As oral health practitioners, one of the most important services that we must provide for our patients is treatment rendered with as little pain and discomfort as possible. There is also the important responsibility that requires us to remain up-to-date with the standard of care in all disciplines of our practice, whether it is using reliable restorative materials or effective and safe anesthesia. We must also continuously challenge ourselves to strive for the best result in everything that we do for our patients. However, dentists routinely find themselves in situations that call for creativity in order to achieve 100% success. This is true for all aspects of dentistry, including the use of local anesthesia. This lofty goal of 100% success remains somewhat elusive. While the constant battle for perfection can be stressful, striving for perfection every time can be the golden key to happiness and satisfaction within the profession of dentistry. Additionally, learning new techniques, trying new products, and having fun in the process can be very rewarding and beneficial for our patients. This article will discuss the use of an intraosseous local anesthetic delivery system that can be used routinely, and also in situations when a patient is difficult to anesthetize.
 |
 |
|
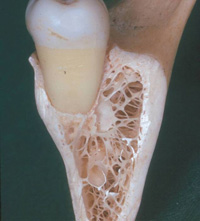
Figure 1. Cancellous bone in which the trabeculae of bone and all the space that exists between them can be seen. |
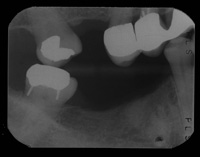
Figure 2. A bite-wing radiograph of the lower right quadrant. Notice the large area of cancellous space mesial to the molar. In addition, a retained root tip can be seen just distal to the premolar. This is an example of an anatomical anomaly that one must uncover before performing a perforation highlighting the importance of taking a preinjection radiograph. |
 |
 |
|
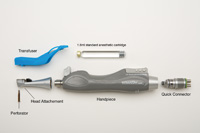
Figure 3a and 3b. One example of an intraosseous injection (IOI system (IntraFlow [Pro-Dex]). These photos show the device unassembled and assembled for use. |
 |
 |
|
Figure 4. The IOI device (IntraFlow) in position to perforate through the buccal plate of bone. The perforator is roughly perpendicular to the surface of the cortex and slightly pointing apically. This ensures that the perforator will travel where the operator wishes it to and not towards any root surfaces in the area. |
Figure 5. The IOI device (IntraFlow) has perforated the buccal cortex and is inside the cancellous space. The operator now removes their foot from the rheostat to stop the perforator from rotating. This device will automatically switch to injection mode and the operator can now lightly step on the rheostat for a second time, and the device will inject solution. |
 |
 |
|
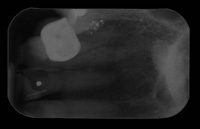
Figure 6. A radiograph showing adequate cancellous bone between the lateral and central incisor. |
Figure 7. The IOI device (IntraFlow) is in correct position and ready to perforate the cortex between the 2 teeth being treated. |
 |
| Figure 8. The needle has just perforated through the cortex of bone and is sitting within the cancellous space. Local anesthetic can now be injected as previously described. |
Next, a preparatory infiltration of approximately 0.3 ml of local anesthetic was slowly injected into the same buccal fold area. This was painless due to previous placement of the topical anesthetic, and because such a small volume creates little sensation from tissue expansion. An anesthetic with 1:100,000 epinephrine was chosen in order to achieve vasoconstriction and to avoid a small amount of bleeding that might occur following perforation. This injection ensured a painless perforation.
The IntraFlow handpiece system was then assembled (Figures 3a and 3b) and readied for use. The perforation site was within attached gingiva, just coronal to the mucogingival line (Figure 4). The rheostat was depressed at full speed (on the slow-speed line), and the perforator was pushed through the gingiva, cortex, and into the cancellous space with gentle pressure. When the cancellous space is entered, the resistance to push while perforating disappears and the perforator “pops” through the cortex (Figure 5). At this point, the foot is released from the rheostat. It should take no more than 3 to 4 seconds to perforate. There are situations where one may not feel that resistance disappear. This happens most commonly in the posterior mandible where the buccal plate of bone is thickest. In this situation, the operator must choose a different injection method since continually pressing on the cortex without perforating it can lead to heat buildup and the possibility of localized bony necrosis.
Next, to carry out the injection, the rheostat was depressed again, this time more lightly. 0.9 ml of local anesthetic (half a cartridge) was then slowly injected over a period of approximately 45 seconds. A solution containing 1:200,000 epinephrine was chosen for this procedure to limit heart palpitations and to maximize duration. The standard is to use this volume to achieve pulpal anesthesia for one tooth on either side of the perforation. If the operator decides to work in another area, there is enough volume to anesthetize 2 other teeth with a second perforation. One should not exceed one (full) cartridge of anesthetic per appointment due to the rapid uptake of the vasoconstrictor from the cancellous space and the risk of obtaining palpitations. The patient was warned about palpitations using the following calm language: “You might feel your heart racing a little bit. This will go away in a few seconds. It is a good sign that the anesthetic is in the right place.”
The dentistry was completed and the patient felt no pain or sensitivity during the injection or during the 45-minute treatment procedure.
CASE REPORT 2
A 67-year-old female was being treated for a crown and bridge prosthesis on her maxillary right lateral and central incisors (teeth Nos. 7 and 8). First, a preoperative radiograph was taken (Figure 6). This image showed a large amount of cancellous bone between the 2 teeth being treated. During the insertion phase of the treatment, it was decided that an IOI using the IntraFlow device would be used to provide pulpal anesthesia to closely match the duration of treatment. With this technique, the smile line can be more accurately assessed when anterior prosthetics are planned and tried in with no lip distortion present.
Next, topical anesthesia followed by a preparatory injection of 0.3 ml local anesthetic was slowly infiltrated into the mucobuccal fold between the central and lateral. Figure 7 shows the initial positioning of the IntraFlow handpiece before injection. Notice that the perforator is placed at the mucogingival line pointing slightly apically, sitting between the lateral and central incisor. In Figure 8, the needle has perforated the cortex and is now sitting inside the cancellous bone. The operator now can begin the injection phase using the methods described above.
Treatment began immediately after injection with the removal of the temporaries, followed by the try-in and finally the insertion of the new crowns. Treatment time took 25 minutes and the patient had no discomfort throughout the procedure.
CONCLUSION
This article has briefly reviewed the history of intraosseous anesthesia and presented 2 case reports describing how IOIs were successfully used. Studies demonstrating that the intraosseous delivery of local anesthetic has been shown to be an effective method of achieving pulpal anesthesia have been cited in this article. This technique has been available for many years via different systems. The author has found that the IOI method for achieving profound local anesthesia to be useful not only as a primary injection, but also in cases where supplementary anesthesia is required due to the failure of the standard techniques. In addition he has found that IOI devices, such as the IntraFlow (Prodex), are also easy to use and well-accepted by patients.
References
- Masselink BH. The advent of painless dentistry. Dent Cosmos. 1910;52:868-872.
- Dental Products Report Survey, Nov 2006.
- Brown R. Intraosseous anesthesia: a review. J Calif Dent Assoc. 1999;27:785-792.
- Reisman D, Reader A, Nist R, et al. Anesthetic efficacy of the supplemental intraosseous injection of 3% mepivacaine in irreversible pulpitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84:676-682.
- Dunbar D, Reader A, Nist R, et al. Anesthetic efficacy of the intraosseous injection after an inferior alveolar nerve block. J Endod. 1996;22:481-486.
- Replogle K, Reader A, Nist R, et al. Anesthetic efficacy of the intraosseous injection of 2% lidocaine (1:100,000 epinephrine) and 3% mepivacaine in mandibular first molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:30-37.
- Parente SA, Anderson RW, Herman WW, et al. Anesthetic efficacy of the supplemental intraosse-ous injection for teeth with irreversible pulpitis. J Endod. 1998;24:826-828.
- Nusstein J, Reader A, Nist R, et al. Anesthetic efficacy of the supplemental intraosseous injection of 2% lidocaine with 1:100,000 epinephrine in irreversible pulpitis. J Endod. 1998;24:487-491.
- Coury KA. Achieving profound anesthesia using the intraosseous technique. Tex Dent J. 1997;114:34-39.
- Gallatin J, Reader A, Nusstein J, et al. A comparison of two intraosseous anesthetic techniques in mandibular posterior teeth. J Am Dent Assoc. 2003;134:1476-1484.
- Coggins R, Reader A, Nist R. Anesthetic efficacy of the intraosseous injection in maxillary and mandibular teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;81:634-641.
- Bigby J, Reader A, Nusstein J, et al. Articaine for supplemental intraosseous anesthesia in patients with irreversible pulpitis. J Endod. 2006;32:1044-1047.
- Prohic S, Sulejmanagic H, Secic S. The efficacy of supplemental intraosseous anesthesia after insufficient mandibular block. Bosn J Basic Med Sci. 2005;5:57-60.
- Nusstein J, Wood M, Reader A, et al. Comparison of the degree of pulpal anesthesia achieved with the intraosseous injection and infiltration injection using 2% lidocaine with 1:100,000 epinephrine. Gen Dent. 2005;53:50-53.
- Wood M, Reader A, Nusstein J, et al. Comparison of intraosseous and infiltration injections for venous lidocaine blood concentrations and heart rate changes after injection of 2% lidocaine with 1:100,000 epinephrine. J Endod. 2005;31:435-438.
- Stabile P, Reader A, Gallatin E, et al. Anesthetic efficacy and heart rate effects of the intraosseous injection of 1.5% etidocaine (1:200,000 epinephrine) after an inferior alveolar nerve block. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:407-411.
- Chamberlain TM, Davis RD, Murchison DF, et al. Systemic effects of an intraosseous injection of 2% lidocaine with 1:100,000 epinephrine. Gen Dent. 2000;48:299-302.
- Jeske AH. Local anesthetics: special considerations in endodontics. J Tenn Dent Assoc. 2003;83:14-18.
- Replogle K, Reader A, Nist R, et al. Cardiovascular effects of intraosseous injections of 2 percent lidocaine with 1:100,000 epinephrine and 3 percent mepivacaine. J Am Dent Assoc. 1999;130:649-657.
Dr. Isen’s dental clinic in Toronto is anesthesia-based, focusing on treating patients with special needs and dental phobia. He is past president of the Ontario Dental Society of Anesthesia and he lectures for the University of Western Ontario’s CE program and the University of Toronto Faculty of Dentistry. In addition, he has lectured internationally on topics related to local anesthesia and medical emergencies. He has acted as a consultant for numerous dental and pharmaceutical companies and serves as a peer reviewer. He can be reached at (416) 498-8484 or d.isen@rogers.com.
Disclosure: Dr. Isen has no financial interest in any company mentioned in this article.











