INTRODUCTION
It’s all over the news: Dentists are treating more cracked teeth since the onset of the COVID-19 pandemic—sometimes at twice the typical rate.1 The vast majority of dentists indicate that the prevalence of stress-related oral health conditions among their respective patients has increased since the beginning of the COVID-19 pandemic, according to the ADA Health Policy Institute’s latest data from its COVID-19 economic-impact tracking poll conducted the week of February 15.2 More than 70% of dentists surveyed saw an increase of patients experiencing teeth grinding and clenching, conditions often associated with stress—up from just under 60% in the fall. Dentists also reported increases in chipped teeth (63%); cracked teeth (63%); and temporomandibular joint disorder symptoms (62%), which includes headaches and jaw pain.2
Pandemic stress, quarantine fatigue, mask burnout, online overload—whatever you want to call it, it’s added stress that people across the globe are experiencing. Stress comes out in many different ways, and each person responds differently, but there is definitely a trend of stress-related issues in dentistry. Management of this stress is a primary concern. Whether you practice mindfulness, begin a yoga habit, or seek professional medical help, addressing the feelings you’re having now is as important as treating the symptoms they are causing.3 The key to any successful treatment plan is understanding the cause of the current condition. This allows you to arrive at the correct diagnosis and develop a treatment plan that will have a predictable, long-term, successful outcome. So, on the surface, the treatment of a cracked tooth may seem simple: Restore the crack with a crown or another appropriate restoration, and that is it. However, if the underlying cause has not been addressed, your treatment is susceptible to failure.4
Cracked teeth and the various complications that arise with this particular type of case can be one of the most significant challenges facing the preventive, restorative dentist today. They present a clinical challenge due to their complex diagnosis and unpredictable prognosis. Treatment often varies depending on the nature of the crack and the clinical experience of the operator. Cracked teeth are challenging to diagnose clinically because of the complicated and diverse symptoms associated with this condition and the challenge in locating crack lines. There is no consensus among dental practitioners regarding the best approach to treat cracked teeth. But what we do know is the treatment and outcome for a cracked or fractured tooth is dependent on the location, direction, type, and size of the crack.5,6 Being able to distinguish these differences can aid in a diagnosis that will ultimately lead to proper care and treatment. The American Association of Endodontists has classified 5 types of cracks in teeth7:
- Craze lines
- Fractured cusp
- Cracked tooth
- Split tooth
- Vertical fracture
These 5 categories of dental fractures have been devised to provide global definitions that researchers and clinicians can use to decrease this confusion. Combining this knowledge with a proper dental history, clinical examination, and radiographic assessment, as well as a periodontal and occlusal evaluation, can help one determine the proper course of treatment for a particular case.8
The following case presentation will highlight the treatment of an incomplete fracture of an upper second premolar. Though there were many ways to approach the treatment of this particular case, the modality chosen focused on a minimally invasive approach involving immediate dentin seal and its emphasis on crack repair.9
CASE REPORT
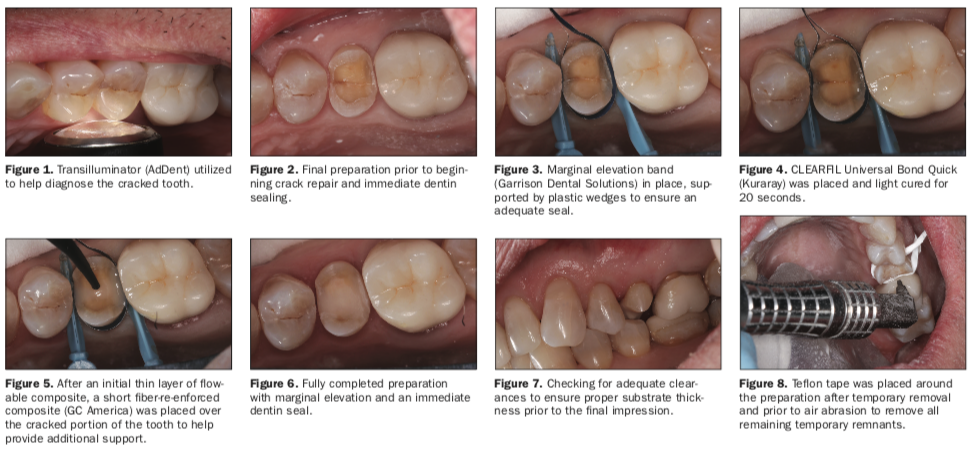
A 60-year-old male patient in good physical health with no underlying medical complications presented complaining of discomfort when biting on his upper left side for approximately the previous 10 days. A radiograph, as well as a visual examination, was conducted, along with a periodontal and endodontic evaluation. It was determined rather quickly that the upper right second premolar was the culprit. Utilizing a transillumination device (AdDent), the large fracture running mesial to distal was easily visualized (Figure 1). Radiographically, there was no sign of pathology, and all vitality testing came back within normal limits. Periodontally, the same can be said regarding the lack of significant findings, as all probe readings were in the normal range of 2 to 3 mm. Treatment options, and the understanding of the complexities of treating a fractured tooth like this, were discussed with the patient. He understood that there was no guarantee that this tooth could be saved with 100% predictability. An integral part of dealing with cracked teeth is that the patient fully understands the situation and has total buy-in when deciding on the course of treatment.
The area was then anesthetized (4% articaine, 1:100,000 epinephrine [Septodont]). Isolation was achieved utilizing a DryShield evacuation system to help achieve an optimal working environment. Being a virgin tooth, the fractured premolar was then explored by utilizing a pear-shaped diamond bur (Meisinger) to begin to evaluate the depth of the fracture. Approaching this fundamentally, the design principles involved in minimally invasive dentistry, combined with a biomimetic approach, helped me establish a protocol when chasing a fracture. The ideal goal was to chase the fracture to a depth of 5 mm from the occlusal surface and a depth of 3 mm interproximally from the axial wall.10 I tried to be careful not to remove too much of the cracked dentin and cause a pupal exposure. The preparation felt complete after I flattened out both the buccal and lingual cusps utilizing an 856 diamond bur (Meisinger) to create a cusp clearance of approximately 1.5 mm. I utilized a large enamel band to help take this preparation from a predominantly tensile position to one of compression, enabling the support to be transferred away from the remaining fractured dentin (Figure 2). Feeling comfortable with my preparation, a marginal elevation band (Garrison Dental Solutions) was placed and secured with 2 interproximal wedges (Palodent Plus System [Dentsply Sirona]) (Figure 3). The band is being utilized to help me raise the interproximal margins slightly supragingival, as well as support the bio base at the interproximal. The fracture was still partially in the dentin-enamel complex, and I was not comfortable chasing that fracture any further. With the band in place, CLEARFIL Universal Bond Quick (Kuraray) was applied to the tooth in an agitated fashion for roughly 10 seconds, then air thinned with a dedicated air line to help reduce contaminants, and then light cured for 20 seconds with an LED curing light (PinkWave [Vista Apex]) (Figure 4). CLEARFIL MAJESTY Flow (Kuraray) was then applied to the entire dentin-bonded surface at a depth of 0.5 mm in a horizontal fashion and light cured for 20 seconds. Some everX Flow (GC America) was applied directly over the fractured portion of the preparation at a depth of approximately 1 mm. This is a short fiber-reinforced flowable composite that increases the fracture toughness of the tooth and should prevent the existing dentin crack from propagating and causing failure (Figure 5).11 The multidirectional fibers found in everX Flow helped bridge the crack and transferred the stresses to regions of greater structural integrity. Finally, a thin layer of CLEARFIL MAJESTY Flow was placed over the everX Flow to ensure a smooth transition and polymerized for the final time for 20 seconds. The band was removed, and the surface was polished with Enhance Finishing Cups (Dentsply Sirona) to remove any flash or possible discrepancies prior to taking our final scan (Figures 6 and 7). The temporary was cemented and the tooth was taken slightly out of occlusion in all excursions. Detailed instructions were given to the patient in regard to home care and management of that area while the permanent restoration was being fabricated.
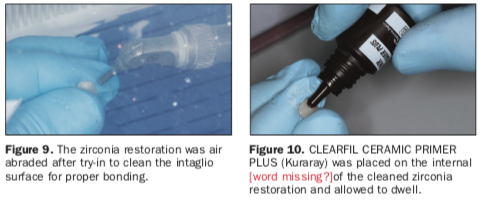
Upon returning to the office, the patient was happy to report there were no signs of discomfort or anything to lead us to believe that we were on the wrong path to a successful outcome. The area was once again anesthetized (4% articaine, 1:100,000 epinephrine [Septodont]), and a DryShield Evacuation System was placed to help in the removal of the temporary and in the bonding protocol of our final restoration. After removal of the temporary, a large piece of Teflon tape was wrapped around the preparation to help protect the gingiva, and air abrasion was performed with the PrepStart H2O (Zest Dental Solutions) utilizing 50-µm aluminum oxide to clean the immediate dentin seal-coated surface (Figure 8). The zirconia restoration (Argen) was then tried in and adjusted to our specific needs. It was then taken to the lab, where it was air abraded for 5 to 6 seconds with 27-µm aluminum oxide to ensure a clean intaglio surface was achieved (Figure 9). In order to bond zirconia restorations, it is critical one achieves an activated surface free of any contaminants that can hinder the chemical interaction. This can be achieved with the introduction of the phosphate monomer MDP.12 The MDP monomer has a very strong affinity to phosphate, which is the predominant component in freshly cleaned zirconia. CLEARFIL CERAMIC PRIMER PLUS (Kuraray), the MDP-containing primer used in our case, was applied to the intaglio surface and allowed to dwell (Figure 10).
With the restoration now ready, the tooth was then prepared by placing 35% phosphoric acid in a total-etch technique for 20 seconds, and then it was rinsed and dried. CLEARFIL Universal Bond Quick (Kuraray) was placed on the tooth and scrubbed and agitated for 10 seconds prior to air thinning until a lack of bonding agent movement was seen along the preparation (Figure 11). PANAVIA SA Universal Cement (Kuraray) was placed directly on the uncured bonding agent, and the restoration was then seated (Figure 12).
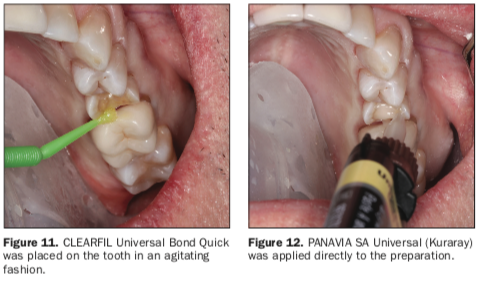
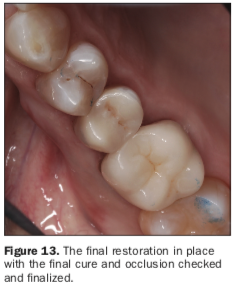
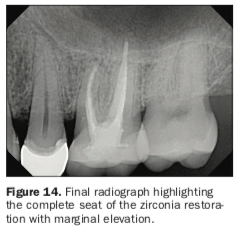
One of the unique features and reasons as to why this cement combination was chosen was because of the built-in dual-cure formulation between CLEARFIL Universal Bond Quick and PANAVIA SA Universal. By not having to polymerize the bonding agent prior to cementation, this ensured that there would be no pooling anywhere along the preparation to create an insufficient seating of the restoration. The restoration was then tack-cured for 3 seconds, and excess cement was removed facially and lingually as well as interproximally with floss. After all excess cement was removed, the restoration was then light cured from all directions for 20 seconds. Enhance Finishing Cups were used to polish the facial and lingual surfaces before checking occlusion. A fine diamond (Meisinger) was used to adjust, and the final polish was completed with a 3-step intraoral zirconia-polishing system (Meisinger) (Figure 13). Postoperative instructions were discussed with the patient, and a final radiograph was taken to ensure complete seating of the restoration and integration with our prior marginal elevation (Figure 14).
CLOSING COMMENTS
The protocol for preventing and treating cracked teeth is advanced yet simplified. By choosing a treatment modality that replaces lost or damaged tooth structure with proper materials and maximum bond strengths while minimizing the stress, we can ultimately achieve a durable and maintainable restoration. Today’s materials provide all of that in reliable bonding technology and flexural strengths, allowing us to prepare non-geometric, retentive preparations that take advantage of the built-in physical properties of natural tooth structure while avoiding the ever-destructive 360° margin preparations. Using biomimetic restorative protocols and concepts increases the longevity of restorative dental treatments and reduces or eliminates future cycles of retreatment, a concept that both the dentist as well as the patient can enjoy every day.
REFERENCES
1. American Dental Association. HPI poll: Dentists see increase in patients’ stress-related oral health conditions. September 28, 2020.
2. American Dental Association. HPI poll: Dentists see increased prevalence of stress-related oral health conditions. March 2, 2021.
3. Harvard Health Publishing. Best ways to manage stress. January 8, 2015.
4. Mamoun JS, Napoletano D. Cracked tooth diagnosis and treatment: An alternative paradigm. Eur J Dent. 2015;9(2):293-303. doi:10.4103/1305-7456.156840
5. Lee JJ, Kwon JY, Chai H, et al. Fracture modes in human teeth. J Dent Res. 2009;88(3):224–8. doi: 10.1177/0022034508330055
6. Seo DG, Yi YA, Shin SJ, et al. Analysis of factors associated with cracked teeth. J Endod. 2012;38:288–92. doi:10.1016/j.joen.2011.11.017
7. American Association of Endodontists. Cracking the cracked tooth code: detection and treatment of various longitudinal tooth fractures. Summer 2008.
8. Abou-Rass M. Crack lines: the precursors of tooth fractures-their diagnosis and treatment. Quintessence Int Dent Dig. 1983;14:437–47.
9. Magne P. Esthetic and Biomimetic Restorative Dentistry: Manual for Posterior Esthetic Restorations. University of Southern California School of Dentistry; 2006.
10. Alleman DS, Magne P. A systematic approach to deep caries removal end points: the peripheral seal concept in adhesive dentistry. Quintessence Int. 2012;43(3):197-208.
11. Garoushi S, Sungur S, Boz Y, et al. Influence of short-fiber composite base on fracture behavior of direct and indirect restorations. Clin Oral Investig. 2021;25(7):4543-4552. doi:10.1007/s00784-020-03768-6
12. Blatz MB, Alvarez M, Sawyer K, et al. How to bond zirconia: the APC concept. Compend Contin Educ Dent. 2016;37(9):611-617; quiz 618.
ABOUT THE AUTHOR
Dr. Schmedding graduated from the University of Puget Sound prior to getting his DDS degree at the University of the Pacific, Arthur A. Dugoni School of Dentistry. For 17 years, Dr. Schmedding practiced in Seattle prior to relocating to California. He held a position as an assistant professor in the Department of Integrated Reconstructive Dental Sciences at the University of the Pacific, Arthur A. Dugoni School of Dentistry. In addition to his pursuits in academia, Dr. Schmedding enjoys his private practice in Walnut Creek, Calif, and lectures nationally and internationally on topics ranging from advanced dental materials and products to complex restorative procedures. He has published articles both nationally and internationally regarding dental restorative materials and procedures. Dr. Schmedding is a current member of the ADA, the California Dental Association, and the American Academy of Cosmetic Dentistry. He is one of 450 dentists worldwide to be an accredited member of the American Academy of Cosmetics. He can be reached at troy.schmedding.dds@gmail.com.
Disclosure: Dr. Schmedding received an honorarium from Kuraray Noritake for writing this article.











