage IV periodontitis are at significant risk of edentulism if they are not treated or receive inadequate care. Therefore, careful planning, efficient therapy, and continued supportive care throughout and after therapy are essential to helping these patients keep their teeth. This article looks at a multi-specialty approach to the management of a patient with advanced (Stage IV) periodontitis.
In 2017, the World Workshop on Periodontal and Peri-implant Diseases and Conditions defined periodontitis based on stage and grade. While “stage” describes the severity, complexity, extent, and distribution of disease, “grade” defines the disease’s biologic features, including the rate of progression, rate of potential poor outcome, and impact of periodontal disease treatment on the patient’s systemic health.1,2 While “grade” involves 3 categories based on evidence of progression as slow, moderate, and rapid progression (Stage A to C) with risk factors as grade modifiers, “stage” categorizes periodontitis based on severity and complexity into Stage I to Stage IV. 1
Stage III and Stage IV describe advanced periodontitis. Patients in both categories are categorized by interdental attachment loss of 5 mm or more, with radiographic evidence of bone loss that extends to mid-root and beyond.1,2 Complexity for Stage III and Stage IV periodontitis patients involves more than 6 mm of probing depth, vertical bone loss of 3 mm or more, and furcation involvement that is type II or type III. For Stage III patients, it also involves tooth loss involving 4 or more teeth and a moderate ridge defect, while for Stage IV patients, it involves tooth loss involving 5 or more teeth and a severe ridge defect.1,2 Additionally, Stage IV periodontitis patients require complex rehabilitation due to masticatory dysfunction, secondary occlusal trauma with tooth mobility of 2 or more degrees, severe ridge defect bite collapse, flaring of teeth, and less than 20 remaining teeth (<10 pairs) in both arches.1,2
The need for complex rehabilitation sets Stage IV patients apart from Stage III patients, and the management of Stage IV patients is significantly more complicated. Early diagnosis is essential, and having a treatment plan that is started immediately rather than delayed is important to preventing further loss of teeth and complications with rehabilitation to restore aesthetics and function.3,4 Stage IV periodontitis patients have a higher risk of periodontal disease-related tooth loss compared to Stage I patients in studies involving a follow-up period of 10 to 30 years (hazard ratio of 3.73), as well as a higher risk for pathologic tooth migration and other functional consequences.3
Recommendations for Management of Advanced (Stage IV) Periodontitis Patients
In 2022, the European Federation on Periodontology (EFP) developed S3-level clinical practice guidelines implementing an interdisciplinary approach to rehabilitate Stage IV periodontitis patients due to the fact that failure to treat or inadequate treatment of these patients can result in additional loss of periodontal tissue, further tooth loss, and the potential for complete edentulism.3 The goal of their guidelines is to summarize evidence-based recommendations for individual intervention involving a multi-disciplinary approach to Stage IV periodontitis.3
Based on their recommendations, assessment of Stage IV periodontitis patients comprises 5 critical dimensions3:
- Evaluation of the amount of periodontal breakdown, patient function, and aesthetics; completing the periodontal exam, charting, and appropriate x-rays; and functional and aesthetic assessment checking for hypermobility, tooth vitality, secondary occlusal trauma, stable posterior stops, fremitus, subjective/objective assessment of chewing function, aesthetics, and phonetics.
- Assessment of the number of teeth lost due to periodontal disease using a history of probable cause of tooth loss.
- The prognosis of individual teeth. Establishing tooth prognosis for Stage IV periodontitis patients is important, especially when differentiating between teeth with questionable vs hopeless prognoses.
- Restorative factors, such as the extent of edentulous spaces, distribution, and restorability of retained teeth, including the technical complexity of planned prostheses and interventions that require dental implants based on adequate ridge dimensions.
- The prognosis of overall care, meaning the overall case prognosis has to be established using individual susceptibility of the patient via primary grade criteria, which also includes the probability of disease recurrence or progression.
In categorizing patients who have Stage IV periodontitis, 4 major phenotypes were identified:
- Case type 1. Patients with tooth hypermobility due to secondary occlusal trauma that can be corrected without tooth replacement.
- Case type 2. Patients with pathological tooth migration characterized by tooth elongation, drifting, and flaring, which is amenable to orthodontic correction.
- Case type 3. Partially edentulous patients who can be prosthetically restored without full-arch rehabilitation.
- Case type 4. Partially edentulous patients with a dentition who need full-arch rehabilitation using either a tooth- or an implant-supported or -retained prosthesis.
For Stage IV periodontitis patients, the “no-treatment” option is highly discouraged due to the potential for complete edentulism.3 In recommending therapy for Stage IV patients, Herrera et al3 advised the use of recommendations made by the EFP for treating Stage I to III patients and added modifications for Stage IV patients. Sanz et al5 recommended the following steps for treating Stage I to Stage III patients:
- Step 1. Guiding behavioral change to have patients undertake successful supragingival plaque control. The goal is to build motivation and adherence, find ways to circumvent barriers, and develop skills for dental plaque removal.
- Step 2. Controlling, reducing, and eliminating bacterial biofilm and calculus involving subgingival instrumentation with or without adjunctive physical and chemical agents, local/systemic host modulation, adjunctive subgingival local delivered antimicrobial agents, or adjunctive use of systemic antimicrobials.
- Step 3. Therapy to address pockets that are more than 4 mm deep and bleeding and/or the presence of deep pockets (≥6 mm) with the goal of gaining further access for debridement, regeneration, and resection of lesions that add complexity to the management of periodontitis, such as intrabony and furcation defects. The goal is to meet the endpoints of therapy prior to starting supportive maintenance, although it might not be completely accomplished for Stage III patients.
- Step 4. Supportive therapy. The goal of therapy is aimed at maintaining periodontal stability in all treatment patients using steps 1 and 2.
In 2014, Trombelli et al6 looked at the impact of professional plaque removal performed during supportive therapy and found that the extent of patient adherence to professional mechanical plaque removal significantly impacted tooth mortality, with patients who attended regular maintenance visits showing tooth loss of 0.6 teeth vs 1.8 for those who did not over a 5-year period. Seirafi et al7 found that in private practice in Iran, bleeding on probing (BOP) was associated with increased tooth loss, and erratic-compliant patients had more BOP than regular-compliant patients. Campos et al8 concluded from a meta-analysis of multiple studies that there was a 26% increase in tooth loss for noncompliant patients vs patients compliant with supportive periodontal therapy. Kim et al9 found increased tooth loss (26% and 30%, respectively) with noncompliant and erratic-compliant patients compared to completely compliant supportive-maintenance patients (4%) in the Korean population. Hirata et al10 found that patients with prior loss of 8 or more teeth were more likely to have further tooth loss during supportive maintenance.
Based on these and other findings, the recommendation for treating Stage IV periodontitis patients is supportive therapy before, during, and after active therapy to improve oral hygiene and patient motivation.3 In addition to the recommendations for Stage I to Stage III periodontitis patients (steps 1 to 4), Herrera et al3 added these guidelines for the clinical management of Stage IV patients:
- Temporary control of secondary occlusal trauma (extracoronal splinting, relief of fremitus by limited occlusal adjustment)
- Orthodontic therapy (usually for flared teeth and other pathologic tooth migrations)
- Rehabilitation of one or multiple tooth-delimited edentulous spaces
- Rehabilitation of unilateral/bilateral posterior free edentulous sites
- Tooth-supported, full-arch, fixed prostheses
- Tooth-supported, full-arch, removable dental prostheses
- Implant-supported, full-arch, fixed dental prostheses
- Implant-supported, removable prostheses.
Recommendations for Treating Advanced (Stage IV) Periodontitis Patients
In management of different categories of Stage IV periodontitis patients, the treatment pathways include the following3:
- Case type I. Patient with hypermobility due to secondary occlusal trauma without requiring teeth replacement. Therapy involves temporary teeth splinting or initial limited occlusal adjustment. The need for longer-term splinting occurs only after steps 1 and 2 of periodontal therapy are completed.
- Case type 2. Pathologic tooth migration causing tooth elongation, drifting, or flaring. Therapy is orthodontic therapy planned during step 2 and, in some cases, step 3. The actual orthodontic therapy is recommended to start after shallow maintainable pockets are attained and inflammation is controlled during the supportive-maintenance phase.
- Case type 3. Partially edentulous patients who can be prosthetically restored without full-arch rehabilitation. The timing of intermediate restoration is planned carefully based on the individual or the case in keeping with the patient’s wishes and aesthetic considerations. Interim restorations are usually utilized after step 2 or 3, depending on the situation. Definitive restorations or implants are usually performed during step 4 after successful completion of step 3.
- Case type 4. Partially edentulous patients who need to be restored by full-arch rehabilitation, either tooth- or implant-supported, with either fixed or removable prostheses. For these patients, the interim prosthesis occurs after the completion of step 1. Step 2 is performed with the interim prosthesis in place. Definitive restoration occurs after stage 3 with successful completion of periodontal therapy and control of periodontal inflammation.
CASE REPORT
A healthy, 54-year-old African American female presented as a patient with Stage IV periodontitis, case type 4. The patient was very concerned about the health of her gums, aesthetics, function, and phonation with her anterior teeth (Figures 1 and 2). Following completion of steps 1 and 2, interim restorations were completed for the patient involving a temporary bridge from tooth No. 5 to 12. Following step 3, extraction of teeth Nos. 6 to 11 was performed, with implants replacing teeth Nos. 6 to 9 (4.0-mm × 12-mm BioHorizon implants) and No. 10 (a 4-mm × 10.5-mm BioHorizon implant). Figures 3 to 8 show surgical management. Figures 9 to 11 show restorative rehabilitation of her dentition. The patient was very motivated with oral hygiene and maintenance visits, and 4 years later, she presented to see us and was able to save all of her remaining teeth.



Figures 1 and 2. Initial patient presentation.

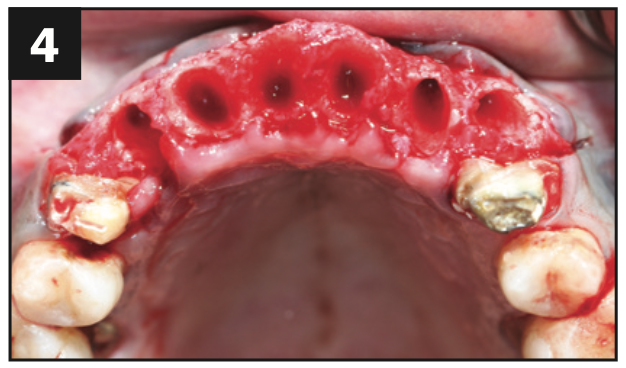
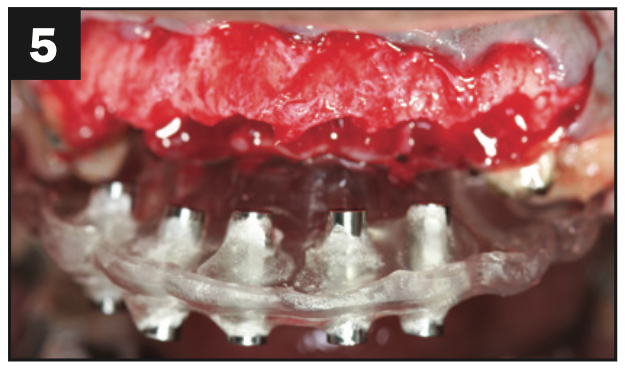
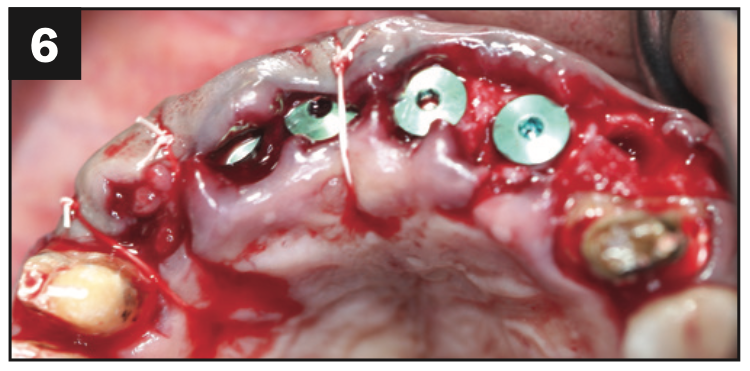
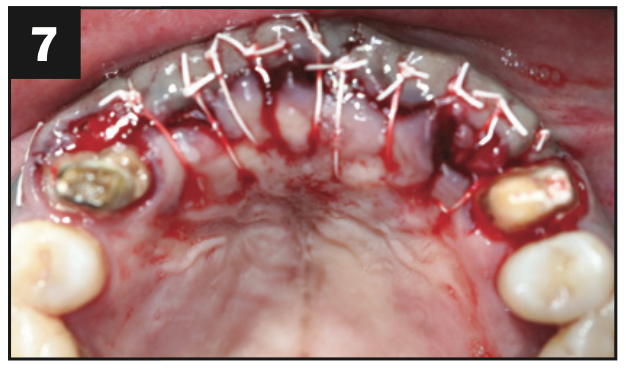
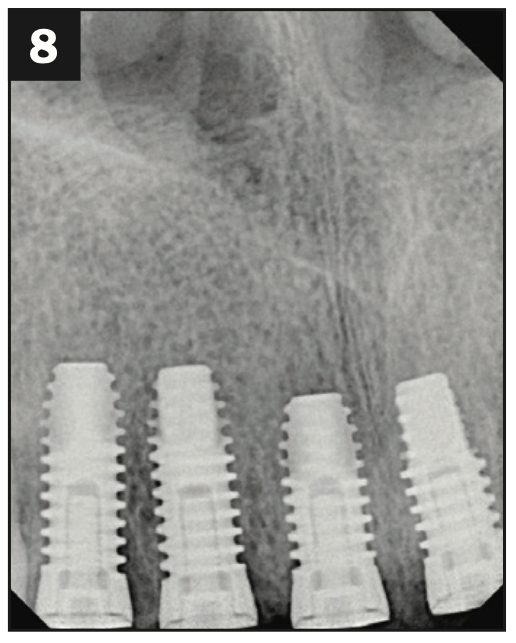
Figures 3 to 8. Surgical pictures.



Figures 9 to 11. Four-year postoperative pictures showing restorative rehabilitation.
CONCLUSION
A high level of complexity is involved in the treatment of patients with Stage IV advanced periodontitis to ensure that they can be able to achieve periodontal health as well as be able to maintain function and aesthetics. The ability for these patients to remain motivated and compliant with their care is also essential to their being able to retain their dentition long-term. Recommendations made by Herrera et al3 include that the patients must be informed in detail about their periodontal condition, including their treatment options and risks. They also discourage early extraction of questionable teeth that might be able to respond to therapy and recommend completing steps 1 to 3 of periodontal therapy, ensuring completion of periodontal therapy prior to orthodontics, long-term tooth splinting, tooth-supported fixed and removable prostheses, and implant-supported fixed and removable prostheses.3,5 In planning restorations for patients with Stage IV periodontitis, it is important that restorations be designed to achieve function and aesthetics using a multi-disciplinary approach. It is also essential that patients are highly motivated with their oral hygiene and supportive maintenance.
REFERENCES
1. Papapanou PN, Sanz M, Buduneli N, et al. Periodontitis: Consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol. 2018;89(Suppl 1):S173–82. doi:10.1002/JPER.17-0721
2. Tonetti MS, Greenwell H, Kornman KS. Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. J Periodontol. 2018;89(Suppl 1):S159–72. doi:10.1002/JPER.18-0006. Erratum in: J Periodontol. 2018;89(12):1475.
3. Herrera D, Sanz M, Kebschull M, et al; EFP Workshop Participants and Methodological Consultant. Treatment of stage IV periodontitis: The EFP S3 level clinical practice guideline. J Clin Periodontol. 2022;49(Suppl 24):4-71. doi:10.1111/jcpe.13639
4. Rasaeipour S, Siadat H, Rasouli A, et al. Implant rehabilitation in advanced generalized aggressive periodontitis: a case report and literature review. J Dent (Tehran). 2015;12(8):614–20.
5. Sanz M, Herrera D, Kebschull M, et al; EFP Workshop Participants and Methodological Consultants. Treatment of stage I-III periodontitis-The EFP S3 level clinical practice guideline. J Clin Periodontol. 2020;47(Suppl 22):4-60. doi:10.1111/jcpe.13290. Erratum in: J Clin Periodontol. 2021;48(1):163.
6. Trombelli L, Franceschetti G, Farina R. Effect of professional mechanical plaque removal performed on a long-term, routine basis in the secondary prevention of periodontitis: a systematic review. J Clin Periodontol. 2015;42(Suppl 16):S221–36. doi:10.1111/jcpe.12339
7. Seirafi AH, Ebrahimi R, Golkari A, et al. Tooth loss assessment during periodontal maintenance in erratic versus complete compliance in a periodontal private practice in Shiraz, Iran: a 10-year retrospective study. J Int Acad Periodontol. 2014;16(2):43-9. Erratum in: J Int Acad Periodontol. 2014;16(3):77.
8. Campos ISO, de Freitas MR, Costa FO, et al. The effects of patient compliance in supportive periodontal therapy on tooth loss: A systematic review and meta-analysis. J Int Acad Periodontol. 2021;23(1):17-30.
9. Kim SY, Lee JK, Chang BS, et al. Effect of supportive periodontal therapy on the prevention of tooth loss in Korean adults. J Periodontal Implant Sci. 2014;44(2):65-70. doi:10.5051/jpis.2014.44.2.65
10. Hirata T, Fuchida S, Yamamoto T, et al. Predictive factors for tooth loss during supportive periodontal therapy in patients with severe periodontitis: a Japanese multicenter study. BMC Oral Health. 2019;19(1):19. doi:10.1186/s12903-019-0712-x
ABOUT THE AUTHORS
Dr. Soolari received his DMD degree in 1990 from the University of Mississippi School of Dentistry where he received multiple awards. He received his specialty training in periodontics from Eastman Dental Center and his MS degree from the University of Rochester in New York. He has been a Diplomate of the American Academy of Periodontology since 1997. Dr. Soolari was a consultant with National Naval Medical Center Postgraduate Periodontics in Bethesda, Md, and a former clinical associate professor at the University of Maryland. He is in private practice at Soolari Dentistry in Silver Spring, Md. He can be reached at asoolari@gmail.com.
Dr. Obiechina completed her training in periodontics and implant dentistry at Columbia University in 2001. She received her DMD degree from the University of Pittsburgh in 1998. She is the recipient of the Melvin Morris Award for clinical excellence in periodontics from Columbia University as well as the Northeast Regional Board Student Award for excellence in periodontics. She has given multiple seminars for dentists on periodontics and implant dentistry and has published works, including books on dental implant therapy and periodontics for dentists as well as articles for multiple peer-reviewed journals. She remains involved in active private practice at Shady Grove Smiles in Gaithersburg, Md, in addition to being an educator. She can be reached at drobiechina@yahoo.com.
Disclosure: The authors report no disclosures.












