Researchers from both Rensselaer Polytechnic Institute and Texas A&M University are developing a material that can be used to replace skull bone lost to injury, surgery, or birth defects. It also has potential for use in repairing jawbone that has been lost or damaged due to periodontitis, oral cancer, and other issues.
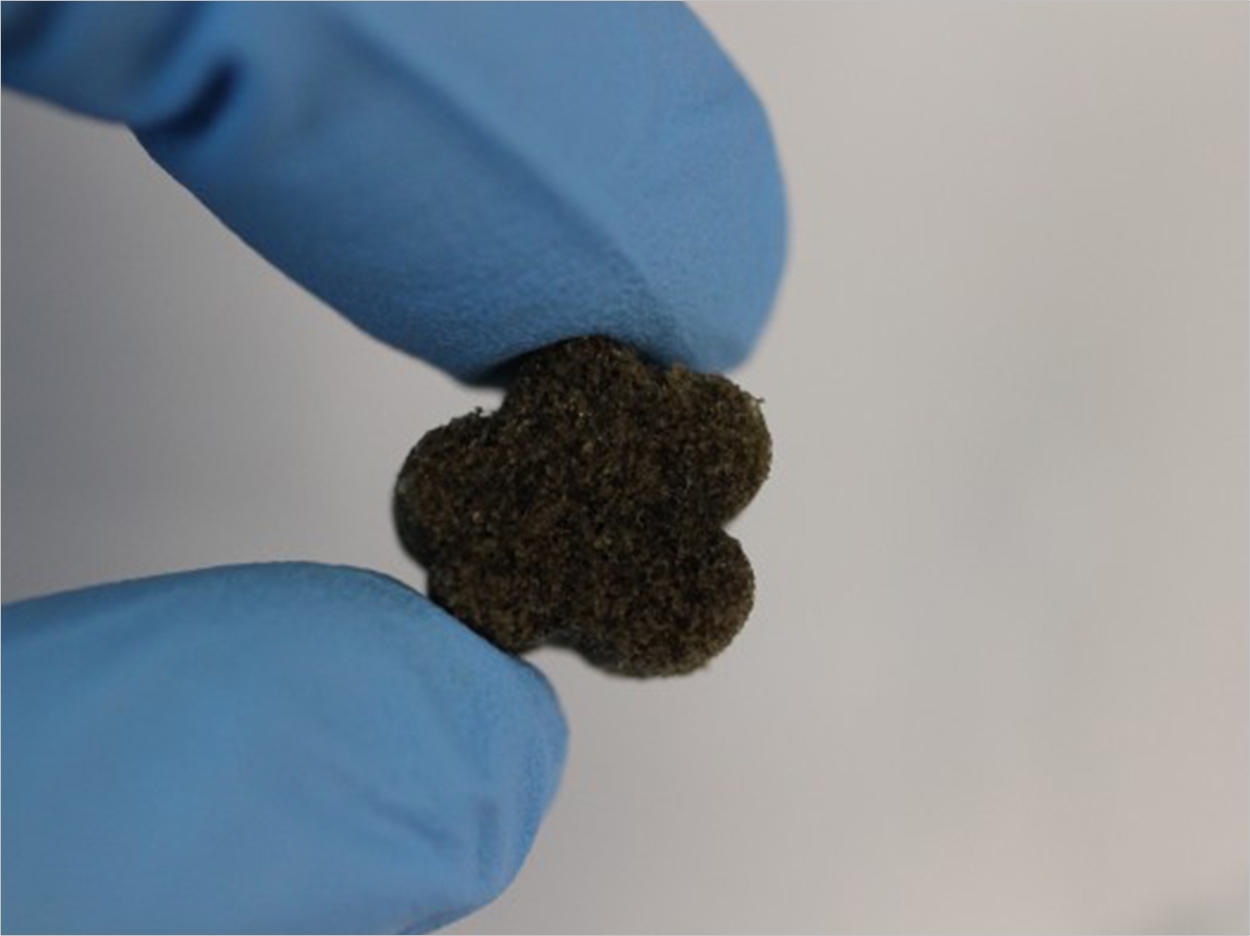
The bioactive foam is malleable when exposed to warm saline, like a sponge, allowing surgeons to easily shape it to fit irregular defects in the bone, where it hardens in place. Once implanted, specially coated pores within the foam attract bone cells, naturally regenerating bone to replace the foam, which dissolves with time.
“Depending on the size of the jaw defect, this material has potential use in jaw repair applications,” said Mariah Hahn, PhD, MS, a member of Rensselaer’s Center for Biotechnology and Interdisciplinary Studies. “If a large segment of jaw were removed (eg, several centimeters), however, this material would need physical support until healing occurred and healing may be less effective, particularly in the central regions of the graft.”
The foam, a shape memory polymer coated in a bioactive polydopamine, is intended as an alternative to materials currently used to treat cranio-maxillofacial gaps. Most commonly, such gaps are filled with a bone graft surgically harvested from the patient’s hip or elsewhere in the body. Such rigid bone grafts are often difficult to harvest and cannot be readily manipulated to fit within irregularly shaped bone defects, compromising healing.
“This is like trying to fill in a missing puzzle piece with the wrong piece,” said Melissa Grunlan, PhD, MS, an associate professor at Texas A&M University who developed the foam. “These bone defects can cause tremendous functional problems and aesthetic issues for individuals, so it was recognized that a better treatment would make a big impact.”
Hahn will test various formulations of the foam in vitro, recommending the most successful formulations for further preclinical testing and providing insights on why some foams are more or less successful in promoting bone growth.
“We want to find the ideal formulation that maintains the amazing shape memory properties of the foam while providing the optimal environment for stimulating new bone formation,” said Hahn.
The research draws upon Hahn’s expertise in bone formation and bone tissue engineering in evaluating the materials and proposing next steps to optimize the formulations. Hahn’s work focuses on understanding cell-to-cell and cell-to-material interactions at a fundamental level. The Hahn Tissue Lab specializes in the development of tissue-engineered replacements for diseases small-caliber arteries and osteochondral tissues as well as the regeneration of chronically scarred tissue. It also is involved in the development of tissue-engineered disease models.
The project began about 5 years ago, and the researchers say it already has shown good biocompatibility in preliminary tests in small animal models. Many more years of refinement and testing are required before a product reaches surgeons as a treatment option. However, Hahn said, the approach has a number of advantages, particularly compared to other options now being researched, such as 3-D printing.
“A moldable bone-promoting scaffold could have broad use if it’s successful,” said Hahn. “It takes advantage of the body’s own healing ability, and it’s a low-cost, off-the-shelf solution that would not need to be pretailored to the individual defect.”
Related Articles
Protein Combination Improves Bone Regeneration
Living Bone Grown for Facial Reconstruction
Plastic Mixed with Bone Powder for 3-D Printed Replacement Bones












