The wave of CAD/CAM dentistry is here. Perhaps you are riding it or likely watching from the sideline. For those of you watching, this article will move you to consider riding the wave. For those of you currently using CAD/CAM, this article will enhance your ability to create/generate great crowns that fit precisely under a partial denture.
One of the most frustrating things a restorative dentist or prosthodontist faces in practice is trying to obtain an adequate fit and retention of a removable partial denture (RPD) to its abutment tooth when the abutment must be crowned. The use of a CAD/CAM technique to create a crown in this situation is invaluable, predictable, and beneficial to both patient and practitioner. CAD/CAM enables the crown to be made in one appointment, eliminating the pitfalls of impression taking, surrender of the partial by the patient, stent making in the case where the patient cannot give up the partial for cosmetic reasons, and remakes when the crown does not seat with the partial. The technique described in this article uses the CEREC CAD/CAM system (Sirona Dental).
The technique is more advanced than a standard crown design, however, it is not insurmountable. The time frame will not be longer than the usual time you spend in a CEREC appointment. The example here is tooth No. 13. It had a large amalgam restoration and endured a horizontal fracture (Figure 1). The design technique to crown this must be correlation. Any missing tooth structure must be built up to the rest seat and clasp area (Figures 2a and 2b). Sometimes the existing tooth-RPD relation is not good. This is fairly common as alloys or composites may have been placed after the RPD was originally delivered. At this time, if there are any voids or poor clasp-to-tooth areas, build them up to ideal position using some composite.
 |  |
Figure 1. A horizontal fracture of tooth No. 13 requires a crown. | Figure 2a. Composite buildup to fit to framework and occlusion. |
 |  |
Figure 2b. Occlusal view of buildup. | Figure 3. Powdering the composite buildup to acquire an image for the CEREC restoration using titanium dioxide powder. |
 |  |
Figure 4. The use of caries indicator to identify any caries. | Figure 5. Preparation completed allowing space for the clasp and rest seat. |
The other common situation is a broken cusp or marginal ridge under the rest seat that fractures off and now must be restored with a crown. Again, build these areas up with composite. This is accomplished by first having the RPD out of the mouth, then build up the tooth with composite paste. Try to gauge the amount needed so that only a slight amount will be expressed from around the clasp and rest area when the RPD is seated. Seat the RPD onto the uncured composite paste. Gently remove the excess with an explorer, making sure to draw toward the framework areas and not away, as that would pull the composite from the framework and cause an error of adaptation. When the composite is well adapted and cleaned up, cure it. Then remove the RPD and cure the remainder. Bonding the composite to the tooth is desirable. Reseat the RPD and check again for voids, filling where needed. Make a mental note of the clasp and rest position and the path of insertion. You will want to hold the acquisition camera in the same plane/angle as the insertion path. Finally, check the occlusion to ensure that your buildup is not overdone. Remove the RPD and powder the tooth (Figure 3).
It is important to know that CEREC uses all the data in the images taken to propose restorations and make correlations. The software will not differentiate tooth from buccal mucosa. In this technique, image acquisitions are crucial to the final fit. Therefore, the area that will be imaged should not contain any cotton rolls, mirrors, or other retraction devices. Doing so would not allow the images to be a perfect correlation. Take 3 images at a minimum; one image each from the occlusal, slightly buccal, and slightly lingual. It is important to capture the area where the clasp is seated on the tooth (this is where you recall the mental note you made in the earlier step).
Now tooth preparation can begin. As an aside, whether or not the tooth has been fractured, it is important to use a caries detecting dye (Figure 4) after removal of all the existing restorative and build-up materials. Using depth cuts for all surfaces is mandatory, as it is the only way to ensure proper thickness of the final restoration. In correlation mode, the restoration is determined from the original tooth shape and size, hence the thickness of the restoration depends upon the ability of the doctor to remove an adequate amount of tooth structure. A coarse chamfer diamond with a tip of 1.6 mm was used in this case. The minimal amount of reduction needed is 1 mm on the axial walls and 2 mm on the occlusal. Check the occlusal clearance with the use of a clearance tab. Also check the clearance under the rest and clasp areas by inserting the RPD over the preparation (Figures 5 and 6). If any inadequate space exists, make appropriate adjustments. When you are confident of the reduction, powder the preparation and take the image.
 |  |
Figure 6. Confirming the space available under the crown with RPD in place. | Figure 7a. Seating of the CEREC crown under the RPD. |
 |  |
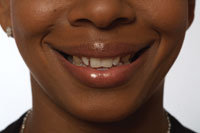
Figure 7b. Occlusal view of CEREC crown seated. Note the excellent adaptation to the clasps. | Figure 8. Cemented crown one hour and 10 minutes after beginning treatment. |
 |  |
Figure 9a. The C-stat matrix; quick-set bite registration seats on adjacent teeth to ensure repeatable angulation on imaging. | Figure 9b. C-stat with putty showing how putty interlocks onto C-stat matrix. |
At this point it is helpful to enlarge the preoperative image so that it can be compared to the active camera by aligning the 2 to obtain excellent correlation. You must be careful in alignment, as the proposed crown restoration will be based on the preoperative image. Any significant variance will result in either poor occlusion or poor adaption of the crown to the rest/clasp areas (Figures 7a to 8). Alternately, a good way to ensure homogeneity between the occlusion and preparation images is to use a purple C-stat from Dentistry by Design (Figures 9a and 9b). This method utilizes a bite registration material on adjacent teeth to lock in the position and angulation of the camera in both occlusion and preparation images. In Figures 10a to 11, the crown is on No. 6. Figure 12 shows how closely one can adapt the crown surface to the partial.
 |  |
Figure 10a. Tooth No. 6 crown prep. The mesiofacial had a large carious lesion removed and composite buildup completed. | Figure 10b. A No. 6 CEREC crown placed, margins checked, then the RPD was placed to check adaptation as in Figure 12. |
 |  |
Figure 11. CEREC on tooth No. 6 completed. | Figure 12. Tooth No. 6 closeup occlusal; notice close adaptation of clasps. |
DESIGNING THE CROWN
The steps in designing the crown are similar to any crown using CEREC, with the biggest difference being the management of the copy line. But first check your parameters. It is good practice to check your parameter settings every time you design a restoration. This is particularily true in an office with more than one doctor using the CEREC unit. Parameters are changed for various restorations, and if you performed a veneer or onlay the last time you used the unit, your parameters will be different this time. Of the most concern for this restoration is to have the occlusal offset set at zero. The other setting critical to this procedure is the emergence profile. For this molar example, setting is made to 3. This helps with the contour and clasp adaptation. When parameter settings are completed, check the preparation image for any extraneous information or “junk” and remove or edit under the design tab using “correction of optical impressions.”
Now draw the bottom line. In the proximal line screen, trace the proximal line (purple line) to the exact shape of the preoperative image that is shown in gray. Next, in the copy line screen, draw the copy line (green line) to include all areas where the clasp and rest seat are located; this means that the green line will come over the cusp and gingivally below the area where the clasps are buccally and lingually; likewise on the proximal surface where the rest seat is located. To do this you need to roll the model buccal and lingual as you draw the lines. This is again where your mental note of the position of the clasps on the tooth in the first steps is called upon. When the copy line is in good postion click “next” and proceed.
Now the restoration is proposed. Click on “occlusion” in the tool box. Look for the image to become speckled with light and dark gray. This indicates that the preoperative and preparation images are identical and the restoration can be trusted. What if your image is not speckled? Use the form tool to either add or remove increments until the pattern appears. If your parameter setting for occlusal offset is not set at zero, the occlusal table (everything inside the green line) will be dark gray with a positive offset number, or light gray with a negative offset number. The technique of looking for the speckling to tell you the adaption of the 2 images will be unreliable.
The priority for the success of this restoration is the copying line. After this is accomplished, check and adjust the contacts, contour, shape, and form. Be sure not to alter anything in the copying line areas. Use the shape tool to adjust cusp tips if necessary.
In checking the contact points, the author sets his contact point strength at 50 µm and sets the contact zone to yellow and green. This results in perfect contacts upon completion of polishing. In checking the contact point where the rest seat is, some rest seats sit in the contact zone. Be mindful of this and do not add contact to the area. Doing so will result in lengthy adjustment on delivery or future fracture on the proximal ridge. Make any final adjustments using the form tool. Insoftware versions 3.01 (and later), the size of the brush is easily accessible on the toolbox. If you do not have this version simply place the smoothing hand on the restoration and right click, holding down as you roll the trackball up and down to change the size of the brush. Make a final check of the occlusion (clicking on the occlusion button in the tool box) after all adjustments are made and make sure no alterations have occurred in the green zone. Now go to the mill menu.
In the milling preview, you should have the minimal thickness set at 1,000 µm (which is 1 mm); any red that is displayed in the preview indicates inadequate thickness. Use this red zone and setting to your advantage for all restorations. Remember that an axial wall can have a minimal thickness of 0.8 mm, and so a little red in the cervical one third is acceptable. Just remember to roll the cursor over it and make sure you do, in fact, have 0.8 mm. Check under the rest seat to confirm a thickness greater than 1 mm. At this point, these are confirmatory steps. Any inadequate areas will necessitate repreparation and design. This is why good visualization, depth cuts, and image acquisition technique are so important. In this preview, be very conscious of clasp location and thickness. If you make any adjustments here, you will only be removing them upon delivery.
Once milling is completed, finish, polish and check fit and occlusion as with any restoration. It is very satisfying to be able to provide the retro-fit crown under a partial denture in one visit. Knowing that you have alleviated the anxiety of delivering the crown from the lab, uncertain of how well it will fit when it is in the mouth, is of great satisfaction to the dental team. Being able to allow a patient to keep their partial denture as opposed to sending it to a lab for 2 weeks is a superior service to the patient. One caveat is that we are copying an existing tooth shape and form, thus we forego the ability to create an “ideal” restoration with perfect contour, shape, (sometimes) shade, and optimal appearance. But in reality the restoration is always better than what the patient had for tooth structure originally, and in the end it is the perfect solution to the challenges that the retro-fit crown presents.
Should you have any specific questions or concerns with your retro-fit experience please contact the author at pcschoenbeck@yahoo.com.
Dr. Schoenbeck maintains a practice in northern New Hampshire and is a medical staff member of the Androscoggin Valley Hospital. He is a sustaining member of the AACD and also a member of the ACE, ADA, AAHD, and AGD. He is a 1994 graduate of Tufts University School of Dental Medicine, and completed his general practice residency at Boston VA Hospital in 1995. He has written articles and presents lectures on CEREC, magnification use, and other topics. He has lectured at many meetings and study clubs from Florida to Maine, and founded and produces the Techno-Ski seminars in New Hampshire. He can be reached at pcschoenbeck@yahoo.com or by visiting his Web site at northcountrydental.com.