INTRODUCTION
Perforation of the maxillary sinus by a dental implant is a concern for many dental implant clinicians. Maxillary sinus floor elevation (SFE) is used to augment insufficient alveolar bone when placing dental implants in the maxillary posterior region and can be accomplished via a trans-alveolar approach1 or a lateral approach.2,3
The most common complication during SFE is the perforation of the Schneiderian membrane,4,5 with a reported prevalence of 8% to 32%.6,7 The risk factors include the presence of sinus septa, low residual bone height, and smoking.8 Some studies have found that membrane perforation increased the possibility of developing sinusitis.8,9 It has been reported that survival rates do not differ significantly between implants placed under perforated or intact Schneiderian membranes8; however, there are studies reporting a relationship between membrane perforation and graft or implant failures.9,10 It is thought that the displacement of a graft material into the sinus may be responsible for complications such as maxillary sinusitis after sinus perforation.8 Therefore, various methods aimed at repairing the perforated membrane have been developed, including suturing and the use of fibrin adhesives and absorbable collagen membranes.11,12 However, most of these studies presented repair procedures via a lateral approach for SFE.
Membrane perforation is the most common complication of the SFE procedure9 and is usually repaired via a lateral approach.13 However, when perforation occurs during SFE, the lateral approach requires a second operation site and increases patient discomfort.
The prevalence of maxillary sinusitis after SFE has been reported to be 8.4% to 9.8%,14,15 with the incidence rate of sinusitis being lower for a crestal approach than for a lateral approach.16 Membrane perforation is a risk factor for postoperative sinusitis,14 which decreases the survival rates of implants.16
With regard to sinus membrane elevation surgery, some complications are inevitable, even though prevention is the best method. Once complications occur, the clinician should acquaint himself or herself with the cause, explain the issue to the patient, and treat the complications accordingly. Cases of serious complications should be promptly referred to a related specialist.15 During surgery, the most common complication is sinus membrane perforation, which could increase the risk of post-op infection and failure of the graft and/or implant. Therefore, it is necessary to be aware of the various methods for closing perforations. After surgery, an infection is the most common complication; early diagnosis and treatment (antibiotics and incision drainage) are very important for the prevention of severe complications.15,16
To minimize complications such as bleeding and sinus membrane perforation, the normal anatomical structures and pathological findings should be identified and diagnosed before surgery. Cooperation with an otorhinolaryngologist should be considered in cases of asymptomatic maxillary sinus lesions, nasomental patency, chronic maxillary sinusitis, mucous retention cysts, and nasal septum deviations.16 To prevent arterial bleeding, the clinician should evaluate the vertical resorption of alveolar bone and the position of the posterior superior alveolar artery.11 Sinus lateral wall thickness is very different for each individual. If the wall thickness is too thin or thick, there is a high possibility of perforation of the sinus membrane during formation of the bony window.11,12 Asymptomatic mucous retention cysts and antral pseudocysts are not a contraindication. However, mucoceles with extensive and destructive aspects are a contraindication for sinus membrane elevation. Sinus elevation is often difficult in cases with mucous retention cysts or pseudocysts where aspiration with a 21-gauge needle could be effective for sinus elevation, bone grafting, and implant placement.14 Sinus septums have been reported in 16% to 58% of patients and could increase the risk of membrane perforation.2,3 Normal sinus membrane thickness is 0.3 to 0.8 mm, and cilia cells remove various secretions and foreign substances formed in the maxillary sinus. If there is a lesion causing maxillary sinusitis or a history of sinus-related surgery, the risk of post-op complications, such as maxillary sinusitis, greatly increases because the cilia cells cannot function normally.11 The most important factor to identify before surgery is maxillary ostium patency (osteomeatal patency), the lack of which could cause post-op maxillary sinusitis due to an issue with the maxillary sinus drainage system. In addition, the risk of post-op complications also increases in cases of nasal septum deviation and nasal mucosa inflammation or injury.12
CASE REPORTS
Case 1
An ASA II, 45-year-old, male patient was missing tooth No. 14 (upper left first molar) for a long time. The patient expressed dissatisfaction with his missing teeth before this appointment. He had previously consulted with many other dentists and was not completely satisfied with the treatment options presented to him. The patient was skeptical about sinus lift surgery. However, he was unwilling to choose other alternative treatments, such as a bridge.
After an initial conversation and discussion with the patient regarding the right approach and treatment plans, he was reassured and decided to proceed with a crestal sinus lift using the Crestal Approach Sinus Kit (CAS Kit) (Hiossen) followed by an implant placement.
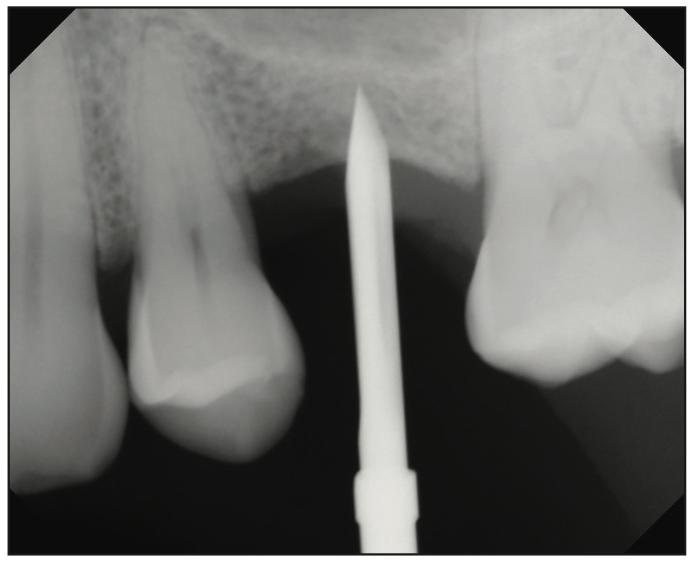
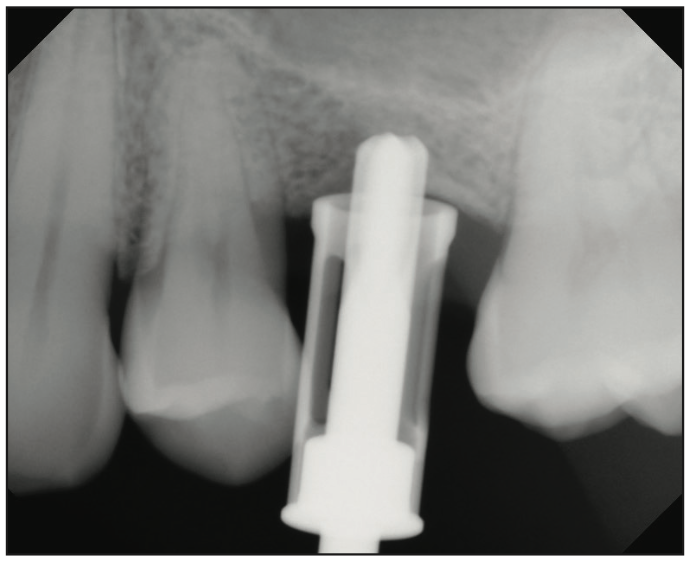
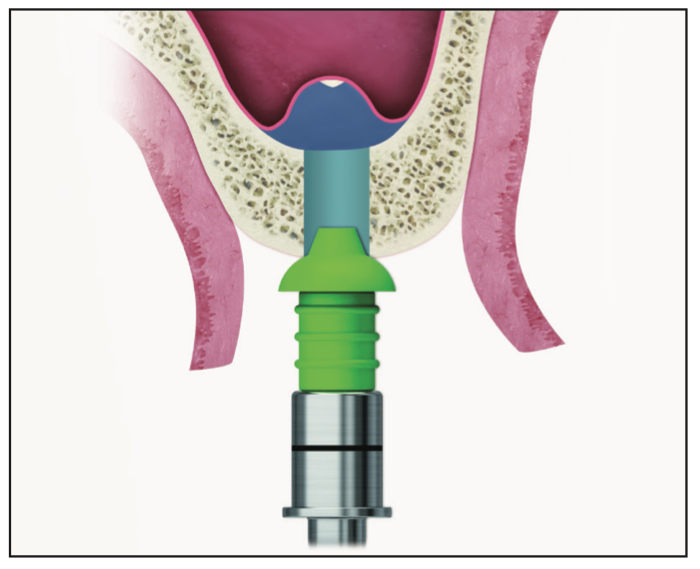
To begin, topical anesthetic was placed at the surgical site, and 4% Septocaine with epinephrine 1:100,000 (Septodont) was given via infiltration. An incision was made using a 15c blade. A periosteal elevator was used to retract the flap, followed by initiation of the osteotomy using a 2-mm guide drill with a 3-mm stopper (Figure 1), keeping it 2 mm away from the sinus cavity. Next, the osteotomy was drilled using a 3.1-mm drill with a 4-mm stopper, followed by a 4.1-mm drill with a 5-mm stopper (Figures 2 and 3). One of the unique features of the CAS Kit bur is that it has an inverted cone design that creates a bone lid, which prevents the Schneiderian membrane from being perforated (Figure 3). After the sinus was lifted, a depth gauge that had an atraumatic tip was used to confirm the membrane lift with a stopper at 5 mm. After confirmation of the membrane lift, a tube attached to a hydraulic lifter containing 1 cm3 or 3 cm3 of saline was used to safely raise the membrane in gradual increments so as to not perforate the membrane (Figure 4).

Figure 5. A bone carrier head with a bone condenser was used to fill the sinus cavity with bone graft material.
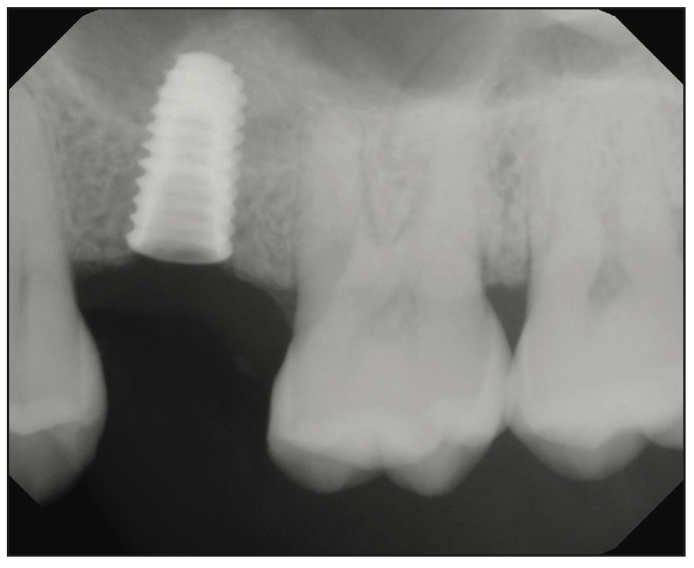
A bone carrier head with bone condenser was used to fill bone graft materials inside the sinus cavity (Figure 5). An x-ray was taken to confirm the sinus lift. The 5- × 8.5-mm implant was placed with 40 Ncm torque value, and sutures were placed (Figures 6 and 7). The patient came back after 4 months for restorations, and the screw-retained crown was delivered. Residual bone height was close to 5 mm; hence, we were successfully able to achieve vertical sinus lift followed by a bone graft without any trauma to the sinus membrane (Figure 8). It was a minimally invasive procedure.
Case 2
An ASA I, 20-year-old girl with a congenitally missing upper right back molar (No. 2) had pain around wisdom tooth No. 1. During the examination, it was discovered that she had an opposing second molar No. 31, and it was slightly supra-erupted due to missing tooth No. 2. The patient expressed concerns with wanting to remove wisdom tooth No. 1 due to pain resulting from pericoronitis (Figure 9).
All treatment options were presented, including the extraction of the wisdom tooth and no treatment due to possible further complications. The patient wanted another molar in the back for better chewing and to prevent supra-eruption of the lower second molar. After discussing with the patient, we devised a plan to extract tooth No. 1 and to place an implant with a sinus lift for tooth No. 2 to increase chewing efficiency and improve overall self-confidence. The sinus was pneumatized, and the residual bone height was approximately 4 mm.
Anesthesia was performed with 2% lidocaine with 1:100,000 epinephrine via infiltration. A subcrestal horizontal incision was made around the area of the first molar to the second molar, and a vertical incision was made on the distal of the first molar. The flap was reflected with the sharp end of the Molt 9 periosteal elevator using a push stroke. After adequate reflection, retraction was much easier with the Seldin elevator. The extraction of tooth No. 1 was done atraumatically. Osteotomy was initiated with a guide drill with a 2-mm stopper for site No. 2, followed by a 2.8-mm drill with a 3-mm stopper. An x-ray was taken to confirm the orientation (Figure 10). Then the final size of drill (3.3 mm) with a 5-mm stopper was used to lift the Schneiderian membrane under copious irrigation. A depth gauge was used with the final size of the stopper to confirm the separation of the membrane without any perforation. The membrane lifter was then used to lift the sinus with saline using a 3-cm3 syringe. OsteOss, a mixture of cortico-cancellous bone, was used to graft the sinus cavity in order to lift the membrane using a bone condenser. A 6- × 8.5-mm implant (ET III NH Implant [Hiossen]) was placed at 35 ncm, and the implant stability quotient was measured at a value of 67 (Figure 11). Finally, a healing cap was placed.

Figure 12. Placement of a healing abutment to support healing of the gingiva and to create emergence profile.
Four months after the implant placement, the patient returned for the restorative phase. A clinical examination showed healthy soft tissue around the implant with an abundance of keratinized tissue. A closed-tray impression coping was used for the final impression. The tooth was restored with a screw-retained solid zirconia abutment, which was chosen over a customized titanium abutment (Figure 12). The radiography showed that the crown and abutment had an adequate fit. The final photo shows natural aesthetics and the harmony of the restoration blending with adjacent tissue (Figure 13).
CONCLUSION
The sinus lift procedure poses many threats to the patient’s health due to the high possibility of perforating the Schneiderian membrane. New and more advanced equipment, such as the CAS Kit, helps to alleviate concerns by facilitating a surgical procedure that is safer in placing implants in the posterior atrophic maxilla while significantly mitigating the chances of perforating the sinus membrane and maintaining sufficient bone generation, providing stable implantation with minimal marginal bone loss. The placement of an implant with equipment such as the CAS Kit provides a better alternative to performing an osteotome procedure, which has proved to be much more time-consuming and has a higher risk of membrane perforation and large amounts of bone loss in the patient.16
REFERENCES
1. Shihab O. Intentional penetration of dental implants into the maxillary sinus: a retrospective study. Zanco J Med Sci. 2017;21:1536–9. doi:10.15218/zjms.2017.001.
2. Summers RB. A new concept in maxillary implant surgery: the osteotome technique. Compendium. 1994;15(2):152, 154–6, 158 passim; quiz 162.
3. Boyne PJ, James RA. Grafting of the maxillary sinus floor with autogenous marrow and bone. J Oral Surg. 1980;38(8):613–6. https://pubmed.ncbi.nlm.nih.gov/6993637
4. Călin C, Petre A, Drafta S. Osteotome-mediated sinus floor elevation: a systematic review and meta-analysis. Int J Oral Maxillofac Implants. 2014;29(3):558–76. doi:10.11607/jomi.3206
5. Stacchi C, Andolsek F, Berton F, et al. Intraoperative complications during sinus floor elevation with lateral approach: a systematic review. Int J Oral Maxillofac Implants. 2017;32(3):e107–18. doi:10.11607/jomi.4884
6. Hernández-Alfaro F, Torradeflot MM, Marti C. Prevalence and management of Schneiderian membrane perforations during sinus-lift procedures. Clin Oral Implants Res. 2008;19(1):91–8. doi:10.1111/j.1600-0501.2007.01372.x
7. Ardekian L, Oved-Peleg E, Mactei EE, et al. The clinical significance of sinus membrane perforation during augmentation of the maxillary sinus. J Oral Maxillofac Surg. 2006;64(2):277–82. doi:10.1016/j.joms.2005.10.031
8. Schwarz L, Schiebel V, Hof M, et al. Risk factors of membrane perforation and postoperative complications in sinus floor elevation surgery: Review of 407 augmentation procedures. J Oral Maxillofac Surg. 2015;73(7):1275–82. doi:10.1016/j.joms.2015.01.039
9. Nolan PJ, Freeman K, Kraut RA. Correlation between Schneiderian membrane perforation and sinus lift graft outcome: a retrospective evaluation of 359 augmented sinus. J Oral Maxillofac Surg. 2014;72(1):47-52. doi:10.1016/j.joms.2013.07.020
10. Al-Moraissi E, Elsharkawy A, Abotaleb B, et al. Does intraoperative perforation of Schneiderian membrane during sinus lift surgery causes an increased the risk of implants failure?: A systematic review and meta regression analysis. Clin Implant Dent Relat Res. 2018;20(5):882–9. doi:10.1111/cid.12660
11. Schwartz-Arad D, Herzberg R, Dolev E. The prevalence of surgical complications of the sinus graft procedure and their impact on implant survival. J Periodontol. 2004;75(4):511-6. doi:10.1902/jop.2004.75.4.511
12. Vlassis JM, Fugazzotto PA. A classification system for sinus membrane perforations during augmentation procedures with options for repair. J Periodontol. 1999;70(6):692–9. doi:10.1902/jop.1999.70.6.692
13. Shende H, Mundada B, Bhola N. Comparative efficacy of osteotome vs CAS kit assisted indirect maxillary sinus lift and immediate implant placement in posterior atrophic maxilla—a study protocol. J Pharm Res Int. 2021;33(63A):183–8. doi:10.9734/jpri/2021/v33i63A35232
14. Kim YK, Ku JK. Sinus membrane elevation and implant placement. J Korean Assoc Oral Maxillofac Surg. 2020;46(4):292–8. doi:10.5125/jkaoms.2020.46.4.292
15. Timmenga NM, Raghoebar GM, van Weissenbruch R, et al. Maxillary sinus floor elevation surgery. A clinical, radiographic and endoscopic evaluation. Clin Oral Implants Res. 2003;14(3):322–8. doi:10.1034/j.1600-0501.2003.140310.x
16. Kim YW, Keum YS, Son HJ, et al. Predictability of simultaneous implant placement with sinus floor elevation in the severely atrophic posterior maxillae; comparison of lateral and trans-crestal approaches. J Korean Dent Assoc. 2010;48:205–17.
ABOUT THE AUTHOR
Dr. Patel graduated from Temple University’s prestigious oral surgery host program as an honors student and earned an excellence award in the field of cosmetic dentistry over the course of his successful practice in general dentistry. He is an active member of the Chicago Dental Society, the ADA, and the International Congress of Oral Implantologists (ICOI). Dr. Patel is a Fellow and a Diplomate in Oral Implantology of the ICOI and the American Association of Implant Prosthetics. He is also a world-renowned faculty member and course director for Hiossen. He can be reached at connectbrijesh87@gmail.com.
Disclosure: Dr. Patel is a course director for AIC, Hiossen Implant’s research and education center, and receives compensation for lectures.