Today’s aesthetic dentistry can involve the selection of methods and materials that can be very overwhelming to the clinician. The dental profession is experiencing a large addition to the services it provides for patients. This change follows the introduction of root form endosseous implants that were introduced in the 1980s, and the aesthetic enhancements provided by the porcelain laminate veneers introduced in the 1990s. The use of CAD/CAM machines to fabricate high-strength ceramic cores for crowns and bridges promises to surpass the effects of the prior two revolutions.1
The switch to all-ceramic restorations and the use of CAD/CAM machines are being driven by a number of factors. The increasing demand for cosmetic procedures by today’s population will cause the demand for all-ceramic crowns and bridges to grow. This in turn will increase the demand for ceramic cores as a substitute for the metal frames used in traditional metal-ceramic crowns and bridges.2 Layering porcelain to nonmetallic cores is not new to dentistry, although certain materials lend themselves to this application better than others when attempting to adhere to sound dental principles and provide strength and exceptional aesthetics.
The challenge that the clinician and laboratory technician face with the advent of CAD/CAM-fabricated ceramic cores is finding a porcelain material that can reproduce the aesthetics found in the all-ceramic restorations without ceramic cores. Ceramic restorations from CAD/CAM machines tend to be very bright, white, high-value, opaque materials. The traditional method of layering porcelain tends to produce high-value and low-translucency restorations, which when placed adjacent to human dentition have a less-than-desirable outcome; the lack of translucency serves as the most important challenge of these new ceramic frameworks. The search for a porcelain substrate that will generate sound porcelain adherance and aesthetics has been the great quest of dental manufacturers.
This article will discuss a ceramic material manufactured for use with CAD/CAM frameworks. A case report using this material is included.
ALL-CERAMIC MATERIALS
Over the years several materials have been used for all-ceramic restorations; however, today only 2 types of ceramics are recommended for use with both anterior and posterior crowns and anterior bridges. These categories include the interpenetrating phase composites or glass-infiltrated ceramics, and the polycrystalline ceramics.3,4
Glass-infiltrated ceramics consist of a product formed by infiltrating molten glass into a partially sintered oxide material (aluminous oxide or alumina-zirconia oxide). Examples of this are InCeram Alumina and InCeram Zirconia (Vident).
Polycrystalline ceramics are materials with densely packed particles containing no glassy components. They cannot be processed to shapes without the use of computer-assisted machinery. Examples of this material include densely sintered, high-purity aluminum oxide, Procera AllCeram (Nobel Biocare), and the yttria tetragonal zirconia polycrystal (Y-TZP) systems. The majority of these systems use CAM of partially sintered Y-TZP blocks, followed by complete sintering of the shaped product for an additional 5 to 8 hours. These systems include Lava (3M ESPE), Cercon (DENTSPLY Ceramco), CEREC InLab (Sirona), and Procera All-Zirkon (Nobel Biocare). The partially sintered or “green state” material is milled to a size that is 20% to 25% larger than the final sintered core to compensate for the shrinkage that occurs during final sintering. As the fit of each final core is deemed to be acceptable, there is no standardization in fit and strength among different manufactured blocks of material because of the differences in the handling of the material by the various laboratories once it has been milled.5
A different system, DCS-Zirconium (DCS Popp Dental Laboratory) uses fully sintered Y-TZP blocks to mill fully sintered frames. No shrinkage is involved in the process when the fully sintered material is used, and the core made from totally industrially prepared material is structurally more reliable than the post-sintered green state material. There are questions that the CAD/CAM procedures may induce surface and subsurface flaws that may affects its physical properties.6 The use of ultrasonic machining promises to revolutionize the treatment of ceramic material in dentistry, as well as all phases of the industry. This technology greatly minimizes contact of the cutting tool with the material, which significantly reduces friction, heat, and the creation of surface flaws. Furthermore, the process increases the accuracy of the final milled product.7
The exceptional physical properties of these CAD/CAM ceramic cores have been described extensively in the literature and are not the focus of this article. This article focuses on the porcelain ceramic that will generate good to excellent aesthetics layered over the CAD/CAM alumina zirconia oxide (AL/ZR) core. The basic fundamental use and qualities for a particular type of porcelain, Initial Zr (GC America), is described.
Initial Zr is one of 6 Initial ceramics in an integrated product line (manufactured by GC Europe) with one color system, which can create metal-ceramic restorations as well as full-ceramic restorations. Each GC Initial ceramic is adapted to meet the needs of its particular fabrication process and frame-work, such as its coefficient of thermal expansion, therefore avoiding stress and fractures. This article focuses on GC Initial Zr, which is designed for layering over CAD/CAM frameworks. GC Initial Zr has an array of unique shades that have been developed for internal layering and external staining, high fluorescence, opalescence, and/or high translucency that allows for very favorable color matching with natural tooth structures.
For simple and promising handling of these high-strength ceramics, it is important for clinicians and lab technicians to consider a few fundamental points.
With zirconium oxide there are 2 variations:
• A white, more or less opaque, milled or sintered zirconium oxide.
• A dyed (in the corresponding shade) sintered zirconium oxide.
 |
 |
| Figure 1. Internal aspect of DCS Precifit Zirconium (DCS Popp Dental Laboratory) core with final layers of porcelain. Note the “white” opaque color of the fully sintered core as discussed in the article. |
Figure 2. DCS Precifit Zirconium oxide frame or copings ready for porcelain layering. |
The former lends itself better to higher-value restorations that are the norm of most patients requesting anterior restorations (Figure 1). The latter definitely offers a more compatible color base for the standard tooth shade buildup, especially for standard layering.8 When using the white zirconium oxide, Initial Zr porcelain lends itself very well to generating the desired aesthetic outcome. The white neutral base of the zirconium oxide allows the applied colors to appear very pure and genuine. The fluorescence missing from zirconium oxide cores or frames must be replaced with a thin coating of liner or frame modifiers to provide the natural fluorescence from inside the restoration. The liners/modifiers can also be individually tinted with the fluorescing Initial stains.9
When the clinician prescribes the shade A2, as was done in the case report described later in this article, the laboratory needs to adapt the base chroma in a different fashion than conventional porcelain layering. When making A2 shades, the base chroma should be at least the color effect of A3. With zirconium oxide frames it should be even a warmer tone because the dentin-colored frame material becomes lighter with each firing. The result is that layered restorations without intensified chroma appear too light in the patient’s mouth.9
A similar appearance is seen with the white, non-chroma-intensified zirconium oxide restorations. The missing chroma and fluorescence on the frame causes a light, too white/gray appearance. The Initial Zr layering system compensates for this unwelcome addition and standardizes the layering procedure for the laboratory technician.10
It is not as simple to evaluate the optimal firing of AL/ZR ceramic. Improper firing causes the incorrect shade seen frequently in AL/ZR restorations. Most furnaces fire 20° to 30°C lower, especially in the temperature firing range of zirconium ceramics. All such ceramics, but particularly AL/ZR, react to low firing temperatures with slightly limited transparency and color effects. On the other hand, somewhat higher firing cycles cause no problems and actually support the color and transparency effects. The ceramic firing stability is unusually good, so that in most furnaces raising the end temperature by 10° to 30°C is recommended in order to achieve the best outcome.10
Incorrectly constructed or layered frames are another reason for aesthetic failures when using white zirconium oxide restorations. In general, the frames should be the same size as the circumference of all the frames and built with light material zirconium oxide. If the frames are of different sizes, then the circumferences of the smaller frames will differ in color, and will appear either gray or too dark and intense in color11 (Figure 2).
When using these AL/ZR frames one must be aware of the aesthetic limits of the material. This material is very difficult to control aesthetically for inlay, onlay, and veneer restorations due to the very white-colored margins. This restorative method lends itself to full-coverage restorations due to the preparation of the tooth structure with circumferential shoulder preparations. The aesthetic effect necessary in veneer, inlay, or onlay restorations is not generally achieved due to the opacious zirconium oxide material blocking light in the enamel of natural teeth, resulting in a color impact along the margin. Therefore, any preparation of the teeth should have a 0.8-mm to 1.0-mm reduction at the margin to prevent this “light-blocking” effect onto the enamel. A shoulder preparation allowing for 0.8-mm to 1.0-mm ceramic material must be provided12 (Figures 3 and 4).
As a side note, the author has noticed that often in the use of inlay, onlay, crown, or veneer restorations with less than 0.8 to 1.0 mm of marginal reduction, a cut-back of the core is needed and traditional shoulder porcelain is necessary for the optimal aesthetic result. The only problem with this is that this shoulder material is often radiolucent and can show up as open margins or defective restorations to the uninformed clinician when doing follow-up radiographic examination.13 Due to this and the aesthetic reasons previously described, the author recommends from experience that another conventional method be utilized if the required amount of preparation cannot be obtained.
PORCELAIN LAYERING
 |
 |
| Figure 3. Left maxillary restorations on model demonstrate good aesthetics and light translucency. |
Figure 4. Left maxillary restorations cemented demonstrate the disappearance of the restorative gingival margin with the natural enamel of the tooth. (Note fit of zirconium frame and the disappearance of the white gingival line often seen with ZR cores.) |
 |
 |
|
Figure 5. Application of FD-91 for internal copying of dentinal structure. |
Figure 6. Bioesthetic layering with modifiers and transparent porcelains. |
 |
 |
| Figure 7. Restorations after first firing ready for the transparent and translucent porcelains. | Figure 8. Lingual depiction of “color from within” of Initial porcelain. Note the transparency and translucency achieved by the Bioesthetic Layering Method. |
 |
 |
|
Figure 9. Facial aesthetics of restorations with refracted and reflected light demonstrating the “halo effect” desired for optimal aesthetics. |
Figure 10. Maxillary premolar demonstrating “color within” without the use of external stains or modifiers. The color mimics natural tooth aesthetics. |
With many restorative porcelain layering techniques, technicians learned to build porcelain in the following way: apply opaque, build dentin, layer enamel, and add translucent material. Unfortun-ately, this method has little correlation with a natural tooth. Transparency is found primarily from the inside of all natural teeth, in the transparent dentin. In anterior teeth, abrasion and wear over time cause this transparent layer covering the dentin to appear at the incisal edge. This changes the transparency of natural teeth considerably depending on the angle of light or the angle of incidence. The teeth appear at times lighter, grayer, darker, or even deeper in chroma. The amount of light reflecting through the transparent dentin also changes the perception of depth.
The internal transparent layer of dentin from tooth morphology comes to the surface at the junction of the root and cervical margin, completely covering the root and influencing the value of the gingiva. Therefore, it makes no sense to use opaque marginal materials in this area where nature shows us differently. The use of GC Initial porcelain, due to its highly chromatic and fluorescent INside powders (GC America), imitates the primary dentin and fluorescence that lie imbedded within the teeth. Layering dentin material over the INside material achieves a perfect balance of chroma and value. When one pairs fluorescent, crystal clear transparency with real opalescent enamel, it makes it possible to copy the effect of natural tooth structure.
The layering of Initial porcelain has been described as the Bioesthetic Layering Method. This method is oriented toward copying the light dynamics and transmission of natural teeth. The method begins with the clinician taking the shade. This can be a very complex challenge, as one needs to make allowances for color in natural teeth under different light situations. These variances in color under different light situations are very difficult or almost impossible to achieve utilizing conventional ceramic materials. Even the most talented technicians depend on materials to produce these natural light effects. When the GC Initial materials are layered analogously to the structure of natural teeth, they automatically produce a complete and logical layering process. The natural chroma and fluorescence seen within natural teeth can be transferred to the restoration with the Bioesthetic Layering Method.
This is a method of layering porcelain through incremental layering of porcelains in a systematic manner, unlike the traditional manner described previously. The first step is the use of a fluorescent Fired Frame Modifier, since zirconium frames lack fluorescence. The next step is the application of INside materials to the cervical and proximal areas. Next, the light-reflecting edges are covered with highly fluorescent white dentin (FD-91), and the body is covered with INside material (Figure 5). Next, the dentin body is built, and the enamel table is built over the dentin body with translucent dentin. Next, modifier stains and INside material continue the layering process. The buildup is now covered with a layer of fluorescent transparent material (CLF[GC America]). Next, a cut-back in the incisal area down to the highly fluorescent dentin is accomplished, and FD-91 is again applied. Another layer of INside on the desired internal structure is placed. Next, opalescent enamel is layered (Figure 6). Now the restorations have their first bake in a porcelain oven. Any corrections to shades or colors can now be accomplished with translucent materials and opalescent enamels (Figure 7). The restorations are baked a second time and finished.
Anterior teeth pose a great aesthetic challenge. Incisals of teeth are very sensitive, since all optical light phenomena converge at this small space. Layering porcelain in the incisal table is very critical because the most light is transmitted here. This area will exacerbate the optical differences between felds-patic porcelains and synthetic ceramic frames. A totally different optical appearance can result when dissimilar frame sizes or materials are used side by side. This difference in optical appearance can be neutralized with the high fluorescent dentins and the INside powders (Figure 8).
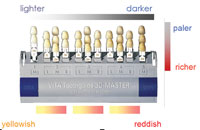
To achieve the desired natural effect at the incisal angle, Initial porcelain’s different white fluorescent, fluorescent transparent material, and transparent dentin can be utilized to provide the optical phenomenon known as the “mammelon structure” or the “Incisal halo effect” (Figure 9). If there is too much transparency at the incisal edge in the mouth, then this results as an unappealing, unnatural gray and flat effect. The use of the white fluorescent, fluorescent transparent material, and transparent dentin along with the opalescent enamels of Initial porcelain copies natural tooth structure very well (Figure 10). When compared to conventional enamels, the difference aesthetically can be enormous. The use of conventional enamels, dentins, and opaques correlates well with the Vita Lumin shade guide system, but not with the dynamics of light in natural teeth. The opalescent effect on the surface, with fluorescence coming from the inside, creates a highly natural appearance. One needs to utilize the ready-made shade guides as a general reference, but not rely on the shade guide to reproduce the desired outcome.
Communication with the laboratory technician needs to be addressed more explicitly with the design of “shade-mapping.” The clinician must communicate to the technician how and where the porcelain and modifiers are to be utilized so that the maximum aesthetic and optical effects are generated. This can pose a big challenge to the clinician when describing the colors seen to the technician. A thorough understanding of tooth morphology and natural opacious dentins, translucent dentins, and enamels in teeth must be utilized if one is to achieve the optimal effect desired. Initial has simplified this with the Bioesthetic Layering Method described earlier.9
CASE REPORT
 |
 |
|
Figure 11. Preoperative smile view of patient. |
Figure 12. Preoperative retracted view of patient’s dentition depicting failing restorations and poor aesthetics. |
 |
 |
| Figure 13. Dentition evidencing compromised gingival heights, crowding, failing restorations, wear, and overall poor aesthetics. |
Figure 14. Preoperative right lateral view. |
This patient was very unsatisfied with the anterior aesthetics of his maxillary dentition. He wanted a result that would dramatically change the anterior aesthetics. He was concerned with severe crowding of the anterior incisors as well as the failing restorations that had been present for many years. The patient was presented with a treatment plan involving a complete restoration of his dentition in both the maxillary and mandibular arches. Prior to the restorative dentistry phase he was advised to undergo orthodontic therapy as a method to improve his interdental and intradental relationship. In discussion with the author the patient elected to avoid orthodontic treatment because full-coverage restorations would be necessary to restore his dentition. Gingival concerns were discussed, as the patient was very unhappy with the differing gingival heights in the maxillary anterior segment (Figures 11 to 14).
The treatment the patient wanted to undergo at the operative session was to restore the maxillary anterior segment, periodontally recontour the maxillary anterior gingiva, and recontour the incisal edges of the opposing dentition to aid in incisal guidance. The lower arch was to be restored at a later time. The shade requested as the final shade would be considerably lighter than the patient’s intial shade.
 |
 |
| Figure 15. Right lateral view of provisional restorations at corrected vertical and incisal lengths. | Figure 16. GC Fuji Plus single-use dispensing capsule in action demonstrating precise delivery of glass ionomer adhesive material. |
The patient was appointed for the initial operative session. The first operative session included a laser-assisted Smile Lift Procedure to accomplish recontouring the gingival architecture to more harmonious and even gingival heights.14 The teeth were prepared for full-coverage restorations with a 0.8-mm to 1.0-mm circumferential marginal reduction. Tissue retraction, impressions, bite records, and provisional restorations were all accomplished at this session (Figure 15).
Upon completion of the restorations, the second operative session was to be the try-in phase to determine restoration fit, marginal integrity, occlusion, aesthetics, and patient satisfaction. With all these accomplished, the restorations were to be placed with final cement. Zirconium restorations can be easily cemented in the conventional manner with glass ionomer cements or conventional ce-ments. The cement chosen for this case was GC Fuji Plus (GC America). The author utilizes this product due to high fluoride release and high bond strengths.15-17 This cement is very versatile due to its ability to cement indirect restorations. The material is supplied in a capsule (Figure 16). It is also available as a Paste-Pak system (FujiCEM). This ensures the proper mixing ratio every time to achieve the highest compressive, tensile, and bond strengths with the lowest film thickness, and maximum fluoride release.18
 |
 |
| Figure 17. Fully retracted view of final restorations in maxillary arch. (The higher value restorations that the patient requested will be matched during the mandibular reconstruction phase.) | Figure 18. Final restorations showing translucency and transparency of the zircon frame/Initial porcelain technique. |
 |
 |
|
Figure 19. Preoperative smile view of patient. |
Figure 20. Postoperative smile view of patient. |
The final results were very aesthetic, and the patient was highly pleased with the results. A third and final operative session was utilized for occlusal accuracy and postoperative evaluation. There was little to no sensitivity during the entire procedure as well as during the provisional and postoperative phase (Figures 17 to 20).
References
- Adams MW. Dental implants—isn’t it about time? J Indiana Dent Assoc. 2002;81:9-10.
- The U.S. Dental Laboratories Industry. 3rd ed. Tampa, Fla: Marketdata Enterprises; 2005.
- Pospiech P, Rammelsberg P, Goldhofer G, et al. All-ceramic resin-bonded bridges: a 3-dimensional finite-element analysis study. Eur J Oral Sci. 1996;104(4 pt 1):390-395.
- Sorensen JA, Kang SK, Torres TJ, et al. In-Ceram fixed partial dentures: three-year clinical trial results. J Calif Dent Assoc. 1998;26:207-214.
- Keough BE, Kay HB, Sager RD. A ten-unit all-ceramic anterior fixed partial denture using Y-TZP Zirconia. Pract Proced Aesthet Dent. 2006;18(1):37-43.
- Luthardt RG, Holzhuter MS, Rudolph H, et al. CAD/CAM-machining effects on Y-TZP zirconia. Dent Mater. 2004;20:655-662.
- Guazzato M, Quach L, Albakry M, et al. Influence of surface and heat treatments on the flexural strength of Y-TZP dental ceramic. J Dent. 2005;33:9-18.
- Raigrodski AJ. All-ceramic full-coverage restorations: concepts and guidelines for material selection. Pract Proced Aesthet Dent. 2005;17:249-256.
- Brusch M, Dahl R. Systematic bioesthetic dental restorations: a ceramic solution with overlapping systems, part 2. Dental Dialogue. 2005;5(June):26-42.
- Schenk H. Esthetics with zirconia. Dental Dialogue. April 2006:118-128.
- Hammer P. Experiences from the laboratory. Dental Dialogue. April 2006:34-46.
- Brusch M, Dahl R. Systematic bioesthetic dental restorations: a ceramic solution with overlapping systems, part 1. Dental Dialogue. 2005;5(June):2-24.
- Rosentritt M, Behr M, Lang R, et al. Marginal adaptation of ceramic inlays using different types of cements. Presented at: The IADR 80th General Session; San Diego, Calif; March 6-9, 2002; Abstract 0053.
- Pinero J. The smile lift procedure. Contemp Esthet Restor Pract. 1998;2:44-52.
- McMillen K, Kerby RE, Thakur A, et al. Fluoride release of resin-based luting cements. Presented at: The IADR 1996 General Session; Abstract 403.
- Burgess JO, Norling BK, Cardenas HL. Fluoride release and flexural strength of five fluoride releasing luting agents. Presented at: The IADR 1996 General Session; Abstract 423.
- Wilson PR, Stankiewicz NR. Effect of cement space and delayed placement on the seating of crowns luted with Vitremer, Fuji Duet and Dyract Cem. Am J Dent. 1998;11:240-244.
- Begazo CC, de Boer HD, Kleverlaan CJ, et al. Shear bond strength of different types of luting cements to an aluminum oxide-reinforced glass ceramic core material. Dent Mater. 2004;20:901-907.
Dr. Pinero maintains a private practice in Milwaukee, Wis, where he emphasizes aesthetic, restorative, and laser dentistry. Dr. Pinero lectures nationally and internationally on aesthetic, restorative, and laser dentistry and provides hands-on in-office programs on aesthetic and laser dentistry. He founded The Midwest Institute of Laser and Esthetic Dentistry in Milwaukee, where he holds advanced postgraduate continuum seminars on aesthetic and laser dentistry. In addition to clinical training, Dr. Pinero has helped numerous dentists employ his expertise of patient management to help them propel their practices to be among the top 5% with his Follow the Formula system. He can be reached at (414) 282-2050.
Acknowledgment
The author would like to thank Robert Popp of Popp DCS in Milwaukee, Wis, and laboratory technician Ernest Grabowski of Popp Dental Laboratory for the laboratory phase of this case.