Aesthetic, full-coverage fixed partial dentures have remained a difficult challenge for dentists. Traditional porcelain-fused-to-metal (PFM) fixed partial denture restorations have provided predictable strength and durability. However, their aesthetics have been compromised by the underlying metal framework. Light transmission is impeded by the metal substructure, leading to dark margins, a shadow effect at the tissue, and opaquer show-through.1
Metal-free systems have been developed with the necessary strength and durability for fixed partial dentures.2,3 However, these high-strength ceramic systems require large connectors for fixed partial dentures, making them appear bulky in the anterior. Also, such systems have opaque ceramic cores that make color matching difficult with other restorations.
A third option for anterior fixed partial dentures is a pressed ceramic-to-metal with an extensive metal cutback.4-6 Pressed dental ceramics have undergone vast improvement during the last 10 years. These materials can now be used either alone for anterior veneers and crowns or in conjunction with metals for increased strength. The ability to press a ceramic to metal allows a critical advantage when metal-free and metal-supported restorations need to be color-matched. The traditional shadow and dark margins of porcelain-fused-to-metal restorations can be overcome with an aggressive metal cutback. The lingual of the restoration can be ceramic pressed to metal while the facial is all-ceramic. The facial can be all-ceramic, allowing easy color matching to all-ceramic crowns or veneers. Such a technique is ideal for fabricating strong, aesthetic fixed partial dentures.
CASE PRESENTATION
 |
 |
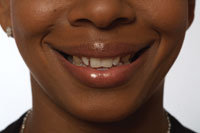
| Figure 1. The patient was unhappy with the display of metal margins, shade, and diastemas. | Figure 2. Retracted view showing preoperative condition of teeth. |
A 40-year-old male presented for replacement of an anterior fixed partial denture (Figures 1 and 2). The patient had a PFM fixed partial denture covering teeth Nos. 9 to 11. The patient had been unhappy with the color and dark metal margins of the preexisting full-coverage PFM fixed partial denture.
Clinical Exam
Clinical examination revealed the existence of a porcelain-fused-to-metal fixed partial denture. There were also small diastemas between the anterior teeth on the right side. The periodontal health was good. Examination also revealed no sensitivity to palpation and no history of temporomandibular joint symptoms. The remaining dentition was noncontributory.
Diagnosis
The patient’s goal was to have a new partial denture that would contribute to a nice smile. The patient was open to additional treatment in order to improve his smile. The goals for improving the patient’s smile were the following:
(1) eliminate shadow effect and dark margins of partial denture;
(2) color matching of anterior teeth; and
(3) shape symmetry of anterior teeth.
Treatment Plan
Restorative options were discussed with the patient, and a treatment plan was subsequently developed. To achieve the patient’s goals, a ceramic-pressed-to-metal partial denture with metal only on the lingual would be fabricated. Seven additional porcelain veneers were recommended to close the anterior diastemas and improve the buccal corridor proportions.
Procedure
A photographic record was captured, and preliminary study models were taken in order to determine the aesthetics, occlusion, and amount of preparation required. A diagnostic wax-up was created to evaluate occlusion and aesthetics, to be a template for provisional fabrication, and to assist in communication with the patient and laboratory technician.
 |
| Figure 3. Preparations for 3 porcelain veneers and a fixed bridge. Note ovate pontic. |
For tooth preparation, the old fixed partial denture was removed and the preparations were refined. Teeth Nos. 6, 7, and 8 were prepared for porcelain veneers. Slightly subgingival chamfer margins were utilized to allow adequate porcelain thickness for strength and color masking. Gingival margins were smoothened with a fine end-cutting diamond bur. All sharp edges were rounded and refined with a fine diamond bur. A diode laser was used to shape an ovate pontic site. This presents the illusion that the pontic is emerging from the tissue as would a natural tooth, with at least 1 mm of soft tissue remaining above the osseous crest (Figure 3).
Final impressions were made using a polyvinyl siloxane (PVS) material. A preoperative model, bite registration, color mapping, desired teeth length and shape, type of porcelain to be used, photos, and stump shades were also sent to the laboratory.
Provisionalization
 |
| Figure 4. The provisional restorations were fabricated from a template of the wax-up to give the patient a preview of the final results. |
To fabricate provisional restorations, an impression of the diagnostic wax-up was utilized as a template. After preparation, the template was filled with a bis-acrylic composite provisional material (Integrity, DENTSPLY) and placed over the prepared teeth. After the initial setting of the provisional material, the provisional restorations were removed and the excess was trimmed and polished. The provisional was cemented with a resin-based provisional cement (Proviolink, Ivoclar, Figure 4).
The patient was seen for a 1-week follow-up to evaluate the aesthetics and occlusion of the provisional restorations.
Restoration Fabrication
Authentic (Microstar) is a type of low-fusing, leucite-reinforced pressable ceramic that allows both a staining technique as well as a layering technique, or a combination of both. It can also be pressed to metal.7
 |
 |
| Figure 5. Metal coping for fixed partial denture did not extend to facial surfaces. | Figure 6. Holes were placed on the lingual of the metal coping to allow for light transmission. |
 |
 |
| Figure 7. Facial view of pressed restorations. | Figure 8. Lingual view of pressed restorations. |
 |
| Figure 9. Internal view of final restoration showing metal coping design. |
A skeleton lingual frame-work for the fixed partial denture was fabricated to add support (Figures 5 and 6). Opaquer was applied to block the metal color. Then all restorations, fixed partial denture, and veneers were pressed to full contour with porcelain (Figures 7 and 8). The final partial denture consisted of a lingual framework with holes to allow for light transmission, covered by pressed ceramic (Figure 9).
Insertion
The provisional restoration was removed, and the teeth were cleaned with pumice and rotary brushes. The final restorations were tried in to assess fit. Once the fit was deemed satisfactory, the restorations were placed with try-in paste (Rely-X resin veneer cement, 3M ESPE) for patient approval prior to final cementation.
After patient approval, a slit rubber dam was placed for moisture control and increased visibility. The internal aspects of the restorations were etched with 37% phosphoric acid (Ultraetch, Ultradent) to remove debris from adjustment and try-in. The internal aspect of the restorations had been etched with 9.6% hydrofluoric acid by the laboratory technician. Silane (Silane, Ultradent) was applied for 1 minute and then air-dried. The restorations were then lightly coated with a low film thickness adhesive (Prime & Bond NT, DENTSPLY) and gently air-dried. Shade B.5 of a light-cured resin cement (Rely-X) was placed into the unit. The restorations were placed in a light-protective container. The teeth were cleaned with an antimicrobial solution (Consepsis, Ultradent) and then etched with 37% phosphoric acid (Ultra-etch). Multiple coats of a single-bottle adhesive (Prime & Bond NT) were applied and air-dried. The restorations were placed into position and spot-cured with a 2-mm light tip. After the restorations were spot-cured, the excess cement was removed using a rubber tip. A thin floss was gently used to remove interproximal excess cement. After all the excess cement had been removed, a thin coat of glycerin was then placed over all accessible margins. The restorations were fully light-cured from the facial and lingual aspects.
Remaining excess cement was removed with a No. 12 blade. Interproximal margins were smoothened with finishing strips (Epitex, GC). Composite veneers were placed on teeth Nos. 4, 5, 12, and 13 to improve buccal corridor proportions. Occlusion was checked and adjusted. The patient was scheduled for a follow-up appointment to evaluate aesthetics and occlusion.
 |
 |
| Figure 10. Full-smile view of final composite veneers, porcelain veneers, and fixed partial denture. | Figure 11. Retracted view of final restorations. |
 |
| Figure 12. Occlusal view showing full-coverage partial denture and veneers. |
The patient reported no sensitivity or complications at the follow-up appointment. Occlusion and gingival health were excellent. The patient was very happy with his new restorations (Figures 10 to 12).
References
1. Meyenberg KH, Imoberdorf MJ. The aesthetic challenges of single tooth replacement: a comparison of treatment alternatives. Pract Periodontics Aesthet Dent. 1997;9:727-735.
2. Fasbinder DJ. CAD/CAM ceramic restorations in the operatory and laboratory. Compend Contin Educ Dent. 2003;24:595-598,600-604.
3. Kugel G, Perry RD, Aboushala A. Restoring anterior maxillary dentition using alumina- and zirconia-based CAD/CAM restorations. Compend Contin Educ Dent. 2003;24(8):569-572,574,576.
4. Melkers MJ, Wohlberg JL. The combination of emerging technologies in aesthetic rehabilitation: Galvano Copings and pressed-to-metal ceramics. Pract Proced Aesthet Dent. 2003;15:247-251.
5. Touati B. The evolution of aesthetic restorative materials for inlays and onlays: a review. Pract Periodontics Aesthet Dent. 1996;8:657-666.
6. Helvey GA. Fabrication of aesthetic, pressed porcelain-fused-to-metal restorations. Pract Proced Aesthet Dent. 2002;14:487-492.
7. Chu SJ, Ahmad I. Light dynamic properties of a synthetic, low-fusing, quartz glass-ceramic material. Pract Proced Aesthet Dent. 2003;15:49-56.
Acknowledgment
The author would like to thank and acknowledge Frontier Dental Laboratory for fabricating the restorations presented in this article.
Dr. Javaheri maintains a private practice limited to aesthetic dentistry in Danville, Calif. He is the course director for the continuing education programs Setting New Standards in Cosmetic Dentistry and Smile Reconstruction at the University of the Pacific, San Francisco. He declares no financial interest in any of the products cited herein. He can be reached at drj@drjavaheri.com.