Most dental practices routinely treat patients who have prosthetic joints, pins, screws, or plates. For many years, conflicting advice was offered regarding the administration of prophylactic antibiotics prior to dental procedures. In 1997, the ADA and the American Academy of Orthopaedic Surgeons (AAOS) issued an advisory statement containing prophylaxis guidelines.1 The ADA/AAOS expert panel concluded that antibiotic prophylaxis is not indicated for dental patients who have pins, screws, or plates, and it is not routinely indicated for the majority of dental patients who have total joint replacements. It is advisable to consider antibiotic prophylaxis for those dental patients who may be at increased risk for hematogenous total joint infection.
Over the past 5 years, the ADA/AAOS guidelines have been widely adopted in the United States, and additional insightful data have appeared in the literature.2 This article discusses the guidelines in light of current knowledge.
THE PROBLEM
In ever-increasing numbers, hundreds of thousands of patients annually in the United States are undergoing total joint arthroplasties.3 Implantation of prosthetic devices during arthroplasty introduces the risk of deep joint infections, which may occur in the early postoperative period or months to years later.4 Many early joint infections are thought to be caused by surgical wound contamination, demonstrating organisms such as Staphylococcus epidermidis. Late joint infections, however, are sometimes associated with the introduction of bacteria such as Streptococcus viridans introduced into the bloodstream (bacteremia) from distant sites and the subsequent seeding of organisms into vulnerable prosthetic joint spaces.5 Because some dental procedures produce significant transient bacteremias6 and acute dental infections produce substantial, sustained bacteremias, some clinicians have assigned a cause-and-effect relationship to cases of septic joints following documented dental treatment or oral infections.7 Late prosthetic joint infections have a severe morbidity and, more importantly, mortality rate. Therein lies the serious concern regarding prophylaxis and prevention.
Prior to the statement by the expert panel of the ADA/AAOS, conflicting advice was given to dentists by professional groups and individual clinicians.8 Advice ranged from condemning the use of prophylactic antibiotics for any dental procedures9 to advocacy of prophylaxis for all treatment, regardless of the bacteremia risk.10 The selection and dosing of antibiotics was also controversial.11 The 1997 recommendations correlated those patients who are most at risk for joint infections with their proposed dental treatments and the appropriate antibiotic regimen.
At-risk Joint Prosthesis Patients
| Table 1. Patients With a Potential for Increased Risk of Hematogenous Total Joint Infection* |
| • Immunocompromised patients disease/drug/radiation-induced suppression inflammatory arthropathies rheumatoid arthritis systemic lupus erythematosus • Insulin-dependent diabetics • Hemophiliacs • Malnourished patients • Joint replacement patients: first 2 years after joint surgery • Joint replacement patients: previous prosthetic joint infection *Adapted from the American Academy of Orthopaedic Surgeons/American Dental Association. J Am Dent Assoc. 1997;128. |
Certain groups of patients who have joint prostheses are at higher risk for bloodborne infections (Table 1). All immunocompromised or immunosuppressed patients are more susceptible to hematogenous infections. Patients who have rheumatoid arthritis, systemic lupus erythematosus,12 or other inflammatory arthropathies are at risk. Patients who are immunosuppressed from radiation therapy, drug therapy, or disease are similarly at risk. Insulin-dependent diabetes, hemophilia, and malnourishment also increase the risk for infection from bloodborne organisms. All such compromised joint prosthesis patients should be considered for antibiotic prophylaxis prior to high-risk dental procedures.
Specifically relating to joint prostheses in patients who are not otherwise compromised, two additional groups of patients should be strongly considered for antibiotic prophylaxis prior to risk-provoking dental treatment: those who have a history of previous prosthetic joint infections or those who have undergone joint prosthesis surgery during the prior 2 years.
RISK-PRONE DENTAL PATIENTS
| Table 2. Stratification of the Incidence of Bacteremia Associated With Dental Procedures* |
|
HIGHER INCIDENCE LOWER INCIDENCE
*Adapted from the American Academy of Orthopaedic Surgeons/American Dental Association. J Am Dent Assoc. 1997;128. |
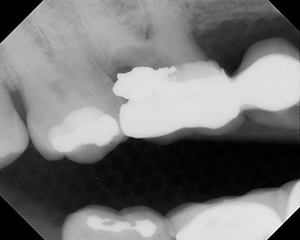
Not all dental procedures are thought to increase the risk of significant bacteremias.13 The 1997 recommendations stratify dental procedures into high incidence and low incidence of bloodborne spread of bacteria (Table 2). High-incidence bacteremia procedures include dental extractions, extensive periodontal manipulation, dental implant placement, reimplantation of avulsed teeth, endodontic instrumentation, apical surgery, initial placement of orthodontic bands, intraligamentary local anesthetic injections, and dental prophylaxis that stimulates hemorrhage. It is reasonable to state that any other procedure the attending dentist clinically judges to be at high risk for promoting a significant bacteremia should be included. In particular, procedures that require significant manipulation of the gingival or oral mucosa create the potential for measurable bacteremias and may be included in the high-risk category at the discretion of the dentist.
Low-incidence bacteremia procedures are said to include restorative dentistry, local anesthetic injections, intracanal endodontic procedures, rubber dam placement, suture removal, seating of prostheses, impression taking, fluoride treatment, taking of oral radiographs, and orthodontic appliance adjustment. However, Roberts and colleagues14 reported that even simple dental restorations can result in a bacteremia comparable to that of dental extractions. In their study of conservative dental procedures in children, the operative-restorative procedures producing the greatest bacteremias were rubber dam placement and matrix band/wedge placement. Therefore, the attending dentist must judge whether or not a procedure is low risk for promoting a significant bacteremia in the individual patient.
In recent years, additional data have further pointed toward a relationship between dental treatment, oral bacteria, and septic joint disease. LaPorte et al15 reviewed the records of 2,973 cases of total hip joint arthroplasty in which late infections occurred in 52 patients, three being “strongly associated with a dental procedure.” By culture from the infected joints, S viridans was identified in two patients and Peptostreptococcus was identified in the third patient. Two of the patients had additional risk factors of diabetes mellitus (one case) and rheumatoid arthritis (one case). These three patients had dental procedures exceeding 45 minutes and none received perioperative antibiotics.
Nadlacan and Hirst16 reported a late infection of a total knee replacement following a dental procedure in a hemophiliac patient. Kaar et al17 reported a case of acute infection 11 months after revision of a hip arthroplasty, with signs of infection occurring 30 hours after a noninvasive supragingival dental prophylaxis, without antibiotic coverage.
Bacteremia risk assessment of dental procedures combined with the risk delineation of prosthetic joint patients facilitates the antibiotic premedication decision. For example, a non-immunocompromised dental patient who had a total joint replacement more than 2 years prior to operative procedures that do not induce significant gingival manipulation is not indicated for antibiotic prophylaxis. Further, this patient is probably more at risk for serious medication complications from the use of antibiotics than from dental treatment-induced late joint infection.
ANTIBIOTIC REGIMENS
| Table 3. Antibiotic Prophylaxis Regimens* |
|
• Patients not allergic to penicillin: 2 g amoxicillin or cephalexin or cephradine, 1 hour pre-op, no follow-up dose • Patients allergic to penicillin: 600 mg clindamycin, 1 hour pre-op, no follow-up dose • Patients unable to take oral medications: 1 g cefazolin or 2 g ampicillin IM or IV, 1 hour pre-op • Patients allergic to penicillin and unable to take oral medications: 600 mg clindamycin IV, 1 hour pre-op *Adapted from the American Academy of Orthopaedic Surgeons/American Dental Association. J Am Dent Assoc. 1997;128. |
A 2-g dose of amoxicillin, cephalexin (Keflex), or cephradine (Velosef, Cefril) 1 hour prior to dental procedures is the recommended antibiotic regimen for patients not known to be allergic to penicillin. No follow-up dose is indicated (Table 3).
For patients known to be allergic to penicillin, the alternative medication is an oral dose of 600 mg clindamycin (Cleocin) 1 hour prior to dental procedures. No follow-up dose is indicated.
A l-g dose of cefazolin (Ancef, Kefzol) or 2-g dose of ampicillin may be given intramuscularly or intravenously 1 hour prior to dental procedures for patients unable to tolerate oral medication and not known to be allergic to penicillin. No follow-up dose is indicated.
A 600-mg dose of clindamycin may be given intravenously 1 hour prior to dental procedures for patients unable to tolerate oral medication and known to be allergic to penicillin. No follow-up dose is indicated.
WHY NOT USE ANTIBIOTICS?
Some dentists, physicians, and patients advocate the use of antibiotics for all joint prosthesis patients, regardless of the risk for joint sepsis. When making this decision, dentists should consider the risks associated with antibiotic intake. These hazards include overgrowth of pathogenic organisms, secondary infections, bacterial resistance in the host, and allergic reactions, including fatal anaphylactic reactions.18 Patients can best be served when dentists and physicians use clinical judgment in concert with the ADA/AAOS guidelines.
In cases in which patients have followed recommendations at variance with the ADA/AAOS guidelines, the attending dentist should re-consult with the attending physician. There are, of course, instances in which an alternative regimen is advisable and prudent, for example, the substitution of a macrolide or cephalosporin in patients who recently received a course of amoxicillin. In such cases, the dentist and the physician may wish to review the current ADA/AAOS recommendations together before a final decision is made.
TOPICAL ANTISEPTIC AGENTS
Some practitioners recommend antimicrobial mouth rinses or irrigations prior to dental procedures or on a daily basis. Research does not support this practice. The issue of bacteremia from the oral cavity is central to prophylaxis against infective endocarditis, as well as for joint replacement care. Much of the bacteremia research applies to both situations. The American Heart Association does not recommend forceful rinsing with antiseptic agents for fear of bacterial resistance development.19 Foote et al20 demonstrated that the use of chlorhexidine was actually detrimental to patients undergoing head and neck radiation therapy. Furthermore, Brown et al21 showed no significant reduction in the bacteremia with the use of oral rinses. Rahn et al22 did show a significant reduction in post-extraction bacteremia from sulcus irrigation with povidone iodine, while chlorhexidine was much less efficacious as a sulcus irrigation agent.
DENTAL CARE FOR JOINT SURGERY PATIENTS
All patients preparing for total joint surgery would benefit from a complete clinical dental examination, appropriate dental radiographs, elimination of any oral source of infection, completion of indicated dental treatment, and reinforcement of home care instructions. Following joint surgery, all patients should be encouraged to practice excellent oral hygiene, receive regularly scheduled oral examinations, and continue professional dental care.
FUTURE RECOMMENDATIONS
The ADA supported the work of the ADA/AAOS expert panel. The resulting 1997 guidelines have greatly clarified a controversial area of clinical practice. Clifford W. Whall, Jr, PhD, of the ADA Council on Scientific Affairs, has noted that a complete review of the literature and the guidelines is anticipated in the next few years (personal communication, telephone conversation, April 3, 2002).
SUMMARY
At this time, all dentists and physicians should be very familiar with the 1997 ADA/AAOS antibiotic prophylaxis recommendations for joint prosthesis patients who are undergoing dental treatment. The guidelines identify physical conditions that place joint replacement patients at the highest risk for joint sepsis. They also stratify dental procedures into higher-risk and lower-risk categories. Combining these two groupings clarifies the dentist’s strategy for antibiotic prophylaxis protocols, which are greatly simplified over previous practices. Of notable importance is the elimination of posttreatment antibiotic dosing, the reduction of the loading dose of antibiotic, and the identification of a large group of joint replacement patients who do not require antibiotic prophylaxis prior to dental treatment. Every dentist must use clinical judgment, knowledge of the patient, and consultation with the attending physician to determine the appropriate treatment plan.
References
1. Advisory Statement. Antibiotic prophylaxis for dental patients with total joint replacements. J Am Dent Assoc. 1997;128:1004-1008.
2. Waldman BJ, Mont MA, Hungerford DS. Total knee arthroplasty infections associated with dental procedures. Clin Orthop. 1997;343:164-172.
3. Curry S, Phillips H. Joint arthroplasty, dental treatment, and antibiotics: a review. J Arthroplasty. 2002;17:111-113.
4. Maderazo EG, Judson S, Pasternak H. Late infections of total joint prostheses: a review and recommendations for prevention. Clin Orthop. 1998;229:131-142.
5. Jacobson JJ, Matthews LS. Bacteria isolated from late joint infections: dental treatment and chemoprophylaxis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1987;63:122-126.
6. Kuriyama T, Karasawa T, Nakagawa K, et al. Bacteriologic features and antimicrobial susceptibility in isolates from orofacial odontogenic infections. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:600-608.
7. Skiest DJ, Coykendall AL. Prosthetic hip infection related to a dental procedure despite antibiotic prophylaxis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;79:661-663.
8. Sandhu SS, Lowry JC, Reuben SF, et al. Who decides on the need for antibiotic prophylaxis in patients with major arthroplasties requiring dental treatment: is it a joint responsibility? Ann R Coll Surg Engl. 1997;79:143-147.
9. Simmons NA, Ball AP, Cawson RA, et al. Case against antibiotic prophylaxis for dental treatment of patients with joint prostheses. Lancet. 1992;339:301.
10. D’Angelo GL, Ogilvie-Harris DJ. Septic arthritis following arthroscopy, with cost/benefit analysis of antibiotic prophylaxis. J Arthroscopy. 1988;4:10-14.
11. Nguyen TT, Garibaldi JA. Cephalosporin versus penicillin. W V Dent J. 1995;69:16-21.
12. Miller CS, Egan RM, Falace DA, et al. Prevalence of infective endocarditis in patients with systemic lupus erythematosus. J Am Dent Assoc. 1999;130:387-392.
13. Little JW. Patients with prosthetic joints: are they at risk when receiving invasive dental procedures? Spec Care Dentist. 1997;17:153-160.
14. Roberts GJ, Gardner P, Longhurst P, et al. Intensity of bacteraemia associated with conservative dental procedures in children. Br Dent J. 2000;188:95-98.
15. LaPorte DM, Waldman BJ, Mont MA, et al. Infections associated with dental procedures in total hip arthroplasty. J Bone Joint Surg Br. 1999;81:56-59.
16. Nadlacan LM, Hirst P. Infected total knee replacement following a dental procedure in a severe haemophiliac. Knee. 2001;8:159-161.
17. Kaar TK, Bogoch ER, Devlin HR. Acute metastatic infection of a revision total hip arthroplasty with oral bacteria after noninvasive dental treatment. J Arthroplasty. 2000;15:675-678.
18. Physician’s Desk Reference. Montvale, NJ: Medical Economics Co; 2002;1486.
19. Dajani AS, Taubert KA, Wilson W, et al. Prevention of bacterial endocarditis: recommendations by the American Heart Association. JAMA. 1997;277:1794-1801.
20. Foote RL, Loprinzi CL, Frank AR, et al. Randomized trial of a chlorhexidine mouthwash for alleviation of radiation-induced mucositis. J Clin Oncol. 1994;12:2630-2633.
21. Brown AR, Papasian CJ, Shultz P, et al. Bacteremia and intraoral suture removal: can an antimicrobial rinse help? J Am Dent Assoc. 1998;129:1455-1461.
22. Rahn R, Schneider S, Diehl O, et al. Preventing posttreatment bacteremia: comparing topical povidone-iodine and chlorhexidine. J Am Dent Assoc. 1995;126:1145-1148.
Dr. Rothstein maintains a private practice in Jacksonville, Fla. He is a diplomate of the American Board of Oral and Maxillofacial Surgery. He may be contacted at (904) 743-5604 or marjerry@fdn.com.