With advancements in communication, the world has become a much smaller place. Through the use of cell phones, the Internet, and e-mail, one can easily communicate and consult with anyone, anytime throughout the world. These technologies offer great benefits, especially in the medical and dental fields. Doctors and patients not only use these tools for communication, but also as a means to transfer views and opinions. Despite these benefits, though, the aforementioned technological advancements have also brought forth many unforeseen problems. One of the latest and fastest-growing businesses in healthcare is medical/dental tourism. This is defined as the act of traveling to foreign, often underdeveloped countries to obtain medical, dental, and surgical care.1
The medical tourism market is estimated to grow by $2.2 billion, with a corresponding increase of $60 billion in the global healthcare market.2 A combination of various factors, such as the high cost of healthcare in industrialized nations, the increased ease of international travel, favorable currency exchange rates in the global economy, rapidly improving medical technology, the Internet, and the standard of care in many countries, have led to the recent increase in its popularity.3
In the case report that follows, a patient of record who was in the middle of treatment in the United States traveled to Argentina to have additional dental procedures done.
The work was completed within a period of approximately one week. It included the removal and replacement of all metallic restorations in the patient’s mouth. The reason for their removal was attributed to “toxic focal infections,” for which the believed cause was the patient’s metallic restorations.
The patient had completed a Huneke Neural Therapy test in Argentina, which not only supposedly tested the toxicity of the restorations, but also identified the specific organ that each “toxic tooth” was “affecting.” The Huneke Neural Therapy test is based on a concept of neural therapy that was developed by 2 German physician-dentists, Drs. Walter and Ferdinand Huneke, in the 1920s and 1930s. Neural therapy is the management of pain and other illnesses by finding and treating “interference fields” or “focal points” on the body. When these are manipulated, it is believed they can relieve pain in other sites in the body.4 To date, no scientific evidence supports any such claims.5
CASE REPORT
 |
 |
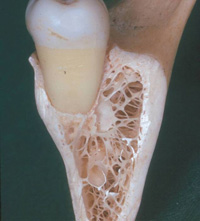
| Figure 1. Radiograph of patient before implant placement. |
Figure 2. Panoramic radiograph of patient after having previous metallic restorations removed. |
 |
 |
|
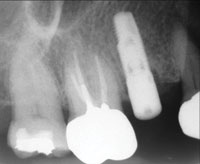
Figure 3. Implant site with metallic restorations still in place. |
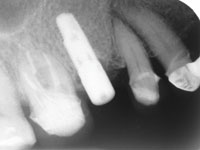
Figure 4. Untouched implant after having all other metallic restorations removed. |
 |
 |
| Figures 5 and 6. The patient was pleased with how well the implant crown color matched the new dental work. |
A 39-year-old Hispanic woman was referred to the Howard University Dental School clinic for restoration of a recently placed Bränemark 4×15-mm titanium implant at the position of tooth No. 4. The initial visit consisted of a review of the patient’s medical history, intraoral and extraoral exams, and radiographs (Figure 1). The patient’s medical history did not have any positive findings, and all vital signs were within normal limits.
Examination did not reveal anything remarkable extraorally. The intraoral exam revealed a full complement of teeth with existing dental work. Teeth Nos. 2 and 14 presented with large but serviceable silver amalgam restorations. Porcelain-fused-to-metal (PFM) crowns were noted on teeth Nos. 3, 15, 18, 19, 29, and 30; with metal posts present in teeth Nos. 3, 18, and 30. The patient also had 2 PFM bridges from teeth Nos. 5 to 9 and teeth Nos. 11 to 13. All the restorations were checked with a sharp dental explorer and passed the inspection for integrity of the margins.
The periodontal evaluation indicated a generalized, mild, soft-tissue inflammation with isolated bleeding upon probing. A neuromuscular evaluation and occlusal analysis revealed no abnormalities; the patient reported that she did not have any TMJ pain. Radiographic examination of the implant placed 6 months prior to her visit revealed signs of proper osseointegration.
Second-stage surgery to uncover the implant was performed under local anesthesia using a 5-mm-diameter punch biopsy kit. The corresponding healing abutment was subsequently attached. The patient was dismissed with instructions to return in 3 weeks. This would allow time for proper adaptation of the surrounding tissue around the healing abutment.
The patient returned with a favorable soft-tissue response. At this appointment, final impressions were taken using the corresponding impression coping with a closed-tray technique. An opposing model, bite registration, and shade were taken. The patient was then told to return in approximately 2 weeks for placement of the permanent implant crown.
On the day of the final cementation, the patient’s sister called the clinic and explained that the patient had left for the week to have dental work done in Argentina. Her appointment was rescheduled for the following week.
The following week, after returning from Argentina, the patient came in for her appointment to have her implant crown cemented. After the patient was seated, she told us that she brought a medical and dental consultation review statement of the work that had been completed in Argentina. After the document was translated from Spanish to English, it was revealed that the patient had participated in a Huneke Neural Therapy test. This report detailed an analysis of every tooth previously restored with metal, with its respective and alleged systemic repercussions. These ailments included back, stomach, and muscle pains supposedly due to the patient’s metallic restorations. When the patient was questioned as to why she did not report these ailments during the review of our initial health questionnaire, the patient responded, “I was not aware of these problems before I had my teeth tested.”
New soft- and hard-tissue exams were performed on the patient. Examination also included full-mouth radiographs, a panoramic radiograph (Figure 2), photos, and the examination of any new dental work. Radiographic examination revealed that all previously placed metallic restorations (including all amalgam restorations, core buildups, metallic posts, and PFM crowns) had been removed except the implant (Figures 3 and 4). The treatment report that the patient provided stated, “The Huneke test was positive to the indicated teeth showing evidence that the cause of the described symptoms (is due to) the metallic restorations found in the mouth. Treatment shall consist of removal of all metallic restorations and the replacement with non-metallic restorations.” New restorations were checked for contacts, occlusion, and marginal integrity. Using a sharp dental explorer, several open margin areas were noted around the newly placed bridgework and crowns. When asked if the patient noticed any changes in her health after treatment was completed, she responded, “I’m not sure. I have not noticed any changes yet.”
She was not informed in Argentina that any alterations to her current metallic restorations might affect restorations in progress in the United States. The teeth the implant crown would have contacted (teeth Nos. 3 and 5) and the occluding teeth (Nos. 29 and 30) had been replaced with new all-ceramic restorations. Attempts to seat the implant crown were unsuccessful. The patient was informed that either the implant crown must be remade or attempts could be made to adjust the crown to see if it could be seated.
Due to the added time that would be required to remake the crown and the concomitant financial considerations, the patient opted simply to have the crown adjusted. She was then informed of the possibility that after adjustments the crown may still not fit properly and a remake might still be needed. Adjustments were made to both the interproximal contacts and occlusal surfaces with a high-speed diamond under copious water irrigation. After this, the crown was seated and the interproximal contacts and occlusion were checked. During the adjustments, perforation of the porcelain, exposing the zirconium substructure, had occurred. However, the crown was able to be seated without discomfort to the patient. The patient was then shown the crown, color was compared to the new dental work (Figures 5 and 6), and she approved the cementation procedure. The crown was cemented with Fuji Plus (GC America) glass ion-omer cement, and a final radiograph was taken.
The patient was seen 6 months later for follow-up and a prophylaxis. When questioned, she reported that she had no changes in any ailments or her quality of life after having had the new dental care completed. She did report that she was happy with how her new crowns and bridges looked. She was made aware of the potential problems that may occur with the open margins. She reported that she spent close to $3,000 (USD) for all of her dental work in Argentina. The patient was placed on a 4-month continuing care schedule, and she was given a guarded prognosis for several of the newly restored teeth. It should be noted that she had no desire to replace any of the crowns found to have open or questionable margins.
DISCUSSION
The concept that oral conditions can significantly influence events elsewhere in the body is not new, and it has undergone a number of transformations over the years.6 While this may be foreign to most physicians in the United States, dentists have known for quite some time about the importance of oral heath and its effects on systemic health. The possibility that events in the oral cavity can influence systemic disease has been mentioned in the Surgeon General’s report7 in 2000 and in various other studies. These studies report a link between oral disease and such systemic diseases as coronary heart disease, stroke, adverse pregnancy outcomes, diabetes, and bacterial pneumonia.6 However, these conditions have nothing to do with “interference fields.” Instead, they are related to periodontal pathogens affecting the body through 2 proposed pathways.8,9
When people travel to foreign countries (especially underdeveloped countries) for dental work, they either ignore or are unaware of the obvious differences in training, infection control, sterilization, and materials standards in clinics. Furthermore, there can be differences between countries in the philosophy of care and various treatment modalities. Government and basic medical insurance, and sometimes extended medical insurance, often fail to cover those medical and dental procedures.
Most countries that offer these services have little or no follow-up care, weak oversight agencies to monitor the quality of care, and little or no legal action available for patient recourse, if needed. While this may help keep healthcare costs down in other countries, it allows for the possibility of less-than-ideal care to be given without ramification. Complications, side effects, and postoperative care are then the responsibility of the medical and dental care system in the patient’s home country.
Dentists in the United States may be reluctant to care for patients who have been treated outside of the country because the patient may blame them for complications related to treatment. The patient’s local dentist is placed in the ethical dilemma of informing these patients that less-than-ideal care was performed, and then must decide whether to retreat. The ADA’s Principles of Ethics and Code of Professional Conduct addresses the issue of “Justifiable Criticism” in Code Section 4.C, stating, “Dentists shall be obliged to report to the appropriate reviewing agency as determined by the local component or constituent society instances of gross or continual faulty treatment by other dentists. Patients should be informed of their present oral health status without disparaging comment about prior services.” This becomes a gray area when dealing with these types of situations, since most “reviewing agencies” are from underdeveloped countries. In the 2006 ADA House of Delegates meeting, the association addressed dental tourism for the first time in its history. By doing so, the ADA recognized the grow?ing trend of United States residents traveling outside the border for healthcare.10
CONCLUSION
As dental tourism continues to grow, dentists will be faced with difficult decisions. When patients who have had dental work completed in a foreign country return to their dentists in the United States, those professionals will now have to determine the best way to manage the treatment that was done elsewhere. While this issue was identified much earlier in the medical field, many dentists are still not fully aware of this issue or the repercussions. The lack of knowledge about this issue makes dealing with it difficult. By the ADA formally addressing this problem in 2007, it marked the beginning of a possible solution. The answer, however, will be difficult to determine. This difficulty is due to the complex nature of why certain people choose to have sensitive medical and dental care done away from home. As the ADA spreads awareness about this situation, not only will the dental community have a better understanding on how to deal with these complex issues, but the patients who seek this care in foreign countries might also begin to understand the ramifications as well.
References
- Medical tourism. http://en.wikipedia.org/wiki/Health_tourism. Accessed April 23, 2006.
- Practising medical tourism: a resounding success. Express Health-care Management [Indian newspaper]. March 2006. http://www.expresshealtharemgmt.com/200603/medicaltourismconf01.shtml. Accessed April 23, 2006.
- Abdullah BJJ, Ng KH. The sky is falling. Biomed Imaging Interv J. 2006;2:e29. http://www.biij.org/2006/3/e29/default.asp. Accessed May 29, 2006.
- Dosch JP, Dosch M. Manual of Neural Therapy According to Huneke. 11th ed. Heidelberg, Germany: Haug Publishers; 1984.
- Neural therapy. American Cancer Society Web site. http://www.cancer.org/docroot/ETO/content/ETO_5_3X_Neural_Therapy.asp?sitearea=ETO. Accessed December 16, 2006.
- Barnett, Michael L. The oral-systemic disease connection: an up-date for practicing dentists. The Journal of the American Dental Association, vol. 137 [Web Page] Available at http://jada.ada.org (Accessed October 2006).
- US Department of Health and Human Services. Oral health in America: a report of the surgeon general. http://www2.nidcr.nih.gov/sgr/sgrohweb/home.htm. Effective September 2000. Accessed December 2, 2006.
- Haraszthy VI, Zambon JJ, Trevisan M, et al. Identification of periodontal pathogens in atheromatous plaques. J Periodontol. 2000;71:1554-1560.
- Chiu B. Multiple infections in carotid atherosclerotic plaques. Am Heart J. 1999;138(5 pt 2):S534-S536.
- Furlong A. 2006 delegates focus on dental tourism. American Dental Association Web site. http://www.ada.org/prof/resources/pubs/adanews/adanewsarticle.asp?articleid=2230. Posted November 17, 2006. Accessed December 12, 2006.
Dr. Vaughn is a full-time associate in a family practice focusing on cosmetic dentistry in northern Virginia. He earned his DDS degree from the University of Michigan School of Dentistry and his AEGD certificate from Howard University School of Dentistry. He can be reached at parisvaughn@gmail.com or at (703) 580-1443.
Ms. Whitley is a full-time dental hygienist in a cosmetic dental practice in Silver Spring, Md. She earned her RDH degree from Howard University and her BA degree from Trinity University. She can be reached at (202) 641-4201.
Disclosure: The authors have no financial interest in any of the companies mentioned in this article.