INTRODUCTION
The introduction of cone-beam computed tomography (CBCT) scanners for the oral and maxillofacial region in the late 1990s has revolutionized dentistry. CBCT technology provides a 3D view of anatomical structures in the head and neck area, making it the preferred modality for diagnosis and treatment planning in many dental tasks. Its clinical applications range from dental implants, endodontics, airway and TMJ analysis, to the diagnosis of jaw lesions and advanced surgical procedures. The clinician’s professional judgment in selecting the imaging modality types, including intraoral, panoramic, CBCT, or a combination of them, could play an essential role in timely diagnosis and management of pathological conditions of the jaws.1
While the CBCT scan provides valuable information about the task at hand, it may also reveal incidental findings. These findings range from benign soft-tissue calcifications and idiopathic sclerosis of the jaw bones to more significant abnormalities, such as cystic or neoplastic (tumoral) lesions, inflammatory and fibro-osseous conditions, and radiographic bone changes related to systemic diseases. This information may not be the primary intent of the CBCT exam. Still, it should not be overlooked since it may provide valuable information with high clinical significance regarding a patient’s oral and overall health.
In dental imaging, a practitioner could be prone to focusing on his or her area of interest, which is the specific area that is being further evaluated in 3D, and he or she is also likely to detect well-demarcated jaw lesions at a higher rate. On the other hand, poorly demarcated lesions with blending or diffuse borders may present a diagnostic challenge. This is especially important since multiple pathologies, such as fibro-osseous lesions, osteomyelitis, medically related osteonecrosis of the jaws, or malignant neoplastic processes, share some overlapping radiographic presentations. Thus, evaluating CBCT scans requires a methodical and systematic assessment of the entire scan in axial, sagittal, and coronal planes. Each of the lesion’s radiographic characteristics needs to be carefully noted and given value in providing information about the abnormality’s nature. In the following radiographs, we will review some of the information that could be gathered based on a lesion’s radiographic presentation.
The location of the lesion(s) and their relation to the mandibular canal, above (Figure 1), within (Figure 2),2 or below (Figure 3), could suggest that the pathology could be more likely odontogenic, of neural or vascular origin, or non-odontogenic, respectively.
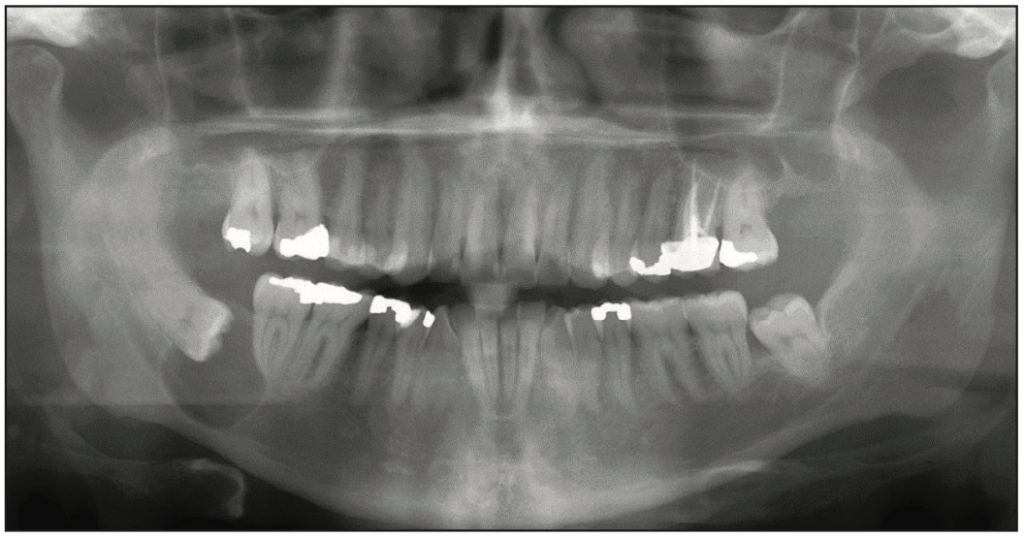
Figure 1. Well-demarcated, corticated radiolucency above the right mandibular canal associated with the crown of impacted No. 32 was suggestive of an odontogenic process. Histologic diagnosis was of a dentigerous cyst.
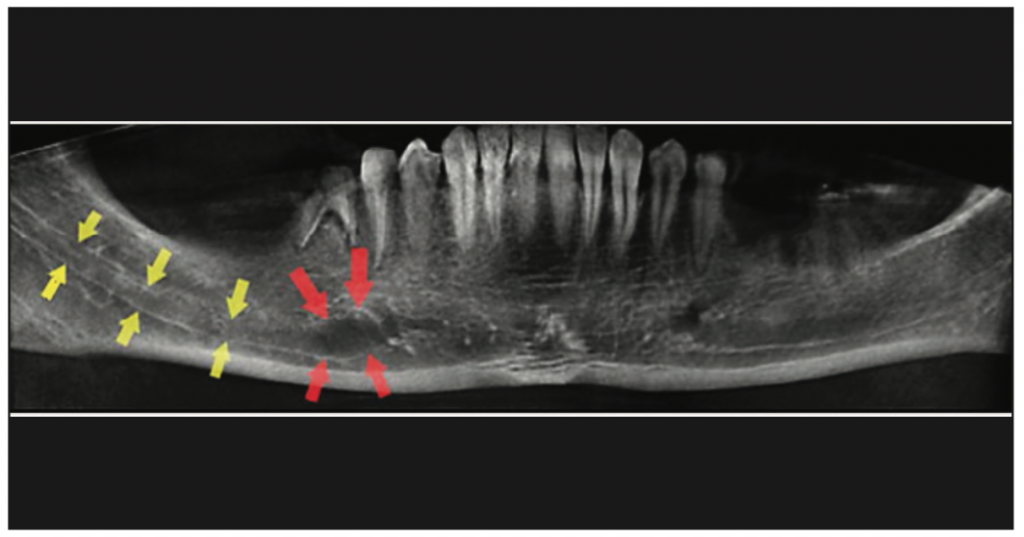
Figure 2. Well-demarcated radiolucency within the boundaries of the right mandibular canal was suggestive of a lesion with neural or vascular origin. The confirmed diagnosis was neurofibroma.
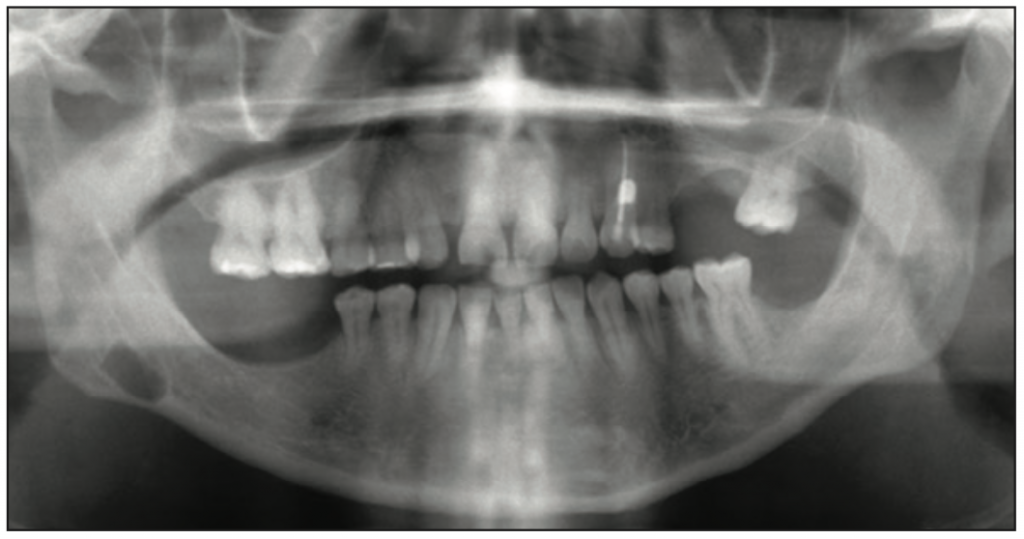
Figure 3. Well-demarcated, corticated radiolucency inferior to the right mandibular canal was consistent with the non-odontogenic entity Stafne bone defect.
The number of lesions: Most jaw lesions present as a single entity. Yet, in cases where 2 or more lesions are present, clinical correlation with the patient’s health history could be beneficial in ruling in or out the possibility of the patient having other inclusion criteria for a specific syndrome. One example is in individuals who present with multiple odontogenic keratocysts (OKCs) in their jaws (Figure 4). Clinical signs, such as hypertelorism, deep plantar pits, intracranial ectopic calcifications, and facial dysmorphism, can also be evident. These findings of multiple OKCs and cutaneous, skeletal, ocular, and neurologic abnormalities are usually associated with nevoid basal cell carcinoma syndrome, also known as Gorlin syndrome, a hereditary condition characterized by a wide range of developmental abnormalities and a predisposition to neoplasms, specifically basal cell carcinoma of the skin.3
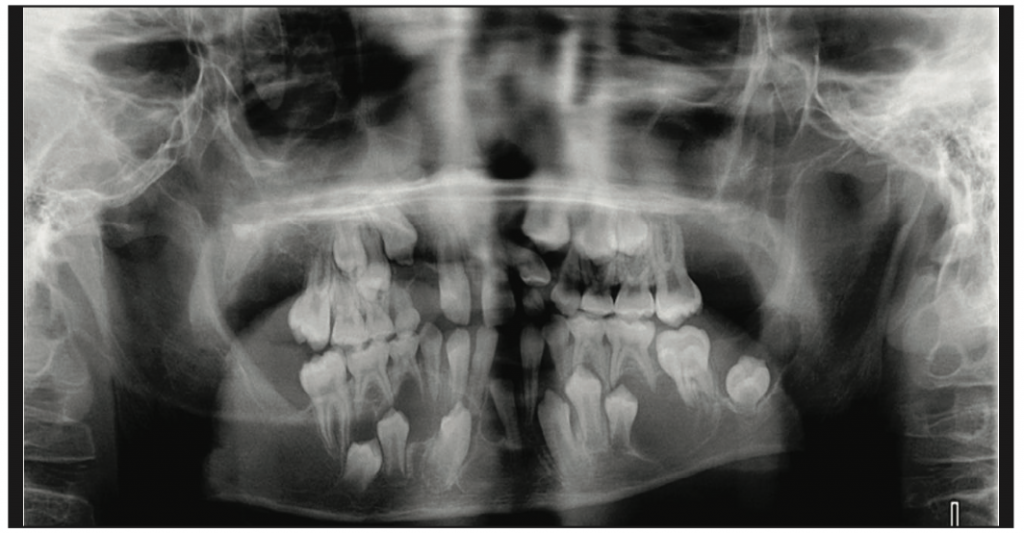
Figure 4. Multiple well-demarcated, corticated radiolucent lesions in the right maxilla, right mandible, and crossing the midline were noted. Histologic diagnosis was multiple odontogenic keratocysts.
Periphery of the lesion: Boundaries (well-demarcated, ill-demarcated, or blending borders); cortication or lack thereof; internal density (radiolucent, radiolucent or mixed density); expansion (cystic vs tumoral); and the lesion’s effects on surrounding structures (resorption of bone, PDL, and teeth), tooth displacement, and periosteal reactions need careful evaluation as well. The following 2 cases highlight how the above-mentioned radiographic features are utilized in generating a differential diagnosis and the tremendous value of a multidisciplinary approach to care when identifying jaw abnormalities.
After assessing the above parameters, a “diagnostic impression” about the lesion’s possible nature (benign, malignant, developmental, or self-limiting) and origin (odontogenic/non-odontogenic) is formed. This impression serves as the basis for generating a differential diagnosis that directs the next steps. The suggested following actions could range from watchful waiting and radiographic re-evaluation of the area to immediate treatment; referral to a specific dental specialty; biopsy; or referral for further imaging, such as an MRI or a medical CT.
CASE REPORTS
Case 1
A 42-year-old female with a history of bisphosphonate use for a duration of 8 years was referred to WesternU Patient Care Center for evaluation of a white soft-tissue lesion on the lateral border of her tongue. Panoramic imaging was acquired as part of the new-patient assessment.
Radiographic Findings
At the initial evaluation stage, panoramic and periapical radiographs were acquired. Radiographic findings (Figures 5 and 6) of irregular interdental and periapical radiolucency and periodontal ligament (PDL) space widening associated with teeth Nos. 26, 27, and 28 were noted. Since the radiographic appearance of irregular PDL widening did not resemble a lesion with odontogenic (endodontic) etiology (which is usually centered at and around the tooth’s apical exit), a decision was made to take a CBCT scan and evaluate the lesion’s effect and extension within the mandible.1
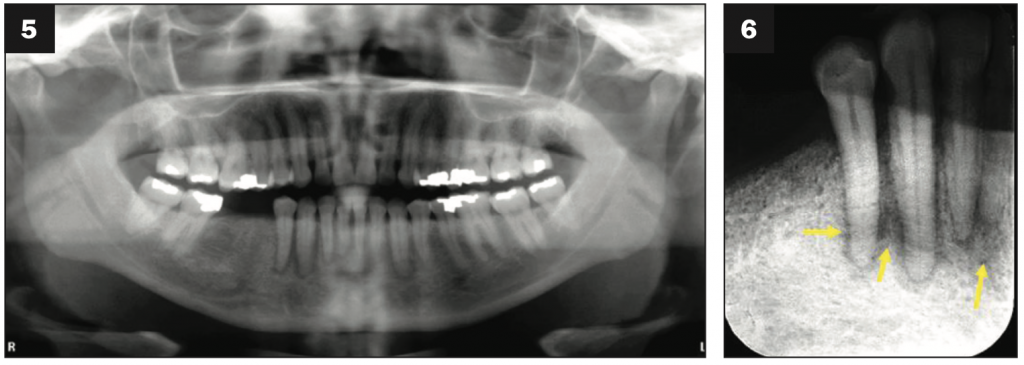
Figures 5 and 6. Panoramic and periapical radiographs showed the loss of bone support and irregular widening of the PDL associated with Nos. 26, 27, and 28—mott-eaten bone appearance.
CBCT findings (Figures 7 to 9) included multiple areas with permeative changes (small 1- to 3-mm radiolucencies) and interruption of buccal and lingual plates in the mandible with no sign of cortical expansion.
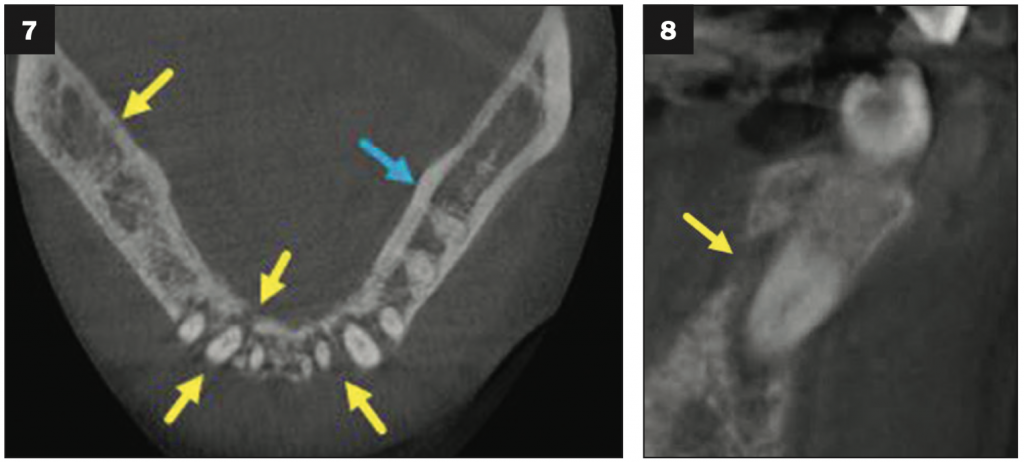
Figures 7 and 8. Axial and cross section views of the CBCT showed multiple areas of interrup- tion of buccal and lingual plates of the mandible with no sign of expansion.
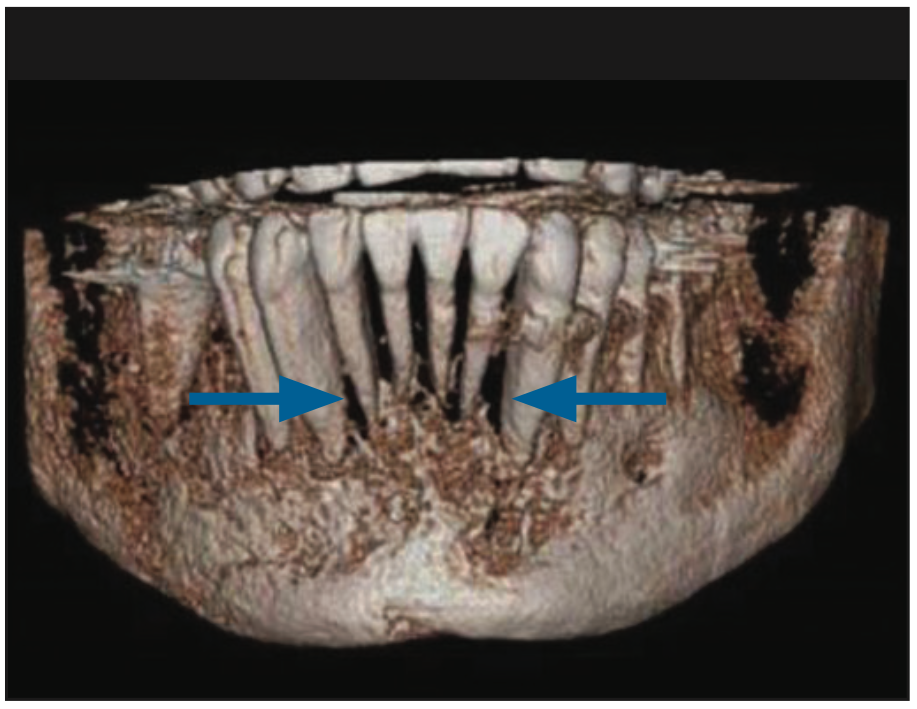
Figure 9. A 3D volume rendering from CBCT volume of the anterior mandible.
Irregular PDL widening, loss of lamina dura, and interruption of the cortices without expansion could be found in association with generalized malignancies such as leukemia, multiple myeloma, and non-Hodgkin’s lymphoma infiltrates. Also, metastatic disease, where malignant cells travel through the bloodstream, can randomly infiltrate the bone in a generalized manner. Those infiltrates can be transported to different parts of the PDL space and cause irregular PDL widening, resorption of lamina dura, and bone loss. Considering the radiographic and clinical findings mentioned above, a decision for a biopsy referral was made (completed by Dr. Jeffery Elo, oral surgeon, WesternU Dental Center). The final diagnosis based on the histopathological findings (Figure 10) was metastatic breast carcinoma invading the mandible.
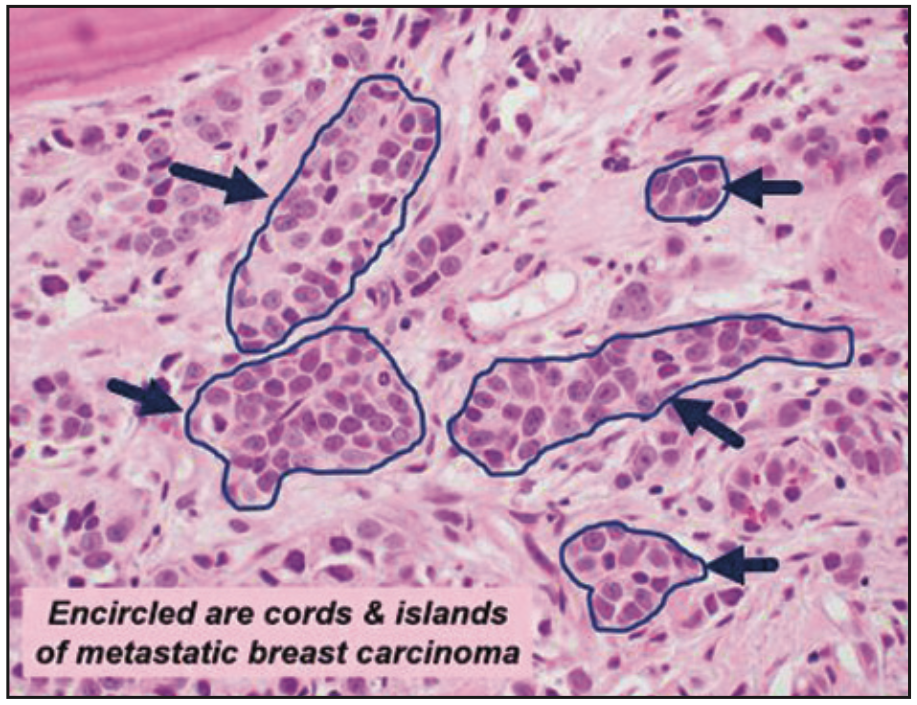
Figure 10. Histologic findings of cords and islands of metastatic breast carcinoma.
Case 2
A 25-year-old female with no contributing medical history presented to WesternU Patient Care Center for teeth cleaning in January 2019. Clinical examination of teeth Nos. 26 to 29 tested vital and positive to percussion and intermittent pain in the area.
Radiographic Findings
In the recent periapical radiograph in 2019 (Figure 11, right), areas of loss of lamina dura and irregular PDL space widening at the distal aspect of No. 27 and mesial and distal apical aspects of No. 26 were noted. The border of the lesion appeared irregular with no notable cortication. A wide region of intermediate density called the “transition zone” (the area between the totally radiolucent region of the lesion and the normal-appearing bone) is present. No tooth resorption was noted. A comparison of periapical radiographs from June 2018 and January 2019 suggested a rather significant amount of bone destruction in this period (Figures 11 and 12).
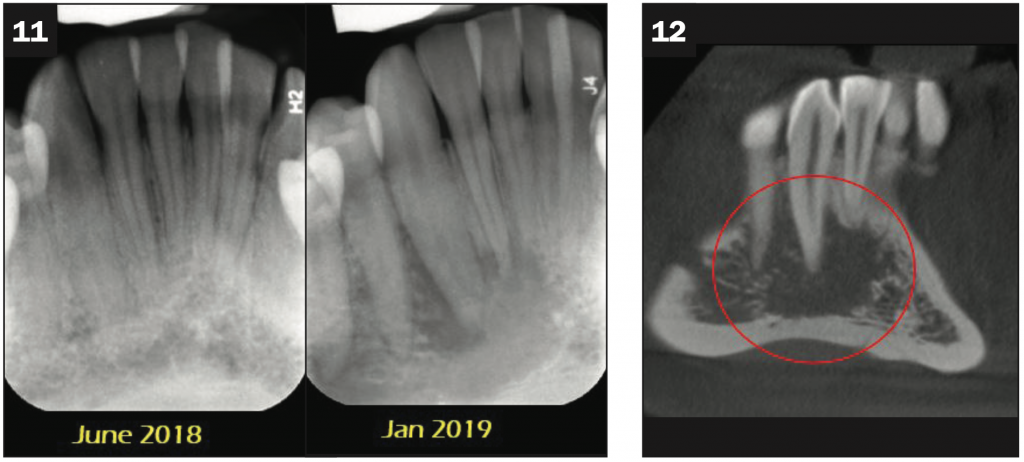
Figures 11 and 12. (Figure 11, left) No radiographic sign of a resorptive lesion in No. 26 or 27 was noted. (Figure 11, right, and Figure 12 [coronal CBCT]) Areas of loss of lamina dura and irregular PDL space widening at the distal aspect of No. 27 and mesial and distal apical aspects of No. 26 were noted. A wide transition zone was present.
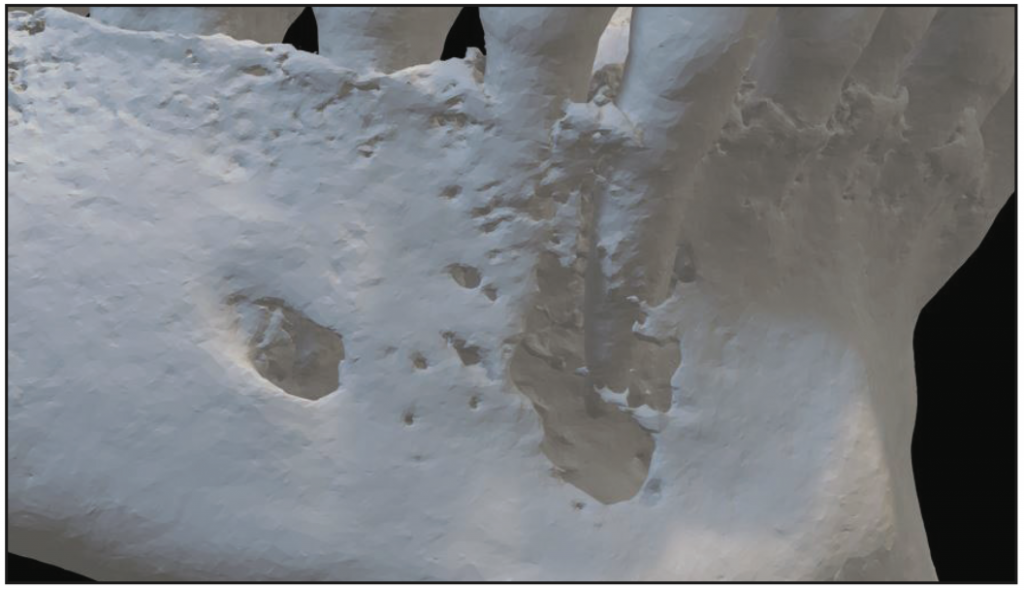
Figure 13. A 3D volume rendering from CBCT volume.
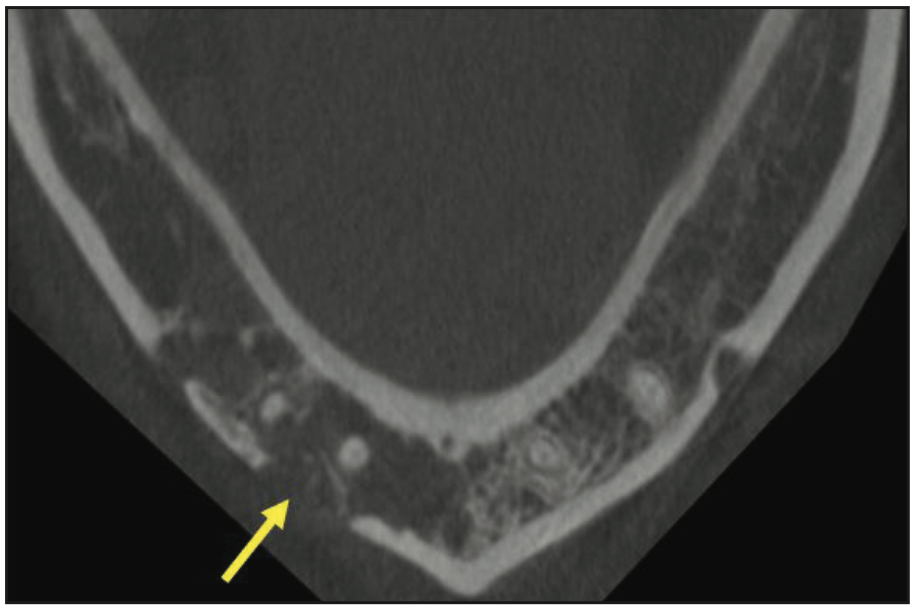
Figure 14. Axial view CBCT showed localized interruption of buccal cortical plate in the area of Nos. 26 and 27; no expansion was noted.
In the 3D volume rendering of the CBCT (Figure 13) residual floating spicules of trabecular bone and irregular borders of the lesion were present. The lesion appeared to have larger dimensions compared to what was visualized in the PA radiograph. The axial view of the CBCT (Figure 14) demonstrated a localized area of interruption of buccal cortical plate at the region of No. 27. In cross-sectional presentation of the CBCT (Figure 15), significant destruction of the buccal cortical plate was noted in the area of Nos. 26 and 27 with no sign of bone expansion or periosteal reaction.
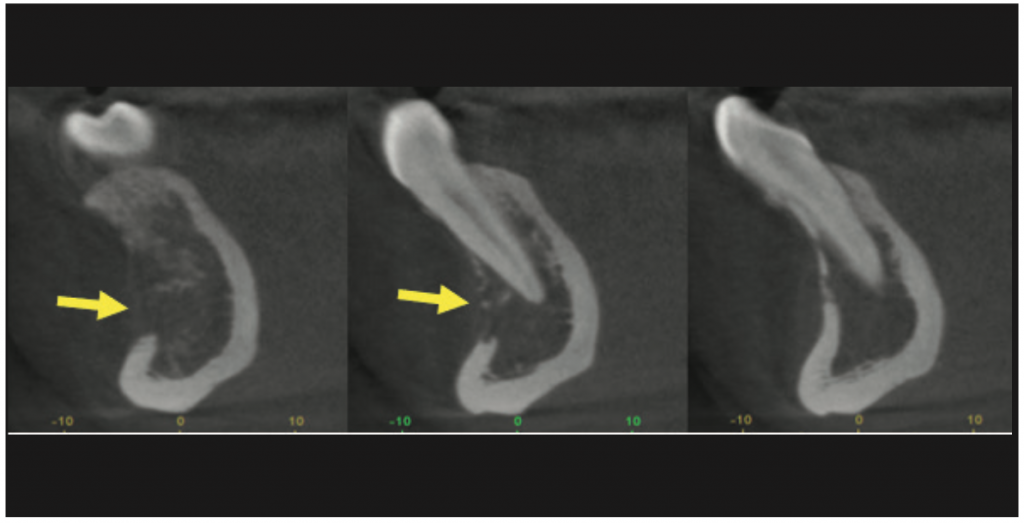
Figure 15. Cross section CBCT showed an interruption of the buccal cortical plate with no expansion.
Considering the radiographic and clinical findings mentioned above, a decision for biopsy referral was made (completed by Dr. Elo). The final diagnosis based on the histopathological findings was diffuse large ß-cell lymphoma.4 The specimen was evaluated by Dr. Mark Mintline, director of the Oral Pathology Lab, WesternU College of Dental Medicine.
CONCLUSION
CBCT technology can be a valuable tool in the diagnostic process for identifying jaw abnormalities. However, dentists who use CBCT technology must have appropriate training in evaluating normal maxillofacial structures in 3D and be competent in identifying potential pathologic findings in CBCT scans. The topic of practitioners’ responsibility in diagnosing and reporting on any abnormality present within the acquired CBCT scan area, even if that finding is beyond his or her scope of knowledge or radiology training, is related to a generalized health condition manifested in the jaws, or is unrelated to the initial intent of the scan, has been discussed extensively and published. In the executive opinion statement published in 2008 on performing and interpreting diagnostic CBCT by the American Academy of Oral and Maxillofacial Radiology,5 the standard under “Practitioners’ responsibility” states that “The responsibility of interpreting the findings of the CBCT images lies with the practitioner who obtains them, and an imaging report should accompany the scan, similar to how a biopsy requires a report.” The standard also mentions that it is essential to note that dentists who use CBCT technology should meet the same standards as board-certified oral and maxillofacial radiologists (OMFRs).
It is essential to recognize that CBCT scans are just one piece of the diagnostic puzzle mostly related to evaluating hard-tissue structures (teeth and bone) with minimal soft-tissue contrast resolution. For this reason, there must be an effective collaboration between multiple diagnostic specialties to accurately assess the hard- and soft-tissue abnormalities and their possible overlap, including oral radiology, oral pathology, oral surgery, and oral medicine.
To streamline the oral diagnosis process, more work must be done to create HIPAA-compliant communication infrastructures that could facilitate a harmonious workflow between diagnostic specialties. By working together and ensuring that dentists who utilize CBCT imaging have the appropriate training and competency in interpreting the CBCT scans as well as having access to expert consultation from qualified oral and maxillofacial radiologists in the form of radiology reports, we can improve the accuracy and efficiency of the diagnostic process and ultimately provide better care for our patients.
REFERENCES
1. Lavasani S. Oral and maxillofacial radiology diagnosis: the role of image modality selection, interpretation skills and use of cone beam computed tomography technology. CDA Journal. 2022.
2. Mortazavi H, Baharvand M, Safi Y, et al. Common conditions associated with mandibular canal widening. A literature review. Imaging Sci Dent. 2019. Jun;49(2):87-95. doi:10.5624/isd.2019.49.2.87
3. Lo Muzio, L. Nevoid basal cell carcinoma syndrome (Gorlin syndrome). Orphanet J Rare Dis 3, 32 (2008). https://doi.org/10.1186/1750-1172-3-32
4. Mintline M, Elo JA, Lavasani S, et al. The synergistic role of 2D and 3D imaging in evaluating tumors of the jaws: a case report of diffuse large B-cell lymphoma of the mandible. J Calif Dent Assoc. 2022;50(9):519–25. doi:10.1080/19424396.2022.12224337
5. Carter L, Farman AG, Geist J, et al. American Academy of Oral and Maxillofacial Radiology. American Academy of Oral and Maxillofacial Radiology executive opinion statement on performing and interpreting diagnostic cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106(4):561–2. doi:10.1016/j.tripleo.2008.07.007
ABOUT THE AUTHOR
Dr. Lavasani is a board-certified oral and maxillofacial radiologist and an associate professor and the director of oral radiology and advanced imaging at Western University of Health Sciences, College of Dental Medicine in Pomona, Calif. She is a Diplomate of the American Board of Oral and Maxillofacial Radiology and maintains an active dental imaging practice at Western University Patient Care Center’s 3D CBCT Imaging Lab and Interpretation Center. She serves as the national oral radiology advisor on the board of General Dentistry, the peer-reviewed journal of the AGD. With numerous lectures, hands-on courses, and book chapters published, she is an internationally recognized voice in the field of 3D radiographic diagnosis, applications of CBCT in dentistry, and topics related to radiation dose and biological effects of ionizing radiation on tissues. Dr. Lavasani is the founder of the California Academy of Oral Radiology where she provides on-demand and customized educational activities, seminars, and hands-on CBCT courses for dentists and DSOs. Dr. Lavasani serves as a member of the board of directors at the Tri-county Dental Society (TCDS) and is a voting delegate representing the TCDS at the California Dental Association House of Delegates. She can be reached at slavasani@westernu.edu or via the Instagram handle @slavasanidds.
Disclosure: Dr. Lavasani reports no disclosures.












