Advancements in reconstructive dentistry utilizing adhesive bonding techniques and aesthetic materials have given the clinician a new perspective on the treatment options available to patients. Some clinicians, however, overlook patients who, due to economic and/or anatomical limitations, are not candidates for this type of dentistry. There are many clinical and financial situations where the removable prosthetic alternative is clearly the correct treatment choice.1
This is particularly true for the prospective implant patient. Although options for augmenting an existing ridge are available, many patients simply do not want to undergo the surgery necessary for implant placement (Figure 1). Many of these patients can be treated very predictably with options other than standard fixed prostheses. The ongoing trend in fixed prosthodontics has created a lull in removable prosthodontic training at a time when there has been less emphasis placed on removable prosthodontics in many dental schools.1 Less time devoted to removable prosthetics in dental school curricula and an increasing need for such services creates a perplexing dilemma.2 Clinicians who continue to hone their skills in removable prosthodontics can expect to provide these services to a multitude of patients and, when attentive to several basic principles, will experience increased referrals from these previously underserved individuals.
This article will discuss clinical indications for removable prosthetic treatment options as well as treatment principles, and illustrate the use of removable prosthodontic techniques in a case report.
PROSTHETIC ADJUSTMENTS AND ADAPTATION
 |
 |
|
Figure 1. Panoramic radiograph illustrating the presence of severe periodontal bone loss and the existence of a severely resorbed maxillary ridge. The sinus floor also precludes the possibility of any implant options without additional adjunctive surgery on the maxilla due to its close proximity. |
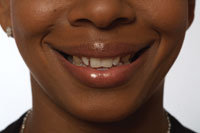
Figure 2. Before full-face photograph of full-mouth reconstruction case. |
 |
 |
|
Figure 3. Retracted “before” anterior view of combination full-mouth reconstruction case. |
Figure 4. Occlusal view of maxillary dentition before reconstruction. |
 |
 |
|
Figure 5. Retracted anterior view after maxillary fixed and removable prostheses have been completed with corresponding temporary overlays on mandibular teeth to final desired vertical dimension. |
Figure 6. Retracted anterior view of completed reconstruction. |
 |
 |
|
Figure 7. Occlusal view of completed maxillary combination case including full coverage porcelain and porcelain fused to gold crowns with provisions for a Vitallium 2000 (DENTSPLY Austenal) removable partial prosthesis designed into abutments. |
Figure 8. Full-face portrait of completed case with patient’s spouse who also had combination of fixed and removable prosthetic full-mouth reconstruction. |
Some practitioners avoid removable procedures because of the need to perform ongoing adjustments to the prosthesis. As with any treatment, however, adjustments must be performed in accordance with the dynamic structural change the body undergoes as it adapts to the aging and resorptive process. A properly designed, exquisitely constructed, and well-supported removable prosthesis can require as few adjustments as its fixed counterpart. Additionally, with careful planning and proper sequencing of treatment, a removable partial or full denture can be a very desirable aesthetic option (Figures 1 through 8).
Consideration of basic physiological principles in the design of the removable prosthesis ensures patient comfort and prevents the formation of destructive lateral forces that initiate the “domino effect” and the successive loss of abutment teeth.3 The destructive forces from improperly designed frameworks can often result in pathophysiologic resorption of the residual ridges.4
One of the primary components in the ideal adaptation of a removable prosthesis to the residual ridge is a mucosa-prosthesis interface that is fluid, or perhaps generated via a more fluid (as opposed to a static) impression. It is difficult to have a patient remain motionless during an impression for a removable prosthesis that will eventually rest upon fixed and/or potentially moving tissue. This is why a conventional alginate impression can, in many cases, create in-accuracies between mucosa and a stone model, particularly in nontooth borne Kennedy Class I and II type partial dentures with the addition of the saddles and denture teeth.5,6 The altered or split-cast technique for the development of removable partial dentures devised several years ago was originally designed to compensate for this dilemma.7 Various impression techniques have been devised over the years to address this inability to accurately obtain impressions of a moving object with a “hold still” type of impression.8
With the fully edentulous patient, the establishment of an ideal impression entails the use of a very slow-setting material (eg, Hydrocast, Sultan Dental; PermaSoft, DENTSPLY Austenal; Microseal, Amco International) that acts as both an impression material and a reline material. Over several days and appointments, pressure points and the vestibular borders are selectively cut back and rerelined as needed. Generally, the occlusion is evaluated during these “trial denture” (adjustment/impression/relining) appointments to ensure that any sore spots experienced by the patient are not attributed to an occlusal etiology. In the author’s opinion, sore spots related to occlusion on the vertical portions of the alveolus and mucosa are related to the lack of a balanced occlusal scheme. Hence, the occlusal adjustments are primarily performed on the cuspal inclines of the denture teeth, located as the patient performs lateral excursive movements. Tenderness found on more horizontal areas (eg, the crest of the ridge) is primarily caused by excessive forces on the occlusal stops of the denture teeth. These adjustments are directed more towards the cusp tips and corresponding fossae identified as the patient moves into maximum intercuspation.
For a comfortable yet functional prosthesis, common sense prevails regarding the need to establish an “average” position in space relative to the remaining supporting structures. With occlusal forces bearing down upon the fragile mucosa from rigid opponents, any excessive frictional movement will ultimately lead to the need for adjustments. The majority of these types of failures could be prevented by simply attending to proper impression protocol, and additionally the balancing of all occlusal forces to maximize their distribution across the entire surface area of the prosthesis. Confining the support of the occlusion onto an area of minimal mucosal movement, yet allowing for extension of the prosthesis into areas that will tolerate its presence, is key to constructing the successful partial and full denture.
 |
 |
|
Figure 9. Metal-free acrylic partial denture immediately placed after extraction (DENTSPLY Thermoflex [Lucitone Flexible Resin System]). |
Figure 10. Metal-free acrylic unilateral partial denture out of mouth. |
In addition to the construction of a prosthesis with balanced occlusion, for selected cases the use of more aesthetic, and sometimes patient-preferred options, should be considered, including the newer acetyl materials (eg, Thermoflex, DENTSPLY Austenal). These materials possess the unique ability to flex yet are strong enough to be utilized as frameworks in the construction of removable partial dentures. Such polymers offer additional nonmetallic choices to the dental profession, and can be occasionally used as major connectors for interim unilateral cases where either implants or other fixed prosthetic choices are to be postponed (Figures 9 and 10).
PATIENT EXPECTATIONS AND OCCLUSION CONSIDERATIONS
Along with proper design and impression techniques, clinicians should educate patients concerning the limitations of their prosthesis and what can be expected.9 While some movement of the removable prosthesis may actually be desirable, a balance must exist. One predictable impression technique that establishes uniform tissue support employs the various procedures developed by Pound and expounded by Turbyfill.10 The basis for determining the most ideal occlusal schemes for removable prosthetics borrows several of the accepted ideologies and procedures commonly used to stabilize and restore natural dentition. In partially edentulous cases, it is advisable to minimize any deleterious forces from the indirect retainers on the abutment teeth.11 With fully edentulous cases, the lingualized occlusion recommended by Turbyfill10 seems to provide the most successful results. Lingualized occlusion involves the use of more highly angled or ‘sharper’ denture teeth on the maxillary denture, against lower angled or more shallow anatomy on the mandibular denture. This simulates a “mortar-pestle” action that aids chewing efficiency, yet can potentially minimize the lateral forces that can not only dislodge the dentures, but also create more sore spots.
Secondarily, a harmony is needed between the movement from occlusal forces and the prevention of excessive wear to the abutment teeth. No prosthetic restoration performs as well as one’s own natural dentition. However, with a well-balanced occlusion, uniform tissue support designed to adapt to a constantly dynamic tissue surface interface, and patient instruction to assist them in adapting to this less-than-ideal replacement, the removable prosthesis can be a rewarding service.
CASE REPORT
 |
 |
|
Figure 11. Panoramic radiograph of sample case illustrating severely resorbed maxillary alveolus and the inability to utilize implant replacements without significant sinus grafting. |
Figure 12. Occlusal view of Empress (Ivoclar Vivadent) porcelain onlay abutment restorations on lab model illustrating rest seats, ledges, and guide planes for clasping for maxillary removable partial denture. |
 |
 |
|
Figure 13. Tissue side of removable prosthesis with Hydrocaste (Sultan Dental) reline material used as functionally generated impression. |
Figure 14. Preliminary polymerization of Triad Gel intraorally with patient in maximum intercuspation to establish initial occlusal relationship. |
 |
 |
|
Figure 15. Occlusal view of preliminary polymerization of Triad on saddles of partial prosthesis, immediately after removal from the mouth. NOTE: Areas of desired occlusal stops on saddle areas marked with Sharpie. |
Figure 16. Occlusal view of maxillary prosthesis with saddle areas and excess Triad Gel removed to a completely flat occlusal plane. NOTE: Areas of desired occlusal stops have not been removed by flattening out excess Triad Gel. |
A 61-year-old female presented for replacement of her missing dentition, which had been lost years previously due to periodontal disease and severe caries. Clinical and radiographic evaluation revealed partial maxillary edentulism, with the remaining dentition in a salvageable state.
The patient had previously avoided replacements of her missing maxillary molars because of her fear of the failure of a removable prosthesis. Upon discussion with the patient, it was determined that due to her desire to not have any additional surgical intervention, implant placement and the involved grafting procedures would not be acceptable as a treatment option (Figure 11). However, additional occlusal support was necessary to prevent secondary occlusal trauma to her remaining dentition. Hence, a maxillary removable partial denture was presented. It was important to the patient that metal not be visible in the seated prosthesis; from the clinician’s perspective it would be necessary to restore the abutment teeth with aesthetic materials that would be durable enough to resist wear from the rest seats and clasping, yet be properly contoured and durable enough to provide the aesthetics and space necessary to hide the indirect retainers.
Treatment was initiated accordingly with the delivery of ceramic onlays (IPS Empress, Ivoclar Vivadent) and a single crown with rest seats and guide planes designed to accommodate clasping that would satisfy all the requirements necessary to stabilize the abutment teeth, yet provide adequate retention for the prosthesis (Figure 12).
Preliminary alginate impressions (Accudent, Ivoclar Vivadent) of both arches were obtained and a bite relationship was taken. A relieved framework was then constructed with acrylic base-plates in the saddle areas instead of actual denture teeth. This gave the clinician the ability to place impression material in the edentulous saddle areas under the flanges to accurately capture the mucosal areas over a period of several days and during function. The preliminary reline impression was established by the clinician, who firmly held the framework against the abutment teeth while preventing the patient from occluding on the acrylic bite rims (Figure 13).
The next phase of construction involved the design of the occlusion on the bite rims. By constructing the acrylic saddle areas on the occlusal side slightly out of occlusion (versus using denture teeth), the mandible was able to find the least resistance to full closure, allowing for a more reproducible bite relationship after several days of wearing the prosthesis with a flattened occlusal surface. When the denture teeth were later placed in the edentulous areas, after the patient had initially worn the prosthesis with single-point contacts, a more comfortable mandibular to maxillary relationship was assured, rather than one guided solely by the prosthesis.
Triad VLC Bonding Agent and then Triad Gel (DENTSPLY) were placed onto the occlusal areas of the saddles. The opposing dentition was lubricated with a silicone-based material, and then the Triad material was preliminarily cured intraorally (Figure 14). This established single-point contacts between the existing natural dentition and the saddle areas to help direct the forces of the antagonists to the crest of the residual ridge, which tends to be the most advantageous place to direct the forces of occlusion (Figure 15).12
 |
 |
|
Figure 17. Final bite registration obtained after several days with Hydrocaste reline on mucosal side of prosthesis, and Triad Gel relined occlusal surface with occlusal stops refined prior to final bite registration. |
Figure 18. Anterior view of final maxillary removable partial denture with DENTSPLY Trubyte IPN teeth processed into saddle areas. |
 |
 |
|
Figure 19. Tissue side of functionally generated Hydrocaste reline/impression for complete denture ready for processing. |
Figure 20. Occlusal view of trial denture ready for final processing. |
Final curing was performed in the Triad Curing Unit. The occlusal surfaces of the saddles were then marked in the most desirable position, and the entire surface was subsequently smoothed flat, without the removal of the marked occlusal stops. This was inserted intraorally and rechecked with articulating paper (Figure 16). Once the patient was comfortable in the saddle areas (after several days) and felt equal bilateral force on her prosthesis, additional time was spent with articulating paper to refine the final occlusal relationship. Once all mucosal areas were comfortable, accurately impressed, and all desired occlusal areas were ideal, a check bite was obtained (Figure 17).
Subsequently, the prosthesis—with the impressed and relined mucosal areas and the flattened, relined occlusal areas—was removed from the patient’s mouth and used in the fabrication of the definitive prosthesis. At the insert of the final denture, the occlusion was again checked for equal bilateral contacts—this time on the denture teeth, which had been processed into the flanges. The mucosal-saddle areas were also checked with a pressure indicating spray for adequate and equally displaced tissue contact. Generally, at this appointment, very little needs to be done to complete the treatment (Figure 18).
CONCLUSION
Given the use of a proven, functionally generated impression technique, extremely accurate and comfortable removable full and partial denture situations can be constructed with ease (Figures 19 and 20). While a detailed discussion of occlusion is beyond the scope of this article, if the same or similar guidelines for occlusion that are utilized for natural teeth are applied to the partial removable prosthesis, successful treatment is attainable. For fully edentulous cases, the only additional requirement for success is providing a fully bilaterally balanced lingualized occlusal relationship. Patience to achieve the desired final outcome is also paramount, along with the proper management of the patient. These are the tools that will help the treating dentist achieve predictable success, and provide the most comfortable and functional removable prosthetic alternative possible to an ever-expanding patient base.
References
- Krul AJ, Jacobson TE, Finzen FC. Removable Partial Denture Design: Outline Syllabus. 4th ed. San Rafael, CA: Indent Publishing; 1990:preface.
- Peterson PG. Will America Grow Up Before It Grows Old? How the Coming Social Security Crisis Threatens You, Your Family, and Your Country. New York: Random House; 1996.
- Maxfield JB, Nicholls JI, Smith DE. The measurement of forces transmitted to abutment teeth of removable partial dentures. J Prosthet Dent. 1979;41:134-142.
- Nishimura I, Szabo G, Flynn E, et al. A local pathophysiological mechanism of the resorption of residual ridges: prostaglandin as a mediator of bone resorption. J Prosthet Dent. 1988;60:381-388.
- Kramer HM. Impression technique for removable partial dentures. J Prosthet Dent. 1961;11:84-92.
- Leupold RJ. A comparative study of impression procedures for distal extension removable partial dentures. J Prosthet Dent. 1966;16:708-720.
- Leupold RJ, Kratochvil FJ. An altered-cast procedure to improve tissue support for removable partial dentures. J Prosthet Dent. 1965;15:672-678.
- Seely PW, Windeler SE, Norling BK. An investigation of shear bond strengths of various resin-bonded inner surface rest seat designs for removable partial dentures. J Prosthet Dent. 1987;58:186-194.
- Jacobson TE. Educating denture patients. J Calif Dent Assoc. 1982;10:81-83.
- Turbyfill WF. Impression techniques for removable partial dentures. Gen Dent. 2001;49:358-364.
- Cecconi BT, Asgar K, Dootz E. The effect of partial denture clasp design on abutment tooth movement. J Prosthet Dent. 1971;25:44-56.
- Kydd WL, Daly CH. The biologic and mechanical effects of stress on oral mucosa. J Prosthet Dent. 1982;47:317-329.
Dr. Voller maintains a private practice in Kittanning, Pa, that focuses on aesthetic and reconstructive dentistry and orthodontics. He is a clinical instructor in dental digital photography and on the advisory board of directors of The Academy of Comprehensive Esthetics. He lectures nationally and has published several articles on full-mouth reconstruction and aesthetic dentistry. He can be reached at (724) 543-4948 and (724) 664-5960, or at drvoller@alltel.net, or visit his Web site at vollersmiles.com.