
Oral implantology has made great strides since introducing the concept of osseointegration, and there is a continuous search for excellence with more predictable planning for aesthetics and function. Implant installation should be prosthetically guided, respecting anatomical limitations and bone availability.
In many cases, computer-guided surgery and prototyped surgical guides eliminate the need for the mucoperiosteal flap. They should be considered the gold standard for achieving perfect 3D implant positioning.
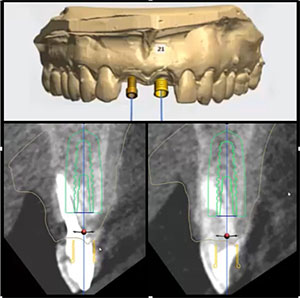
This report describes the full digital workflow of a patient who underwent extraction of teeth Nos. 8 and 9 with immediate implants installed in the aesthetic zone. Guided surgery without flap displacement was performed through virtual planning using software and stereolithographic surgical guides.
 |
 |
| Figure 2. Preoperative panoramic radiography. | Figure 3. Virtual 3D planning. |
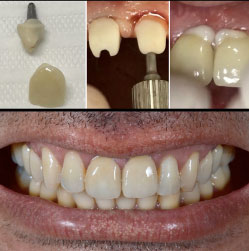
The CAD/CAM chairside technique was used to make the definitive metal-free crowns. This technique has shown excellent accuracy even when extractions are performed in the same session, making the procedure faster and offering many advantages in terms of favorable aesthetics, desirable occlusion, and long-term peri-implant hard-tissue and soft-tissue stability.
Background
Root fractures, endodontic failures, extensive cavities, and severe periodontal disease are the most common reasons for anterior tooth loss.1
 |
 |
| Figure 4. Stereolithographic printing of surgical guide. | Figure 5. Extraction of tooth No. 9; surgical guide positioned on the maxilla; implant placement; the gap between socket and implant filled with alloplastic bone substitute. |
Since the development of osseointegrated implant systems and the publication of the first longitudinal studies evaluating their success and survival, contemporary implantology’s primary focus has been investigating less invasive and more predictable surgical techniques that reduce treatment times.2
The 3D positioning of a dental implant is considered a prerequisite for an ideal aesthetic result.3-5 This positioning is crucial in the aesthetic zone because patients generally have higher expectations for treatment and aesthetic outcomes.
In 2004, Buser3 reported that the mesiodistal, buccolingual, and apicocoronal dimensions are well described, defining comfort and danger zones for the implant’s proper position in the anterior region of the maxilla. According to a 2019 study by Chein,4 an accurately placed implant could simplify prosthetic procedures, aesthetic results, and the long-term stability of peri-implant hard and soft tissues.
 |
| Figure 6. Immediate provisioning of implant No. 9 and postoperative panoramic radiography. |
The advantages of a single surgical procedure, reducing the total treatment time, have encouraged professionals to install the implant immediately after tooth extraction.1 A flapless approach is recommended to preserve the blood supply to the fascicular bone, providing better healing of soft tissues, avoiding interruption of the bone blood supply, and improving the patient’s comfort.6
Recent studies7-11 have found alveolar and peri-implant bone loss comparable to implant procedures performed later. However, a slightly lower survival rate was observed in immediate implants (95.21%)12 than in late implants (98.38%).
In cases where there is resorbed or deficient buccal bone wall, there is a need to regenerate the missing structure using block grafting, guided bone regeneration with barrier membranes, and suitable bone grafts13 and/or bone substitutes.3
 |
| Figure 7. Intraoral scanning with CEREC system for implants Nos. 8 and 9; digital design; manufacture of multilayer prosthesis with lithium disilicate pillars and crowns of feldspar ceramic, polychromatic. |
Oral implantology has entered a new era due to advances in CAD/CAM technology.14 The advent and wide availability of CBCT and a constant evolution in software have contributed to the development of techniques that has led to greater confidence in the use of guided surgery.2,5 The transfer needs ideal positioning of the implant, from the virtual planning to the implant’s placement. It is essential to protect structures and optimize aesthetic and functional results.6
Digital planning involves synchronizing a patient’s digital files and generating a 3D view of the dental hard and soft tissues through software, where virtual surgeries for implant placement are performed. Finally, surgical guides are manufactured using rapid prototyping or stereolithographic technology,14 and this technology can rule out the use of a surgical flap.2
Case Report
A 39-year-old male was referred to the Department of Oral Implantology of Odontoclínica da Aeronáutica Santos Dumont (Brazilian Air Force), Rio de Janeiro, Brazil, indicating extractions of teeth Nos. 8 and 9 and rehabilitation with dental implants. Imaging exams showed cavities in the cervical third of the root of tooth No. 8 and resorption in the root apexes, contraindicating their preservation (Figures 1 and 2).
 |
| Figure 8. Installation of pillars and cementation of the crowns with resin cement. |
Clinically, the amount of keratinized mucosa was considered satisfactory. During probing, a pocket depth of less than 3 mm was observed. The smile line, periodontal condition, papillae, and mucosa adjacent to neighboring teeth were also evaluated.
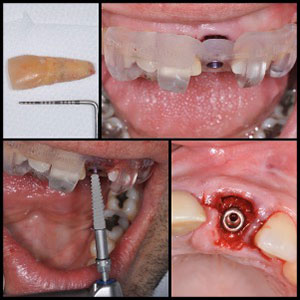
Given the clinical, radiographic, and aesthetic needs, we opted to extract teeth Nos. 8 and 9 and install implants with immediate loading, using the guided flap surgery technique.
The diagnostic impressions of the upper and lower arches and the DICOM file, obtained by CBCT, were sent to a digital planning center in our facility to carry out the virtual planning using software and the fabrication of stereolithographic surgical guides supported by teeth.
During 3D planning, some essential factors for the treatment’s success were observed, including the maintenance of the proximal bone crest, an indispensable element in the interproximal papillae’s care since it is responsible for supporting soft tissue and the remaining bone for the installation of immediate implants.
Two dental implants, 3.5 by 16 mm, were planned (Drive CM, Neodent, Curitiba, PR, Brazil) using two different surgical guides for teeth Nos. 8 and 9, respecting the minimum interval of three months between surgeries (Figure 3). The strategy aimed to minimize trauma to the bone crest and maintain the interdental papilla between the central incisors (Figure 6).
One hour before the procedure, the patient was premedicated with 1 g of amoxicillin and 8 mg of dexamethasone. After local anesthesia, using two tubes of 2% lidocaine with epinephrine 1: 100.000, tooth No. 8 was extracted atraumaticaly, using the peritome to preserve papillae, marginal gums, and bone structures.
The surgical sequence without detaching the mucoperiosteal flap was started after the surgical guide’s placement, supported on the adjacent teeth. Surgical instrumentation followed the progressive sequence of guides and drills from the Neodent Guided Surgery Alvim Surgical Kit (Neodent, Curitiba, PR, Brazil), with constant and abundant irrigation with 0.9% saline solution.
A 3.5- by 16-mm implant (Neodent, Curitiba, PR, Brazil) was installed, keeping the implant around 5 mm below the gingival margin. The primary stability of more than 45 Ncm allowed the use of the immediate load philosophy. The surgical guide was removed, and the 3.3- by 6- by 2.5-mm CM Universal abutment (Neodent, Curitiba, PR, Brazil), indicated for cemented prosthesis, was placed and adapted on the implant, with a torque of 32 Ncm. The gap between socket and implant was filled with approximately 0.2 cc of Alobone (Osseocon, Rio de Janeiro, Brazil), a synthetic biomaterial (alloplastic).
Finally, immediate provisionalization and occlusal adjustment were performed to improve immediate aesthetics and adequate masticatory function. Six-hundred milligrams of ibuprofen were prescribed orally for the patient every eight hours for pain.
The patient returned seven days after the operation without local pain or discomfort. After three months, the same surgical steps were performed for tooth No. 9, and immediate panoramic radiography was performed (Figures 7 and 8).
Through the digital flow, we used the CEREC system (Dentsply Sirona) to perform intraoral scanning of implants No. 8 and 9, using TiBases and ScanBodies. After the digital design and manufacture of the multi-layered prosthesis with lithium disilicate pillars (IPS E-max CAD, Ivoclar Vivadent) and polychromatic feldspar ceramic crowns (Cerec Blocs PC, Dentsply Sirona) (Figure 9), cementation was performed in the mouth with Calibra Ceram (Dentsply Sirona), a resin cement (Figure 10).
Discussion
Imprecise placement of the implant may occur due to limited mouth opening, asymmetric bone density, or the clinician’s lack of experience.4 A study carried out by Canullo in 2016 showed that poor positioning surgically triggered almost half of the cases of peri-implantitis examined.15
The implant’s correct positioning has been identified as a crucial factor for an excellent aesthetic and functional result.3-5 In addition to aesthetics, correct positioning can reduce technical and/or biological complications.15
The immediate installation of implants in the alveoli of extracted teeth reduces treatment time. It preserves the alveolar bone’s height and thickness and the soft-tissue dimension, promoting more significant bone-implant contact.1,6
According to Tabassum,14 immediate implantation may be more difficult in clinical situations due to the proximity of adjacent teeth or critical anatomical structures, such as the lower alveolar canal and maxillary sinus.
To preserve the peri-implant region, it is necessary to maintain soft and hard tissues for better functional and aesthetic results. This is possible with the optimization of treatment, reducing the number of surgical interventions.1
Surgical techniques can affect the gingival papillae’s shape. Thus, atraumatic protocols for immediate implantation have been developed to reduce damage to soft tissues and preserve aesthetics. Three dimensions must be considered when it comes to techniques and procedures concerning the implants’ bone status: mesiodistal, buccolingual, and apicocoronal.
Based on this, the adequacy of bone and soft tissues should be evaluated before surgery. Studies report, for example, that the simultaneous removal of adjacent teeth causes the collapse of the bone crest, remodeling the bone board. According to the diagnostic keys of Kois, this remodeling is an essential factor for forming the papilla.16
According to Chen et al,6 three different surgical approaches were available in 2018: freehand, computer-guided, and surgery with transoperative navigation.
Also known as mental navigation, the freehand process involves the clinician manually transferring the implant’s planned position to the surgical site, with access to virtual software planning during the surgery.
Computer-guided surgery uses a manufactured, computer-aided surgical guide that guides the drills and the implant in a specific direction.
Surgery with computer-operated transoperative navigation requires the application of a system that provides real-time information about implant placement.
Surgery virtually guided by computerized planning and prototyped surgical guides represents one of the significant advances in modern oral implantology. Tabassum14 said it minimizes the risks of possible complications and offers many advantages in terms of pleasing aesthetics, desirable occlusion, phonetics, and hard and soft tissues’ stability. Younes et al15 reported that guided surgery should be considered the gold standard approach to achieve perfect 3D positioning of the implant.
In 2018, Chen et al6 carried out a pilot study with 24 upper incisors on eight heads of human cadavers, comparing the precision of freehand and computer-guided surgery in placing an immediate implant without a flap in the anterior maxilla.
They concluded that freehand surgery’s imprecision is significantly greater in most of the evaluated parameters and that immediate implants tend to deviate toward the buccal area, even under computer-guided surgery.
Virtual guided surgery is so precise that this average accuracy change is within 1 mm for implant placement and up to 5 degrees of deviation from its inclination. In other words, it is significantly more accurate than the freehand method.17
Thus, technological advances in oral implantology have considerably increased the number of rehabilitation procedures in patients with immediate aesthetic needs. With the evolution of new diagnostic and planning techniques and resources, surgical procedures have become faster and less invasive, ensuring success, predictability of treatment, and patient satisfaction.
Conclusion
Within the limitations of the present study, guided surgery should be considered the gold standard approach to achieve the correct 3D positioning of the implant.
The digital flow presented was shown to be accurate for immediate implants in the aesthetic area and allowed the installation of permanent crowns in a single clinical session.
References
- Oliveira Filho FA, Rebelo HL, de Souza Dias TG, Melo Barbalho JC, Araújo de Morais HH. Regeneração óssea guiada com carga imediata em zona estética: relato de caso clínico. Rev Cir Traumatol Buco-Maxilo-Fac. 2015;15(2):33-38.
- Moraschini V, Velloso G, Luz D, Barboza EP. Implant survival rates, marginal bone level changes, and complications in full-mouth rehabilitation with flapless computer-guided surgery: a systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2015;44(7):892-901. doi:10.1016/j.ijom.2015.02.013
- Buser D, Martin W, Belser, UC. Optimizing esthetics for implant restorations in the anterior maxilla: Anatomic and surgical considerations. Int J of Oral and Maxillofac Implants. 2004; 19(Suppl): 43–61.
- Chen L, Lin WS, Polido WD, Eckert GJ, Morton D. Accuracy, reproducibility, and dimensional stability of additively manufactured surgical templates. J Prosthet Dent. 2019; 122(3):309-314. doi:10.1016/j.prosdent.2019.02.007
- Younes F, Eghbali A, De Bruyckere T, Cleymaet R, Cosyn J. A randomized controlled trial on the efficiency of free‐handed, pilot‐drill guided and fully guided implant surgery in partially edentulous patients. Clin Oral Impl Res. 2019;30:131–138. doi:10.1111/clr.13399
- Chen Z, Li J, Sinjab K, Mendonca G, Yu H, Wang HL. Accuracy of flapless immediate implant placement in anterior maxilla using computer-assisted versus freehand surgery: a cadaver study. Clin Oral Impl Res. 2018;29(12):1186-1194. doi:10.1111/clr.13382
- Zhang S, Wang S, Song Y. Immediate loading for implant restoration compared with early or conventional loading: A meta-analysis. J Craniomaxillofac Surg. 2017;45(6):793-803. doi:10.1016/j.jcms.2016.05.002
- Lee J, Park D, Koo KT, Seol YJ, Lee YM. Comparison of immediate implant placement in infected and non-infected extraction sockets: a systematic review and meta-analysis. Acta Odontol Scand. 2018;76(5):338-345. doi:10.1080/00016357.2018.1453084
- Lee CT, Chuang SK, Stoupel J. Survival analysis and other clinical outcomes of immediate implant placement in sites with periapical lesions: systematic review. Int J Oral Maxillofac Implants. 2015; 30(2):268-278. doi:10.11607/jomi.3619
- Martin C, Thome G, Melo AC, Fontao FN. Peri-implant bone response following immediate implants placed in the esthetic zone and with immediate provisionalization—a case series study. Oral Maxillofac Surg. 2015;19(2):157-163. doi:10.1007/s10006-014-0470-5
- Takeshita K, Vandeweghe S, Vervack V, Sumi T, De Bruyn H, Jimbo R. Immediate implant placement and loading of single implants in the esthetic zone: clinical outcome and esthetic evaluation in a Japanese population. Int J Periodontics Restorative Dent. 2015; 35(5):715-723. doi:10.11607/prd.2494
- Mello CC, Lemos CAA, Verri FR, Dos Santos DM, Goiato MC, Pellizzer EP. Immediate implant placement into fresh extraction sockets versus delayed implants into healed sockets: A systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2017;46(9):1162–77. doi:10.1016/j.ijom.2017.03.016
- Rosa JC, Rosa AC, Francischone CE, Sotto-Maior BS. Esthetic outcomes and tissue stability of implant placement in compromised sockets following immediate dentoalveolar restoration: results of a prospective case series at 58 months follow-up. Int J Periodontics Restorative Dent. 2014;34(2):199-208. doi:10.11607/prd.1858
- Tabassum A. Guided implant surgery and immediate implant placement in esthetic zone. Int J Med Dent Case Rep. 2018;5:1-5. doi:10.15713/ins.ijmdcr.92
15. Younes F, Cosyn J, De Bruyckere T, Cleymaet R, Bouckaert E, Eghbali A. A randomized controlled study on the accuracy of free‐handed, pilot‐drill guided, and fully‐guided implant surgery in partially edentulous patients. J Clin Periodontol. 2018;45(6):721–732. doi:10.1111/jcpe.12897
- Soares NP, Pimentel AC, Cançado RM, et al. Determining factors for formation and/or maintenance of peri-implant papilla: Literature review. Dental Press Implantol. 2013; 7(2):73-80.
- Nickenig HJ, Eitner S, Rothamel D, Wichmann M, Zoller JE. Possibilities and limitations of implant placement by virtual planning data and surgical guide templates. Int J Comput Dent 2012;15(1):9-21.
Tariza Gallicchio Moreira is a member of the Oral and Maxillofacial Surgery Department of the Brazilian Navy in Rio de Janeiro, Brazil.
Carlos Fernando de Almeida Barros Mourão is a member of the Biotechnology Department and the Department of Oral Surgery at the School of Dentistry at the Universidade Federal Fluminense of Niterói in Rio de Janeiro. Correspondence may be sent to mouraocf@gmail.com.
Kayvon Javid is enrolled in the postgraduate program at the School of Dentistry at the Univesridade Federal Fluminense of Niterói.
Marcela Ferraz Catramby is a member of the Oral Implantology Department of the Brazilian Air Force in Rio de Janeiro, Brazil.
Daniel Costa Ferreira de Almeida is a member of the Oral Implantology Department of the Brazilian Air Force in Rio de Janeiro, Brazil.
Vittorio Moraschini is a member of the Periodontology Department, Dental Research Division, at the School of Dentistry at Veiga de Almeida University in Rio de Janeiro, Brazil.
Related Articles
Know the Risks Before Adding Phlebotomy to Your Dental Practice
Management of Oral Viral Lesions With a Diode Laser











