Excessive gingival display can affect the total aesthetics of a smile, becoming its focus instead of its frame. This can be the result of passive eruption of the gingival complex as the teeth erupt.1,2 The condition of delayed or altered passive eruption exists when the gingival complex remains coronal to the cementoenamel junction (CEJ), with the attachment on the enamel instead of the cementum of the root, giving the appearance of short clinical crowns.3
Crown lengthening4 is critical to the success of creating a smile that is harmoniously balanced with its surrounding facial features.5 Patients who clinically display too much gingival tissue and short teeth (“gummy” smile) require a thorough diagnosis and treatment planning to provide predictable aesthetic outcomes.6 If a patient has altered passive eruption (APE) of the maxillary anterior teeth (either secondary to orthodontic treatment or without orthodontic therapy) and the patient has completed facial growth,7 then the surgeon must first correct the gingival levels with either a gingivectomy or aesthetic crown lengthening procedure. This must be done before the placement of veneers or crowns while ensuring that the eventual gingival margins of the maxillary anterior teeth will be at their correct level relative to the adjacent anterior teeth.8
OSSEOUS STRUCTURE CONSIDERATIONS
In the absence of periodontal disease, the osseous structure roughly follows the scalloped parabolic contour of the CEJ from facial to interproximal at an average distance of 2 to 3 mm.9 In addition, the average interproximal bone height is 3 mm coronal to the facial crest of bone (COB).10 Since the soft-tissue topography is usually determined by the underlying hard tissue, this osseous “scallop” usually results in a gingival scallop of 3 mm.11 Examination of periapical radiographs or periodontal vertical bite-wings will allow the clinician to ascertain the position of the alveolar bone relative to the CEJ to determine whether the COB is 2 to 3 mm apical to the CEJ, thereby allowing for the biologic width.12 However, in a clinical situation where the COB is coronal to the CEJ, the condition results in altered passive eruption (APE).13 In this situation, the gingival margin is usually located 3 mm (on average) coronal to the level of the COB, and, being more coronal on the body of the tooth, creates the appearance of a short clinical crown.14
These visual findings are coupled with the clinical information obtained by bone sounding. Bone sounding involves using a periodontal probe to locate the CEJ to determine whether it can be felt within the gingival sulcus or only when the probe penetrates through the base of the sulcus.15 The periodontal probe is also used to feel for the COB. This value is expressed as a numeric distance in millimeters, thus revealing the distance between the COB and CEJ. This is to ascertain whether there is sufficient biologic width.16 Normally the COB is 2 to 3 mm apical to the CEJ in a healthy human periodontium.17
SOFT- AND HARD-TISSUE CONSIDERATIONS
In addition to the gingival margin on the facial aspect of the teeth, in a healthy dentition without any bone loss the interproximal papilla between teeth is approximately 4.5 mm coronal to the interproximal crest of bone. The mid direct facial is about 1.5 mm more coronal to the COB. This additional 1.5 mm, with the 3-mm average osseous scallop from the CEJ, results in the tip of the papilla being an average of 4.5 mm coronal to the facial free gingival margin, where there is a “normal” periodontium without loss of bone or periodontal attachment due to periodontal disease.18
Anatomic considerations act as parameters when practitioners perform aesthetic gingival recontouring. A useful guide can be fabricated by modifying the mounted diagnostic casts so that the waxed modification reflects the ideal tooth proportions desired in the final result based on the guidelines previously published by Chiche and Pinault.19 These guidelines suggest that the average length for aesthetically pleasing maxillary central incisors is 10 to 12 mm.20 They, along with the recommended width-to-length ratio of 75% to 80%,21 should be kept in mind when recontouring the gingival tissues so the teeth are not left too long or too short.22
After the desired proportions are achieved on the central incisors, practitioners should then focus on the height of contour of the gingival margin on the lateral incisors (zenith).23 The proper placement of the gingival zenith should be at the peak of the parabolic curvature of the gingival margin. For the central incisors, cuspids, and bicuspids, this should be specifically located slightly distal to the middle of the long axis on these teeth. This gives the centrals, cuspids, and bicuspids the subtle distal root inclination, which is paramount for the scaffold of a beautiful smile. The zenith for the lateral incisors is located at the mid-line of the long axis of the tooth. Furthermore, the gingival crest height for the lateral incisors should be 1 mm shorter than the gingival margins of the adjacent teeth. Additionally, the gingival tissues should have a knife-edge gingival margin.24
When the presence of short clinical crowns and crestal bone levels approximating the CEJ have been determined, a diagnosis of APE can be made through the maxillary arch. The practitioner can then fabricate an aesthetic guide, which can be placed over the patient’s existing teeth, allowing both the practitioner and patient to visualize what the smile would look like with the gingiva in the modified aesthetic position.25
The central incisors should demonstrate midline symmetry as well as the correct 75% to 80% width-to-length ratio. In addition, the incisal smile line follows the curvature of the lower lip.26 The newly established soft-tissue smile line should show a reduction of the “gummy” smile and be aesthetically appealing and harmonious with surrounding facial features.27
Gingival levels should be assessed relative to the projected incisal edge position. A predictable method of determining the proper gingival positions is to determine the desired tooth size relative to the projected incisal edge position. The practitioner should remember that the incisal edge should not be positioned using the relative position of the gingival margin to create the proper tooth size. This is because the gingival margin can move with eruption or recession.28 It is also critical, when establishing the proper position of the maxillary anterior teeth for an optimal cosmetic outcome, to assess the levels of the in-terdental papillary tissues and their position relative to crown length of the maxillary incisors.
GINGIVECTOMY/GINGIVOPLASTY: CORRECTION OF SOFT TISSUE
Traditionally, scalpels and periodontal knives (Orban and Kirkland) were utilized to sculpt soft tissue when gingivectomy was indicated to improve aesthetics.5 These provided precise incisions, but resulted in raw, bleeding surfaces and a more difficult postoperative healing. Another option, monopolar electrosurgery, requires a dry field during treatment. This may increase tissue inflammation during the initial healing stage with subsequent tissue shrinkage. “Charring” of the tissue margins at the surgery site has also been reported with monopolar electrosurgery and from operating in a dry field.29,30 Bipolar electrosurgery was developed to overcome these obstacles associated with monopolar electrosurgery.
True bipolar electrosurgery, as currently used in dentistry, is a crossover from neurosurgery, where delicate incisions are required in wet fields with no lateral heat generation. The Bident Bipolar surgical unit (Synergetics) transfers those neurosurgical requirements to the dental environment, allowing intraoral soft-tissue surgery in wet fields with char-free, nonbleeding incision margins.31 This eliminates marginal shrinkage related to tissue inflammation and provides more comfortable postoperative healing for the patient.
When using the bipolar surgical unit, since the tips have 2 electrodes that are either straight wires or loops, one must remember that the first electrode to touch the tissue acts as the return and the second electrode cuts/coagulates depending on which foot pedal is depressed. Since the bipolar surgical unit is fully isolated from ground (unlike monopolar electrosurgical units), a ground is not required. The author (Kurtzman) recommends the use of constant irrigation while operating with the Bident Bipolar surgical unit to maintain tissue hydration and eliminate tissue charring during treatment. It also reduces postoperative inflammation and improves efficiency with the handpiece. Coagulation occurs during cutting so that there is no oozing from the wound edges to interfere with any restorative procedures being performed at the same appointment.32
CASE REPORT
 |
 |
| Figure 1. Preoperative smile demonstrating passive eruption and an uneven display of gingiva on the maxillary anterior. | Figure 2. Passive eruption of the maxillary anteriors and premolars, with a wide band of attached gingiva present. |
 |
 |
| Figure 3. Master model showing ideal placement of the gingival margin based on proper width-to-length ratio outlined on the cast. |
Figure 4. Vacuform surgical stent on the master model trimmed to desired gingival margin location and outlined in black for easy identification intraorally. |
 |
 |
|
Figure 5. Surgical stent is placed intraorally to show where gingival margins will be in relation to the upper lips at maximum smile. |
Figure 6. Surgical stent intraorally showing where the gingival margins will be in relation to the mucogingival junction. |
 |
|
Figure 7. A Bident Bipolar electrosurgical handpiece is utilized to connect the marks made with the stent, exposing the cervical coronal tooth structure. (This image is a video screen-capture.) |
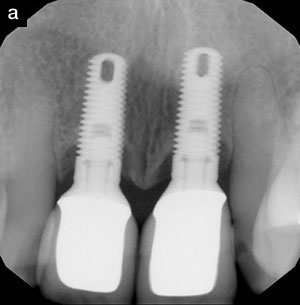
A female patient presented with a complaint that her teeth appeared too short and her smile was “gummy” (Figure 1). Diagnosis determined that the patient had good periodontal health with no gingival inflammation or bleeding. She had a wide band of attached gingiva (Figure 2). Probing depth in the maxillary anterior was within normal limits with depths of 1 to 2 mm. The gingival margin was, in general, 2 mm coronal to the CEJ. Radiographically, the osseous crest was apical to the CEJ, and no bone loss was evident.
Upper and lower impressions were taken with alginate, and study models were fabricated. Using a width to length ratio of 75%, a pencil mark was made on the cast indicating the ideal gingival margin placement (Figure 3). A vacuform stent was fabricated using a sheet of 0.020-inch Tray-Rite (DENTSPLY Raintree Essix). The tray was then trimmed to place the facial edge at the desired gingival margin. A black Sharpie pen was used to color the facial edge of the material to improve visibility intraorally during surgery (Figure 4).
The surgical stent was tried in and the position of the new gingival margin was checked for aesthetic positioning in relation to the patient’s upper lip when smiling (Figures 5 and 6). This should be done prior to application of local anesthetic to see the normal lip position. Alterations can then be made to the stent prior to initiation of the surgical aspect of the gingival correction.
Local anesthetic was infiltrated into the buccal vestibule from the maxillary second premolar to maxillary second premolar. A periodontal probe was introduced into the facial sulcus to sound the osseous crest in relation to the CEJ; no bone was noted coronal to the CEJ on the teeth. The surgical stent was inserted, and a Bident Bipolar 3303 (Synergetics) gingivectomy handpiece was utilized to mark the zenith of each tooth to be altered. The stent was removed, and, using the gingivectomy handpiece, the gingival margin was sculpted to ideal contours (Figure 7). The papilla is spared to avoid the potential of creating interproximal black triangles.
 |
 |
| Figure 8. A Bident Bipolar “fishhook” handpiece is utilized under irrigation to feather the new gingival margins, providing normal contours. (This image is a video screen-capture.) | Figure 9. Immediately following gingivectomy utilizing the Bident Bipolar surgical system. Although the tissue is red, note a lack of tissue hemorrhage. |
 |
 |
| Figure 10. Two-week post-surgical treatment. Note lack of tissue inflammation. | Figure 11. Four-week post-surgical treatment. Note lack of inflammation and an improved aesthetic result. |
The resulting tissue margin after use of the gingivectomy handpiece results in a soft-tissue ledge, which needs to be tapered onto the tooth. A Bident Bipolar 3302 (Synergetics) gingivoplasty handpiece, also referred to as a “fishhook,” is used to taper the gingival margin to create a natural knife-edge (Figure 8). As the papilla following the gingivectomy is often bulky facially, the facial aspect of the papilla is planed back to de-bulk the papilla with the fishhook. Although the altered margins appeared red, due to the coagulation abilities of the Bident Bipolar unit, no active bleeding was noted (Figure 9).
The patient was dismissed and instructed to avoid any mouthrinses containing alcohol or peroxide for the first week and to rinse with warm salt water 3 to 4 times daily for the first 3 days. Additionally, the patient was instructed to continue oral hygiene, including brushing the area with a toothbrush and her normal toothpaste. At 24 hours the patient was called to check on her comfort level; she indicated neither postoperative discomfort nor irritation during normal daily activities.
The patient returned for a postoperative examination 2 weeks later. No inflammation was noted (Figure 10). A 4-week postoperative examination demonstrated a more aesthetic smile with improved width-to-length proportions and the elimination of excess gingival display (Figure 11).
CONCLUSION
When patients have a desire to improve the aesthetics of their smiles, one should evaluate the gingival “frame” as well as the teeth when determining the best treatment plan to achieve their goals. Preplanning the desired position of the gingival margin extraorally will simplify the procedure and ensure that the patient’s expectations are met. The proper use of the Bident Bipolar surgical system produces a noncharred, nonoozing gingival margin immediately following surgery with a lack of postoperative inflammation.
REFERENCES
- Moshrefi A. Altered passive eruption. J West Soc Periodontol Periodontal Abstr. 2000;48:5-8.
- Dolt AH III, Robbins JW. Altered passive eruption: an etiology of short clinical crowns. Quintessence Int. 1997;28:363-372.
- Weinberg MA, Eskow RN. An overview of delayed passive eruption. Compend Contin Educ Dent. 2000;21:511-522.
- Kois JC. Altering gingival levels: the restorative connection part 1: biologic variables. J Esthet Dent. 1994;6:3-9.
- Glassman S. Cosmetic treatment of the gummy smile. Contemp Esthet Restor Pract. 2001;5:58-61.
- Rufenacht CR. Fundamentals of Esthetics. Carol Stream, IL: Quintessence Publishing; 1990.
- Silverstein LH, Shatz PC, Baker K. Subgingival technology to enhance the therapeutic outcome during surgical and restorative phases of smile reconstruction. Contemp Esthet Restor Pract. July, pp 40-47, 2002.
- Levine RA, Randel H. Multidisciplinary approach to solving cosmetic dilemmas in the esthetic zone. Contemp Esthet Restor Pract. 2001;5:62-67.
- Kokich VG. Esthetics and anterior tooth position: an orthodontic perspective, part III: mediolateral relationships. J Esthet Dent. 1993;5:200-207.
- Rufenacht C. Structural esthetic rules. In: Fundamentals of Esthetics. Chicago, IL: Quintessence Publishing; 1992:67-132.
- Carranza FA, Newman MG, Glickman I. Clinical Periodontology. 8th ed. Philadelphia, PA: WB Saunders; 1996:720-722.
- Kois JC. The restorative-periodontal interface: biological parameters. Periodontol 2000. 1996;11:29-38.
- Goldstein RE. Esthetics in Dentistry. Philadel-phia, PA: Lippincott; 1976:425-455.
- Smukler H, Chaibi M. Periodontal and dental considerations in clinical crown extension: a rational basis for treatment. Int J Periodontics Restorative Dent. 1997;17:464-477.
- Hirschfeld I. A study of skulls in the American Museum of Natural History in relation to periodontal disease. J Dent Res. 1923;5:241-265.
- Weinman JP, Sicher H. Bone and Bones: Fundamentals of Bone Biology. 2nd ed. St Louis, MO: Mosby; 1955.
- Hermann JS, Cochran DL, Nummikoski PV, et al. Crestal bone changes around titanium implants. A radiographic evaluation of unloaded nonsubmerged and submerged implants in the canine mandible. J Periodontol. 1997;68:1117-1130.
- Saadoun AP, Le Gall MG, Touti B. Current trends in implantology: part II – treatment planning, aesthetic considerations, and tissue regeneration. Pract Proced Aesthet Dent. 2004;16:707-714.
- Rosenberg ES, Cho SC, Garber DA. Crown lengthening revisited. Compend Contin Educ Dent. 1999;20:527-538.
- Garnick JJ, Silverstein LH. Periodontal probing: what does it mean? In: Clark’s Clinical Dentistry. Vol 3. Philadelphia, PA: Lippincott; 1997:1-15.
- Ten Cate AR. The development of the periodontium. In: Melcher AH, Bowen WH, eds. Biology of the Periodontium. New York, NY: Academic Press; 1969.
- Spear FM. The esthetic management of multiple missing anterior teeth. Inside Dentistry. January 2007;72-76.
- Kokich VG, Kokich VO. Interrelationship of orthodontics with periodontics and restorative dentistry. In: Nanda R, ed. Biomechanics and Esthetic Strategies in Clinical Orthodontics. St Louis, MO: Saunders; 2005:348-373.
- Silverstein LH, Garnick JJ, Szikman M, et al. Medication-induced gingival enlargement: a clinical review. Gen Dent. 1997;45:371-378.
- Silverstein LH, Koch JP, Lefkove MD, et al. Nifedipine-induced gingival enlargement around dental implants: a clinical report. J Oral Implantol. 1995;21:116-120.
- Sterrett JD, Oliver T, Robinson F, et al. Width/length ratios of normal clinical crowns of the maxillary anterior dentition in man. J Clin Periodontol. 1999;26:153-157.
- Spear FM, Kokich VG, Mathews DP. Interdisciplinary management of anterior dental esthetics. J Am Dent Assoc. 2006;137:160-169.
- Ahmad I. Geometric considerations in anterior dental aesthetics: restorative principles. Pract Periodontics Aesthet Dent. 1998;10:813-822.
- Livaditis GJ. Comparison of monopolar and bipolar electrosurgical modes for restorative dentistry: a review of the literature. J Prosthet Dent. 2001;86:390-399.
- Malis LI. Electrosurgery and bipolar technology. Neurosurgery. 2006;58(1 suppl):1-12.
- Malis LI. Atraumatic bloodless removal of intramedullary hemangioblastomas of the spinal cord. J Neurosurg. 2002;97(1 suppl):1-6.
- Tucker RD, Hollenhorst MJ. Bipolar electrosurgical devices. Endosc Surg Allied Technol. 1993;1:110-113.
Dr. Kurtzman is in private practice in Silver Spring, Md, and is an assistant clinical professor at the University of Maryland, School of Dentistry, Department of Restorative Dentistry. He is on the editorial board of the Journal of Oral Implantology, an assistant editor of the International Magazine of Oral Implantology, and editor of the Maryland Academy of General Dentistry. He has earned Fellowships in the AGD, the International Congress of Oral Implantologists, the Pierre Fauchard Academy, and American College of Dentists, and Masterships in the AGD and the Implant Prosthetic Section of the International Congress of Oral Implantologists. He has earned Diplomat status in the International Congress of Oral Implantologists. Dr. Kurtzman can be contacted at dr_kurtzman@maryland-implants.com.
Dr. Silverstein is an associate clinical professor of periodontics at the Medical College of Georgia in Augusta. He has lectured internationally on the topics of periodontics and dental implantology and has contributed extensively to the literature available on these topics. He is on the editorial boards of Practical Periodontics and Aesthetic Dentistry, Dentistry Today, and Esthetique, a direct-to-consumer aesthetic topics publication. He also maintains a private practice limited to periodontal care and dental implants in Atlanta at Kennestone Periodontics, PC. He recently became the chairman of the Interactive Distant Learning Center, an affiliate of the Medical College of Georgia located in Marietta at Kennestone Periodontics, PC. He has recently published his first textbook, Principles of Dental Suturing: A Complete Guide to Surgical Closure, which is credentialed by the AGD. Dr. Silverstein can be reached at (770) 952-5432 or kenperio@mindspring.com.