INTRODUCTION
Do you ever stop to reflect that, as dentists, we are living in a truly amazing time? We have incredible technology at our fingertips, and patients are fortunate to have unprecedented access to dental care.
But no matter how much shiny, state-of-the-art technology is available, if dentists believe that a tooth can’t be saved, it automatically becomes impossible to save it. We were all taught to cultivate certain beliefs in dental school. However, have you ever thought, “I wonder if that tooth would respond to treatment?” Remembering your training, though, you decided the safest bet was to extract.
Over the years as a practicing endodontist, I’ve been privileged to witness so many “unsavable” teeth be saved that I knew I had to re-examine my own beliefs.
Today, I view myself as a tooth saver, and I’d like to encourage all of us to open ourselves up to new beliefs about which teeth can be saved. This way, we can serve our patients at an even higher level.
Teeth are so incredibly important, but since we treat them day in and day out, we sometimes lose sight of the bigger picture.
What if our beliefs were the most important piece of technology that we really needed to upgrade? Take a moment, step back, and think about it. I view our teeth as tiny little temples within our mouths—the gateway to our bodies. Our teeth help nourish and hydrate our bodies, and they give us confidence when we smile. Teeth are precious, and we were born with them for many reasons.
Right now, I believe we are being called to make a shift in our beliefs around saving vs extracting these precious pearls that Mother Nature gave each of us. That way, we can wholeheartedly help our patients.
We can each trust ourselves to save teeth, and we can trust the incredible power of the human body to heal when given proper treatment. Believe in your healing power as a dentist.
I’m not asking you to shift your beliefs without evidence, though. So I’m going to use real tooth stories from my own practice to explore some of the biggest and most common dental beliefs about “unsavable” teeth. Once we shift these beliefs into the new, upgraded beliefs I will propose, we can make a long-lasting, positive impact on the patients we touch. Walk with me down Tooth Story Lane, and I hope you will feel inspired, empowered, and ready to make an upgrade to your beliefs.
COMMON BELIEF NO. 1: BIG LESIONS DON’T HEAL
How do you feel when you encounter a big lesion? If you’re thinking, “It’s hopeless; let’s extract it,” you aren’t alone, my friend. Across the community of dental professionals, there are different views on whether these teeth should be extracted or saved.
It’s easy to be concerned about the amount of bone loss around the tooth. The general teaching in dentistry is that the tooth will not respond to treatment, especially when there is a loss of the buccal cortical plate. In this situation, it’s not uncommon for us, as dentists, to believe the treatment won’t work.
But there is a shining beacon of hope. We can actually see healing in this scenario when we shift our thinking.
Understanding the pulpal diagnosis of the tooth—and furthermore, understanding the fact that when a patient has a necrotic pulp, it will create bone loss—is an essential part of this discussion.
Sometimes that bone loss is little, and sometimes it’s monstrously big. It will vary per case and per patient, so I encourage us not to be so quick to judge these situations with a blanket statement. If we solely look at the radiograph and treat it based on the size of that lesion without doing any endodontic diagnostic testing, we are making a diagnosis based on the limiting beliefs that have been imprinted on so many of us from our previous teachers. And that means that, despite our very best intentions and aspirations, we may be doing our patients a disservice.
It’s time to truly understand the disease process and step into our superhero roles as dentists to save teeth.
A Tooth Story About a Giant Periapical Radiolucency
Take, for example, a 46-year-old woman who presented to my office after her dentist found a periapical radiolucency around tooth No. 31. She was asymptomatic, and there was a significant amount of circumferential bone loss.
I performed my endodontic diagnostic tests and found that the tooth had no response to cold, had no pain upon percussion, and had no mobility, believe it or not. Additionally, there was a 9-mm mid-buccal probing (all other areas of the tooth probed normally). I diagnosed the tooth as necrotic pulp and chronic apical abscess on No. 31 (Figures 1a and 1b).
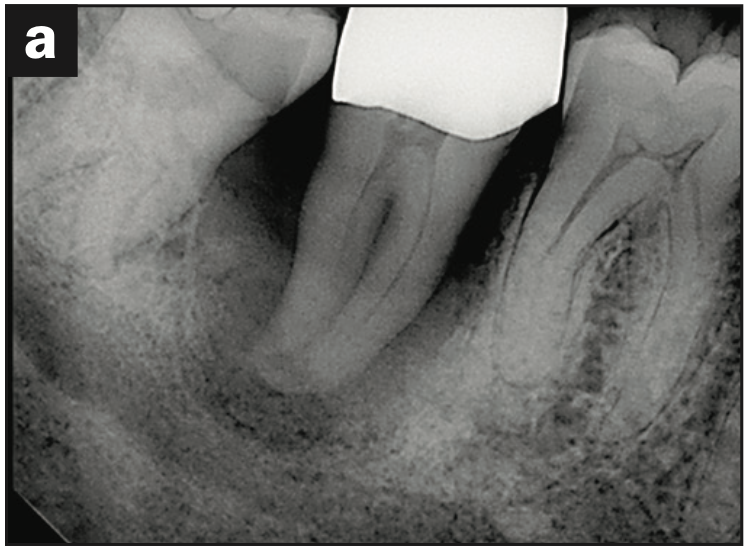
Figure 1a. Preoperative periapical radiograph of tooth No. 31.
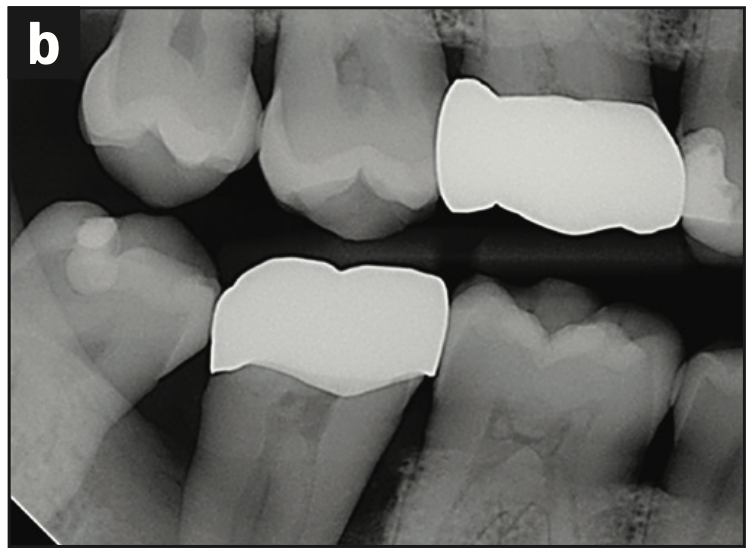
Figure 1b. Pre-op bite-wing radiograph of tooth No. 31.
Most of the time, when I present this case in my lectures, I ask the audience, “What would your treatment plan be?” The answer I most often get is “Extraction.” This is because we, as dentists, have been taught to believe that lesions of this size are incapable of healing.
Instead, what’s important to understand is that the endodontic diagnosis (not lesion size) is what will guide you to the right treatment plan.
Remember, necrotic pulps create bone loss, and sometimes that bone loss can be massive. That just happens to be what is natural for that particular patient, including the one I’m sharing with you here.
As an endodontist, I have learned to reframe the beliefs that I learned in dental school and to trust my diagnosis. So, in this case, I did the root canal (Figure 1c).
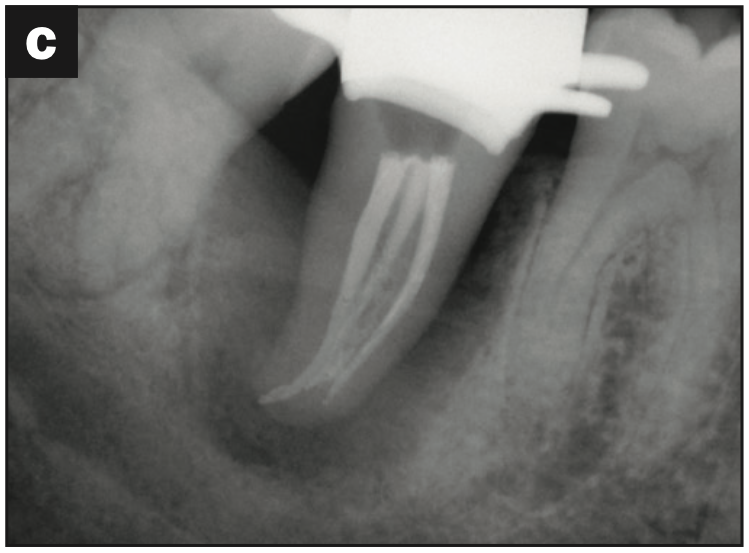
Figure 1c. Immediate final post-operative obturation radiograph of tooth No. 31.
Now, it’s just a matter of giving the body the time that it needs to regenerate that bone. This is the importance of following up with your patients when it comes to endodontics. One year later, I witnessed her great recovery. Some may call it a miracle, but it’s not. It’s simply the superpower that exists within all of us: the ability to regrow our own bone back (Figure 1d).
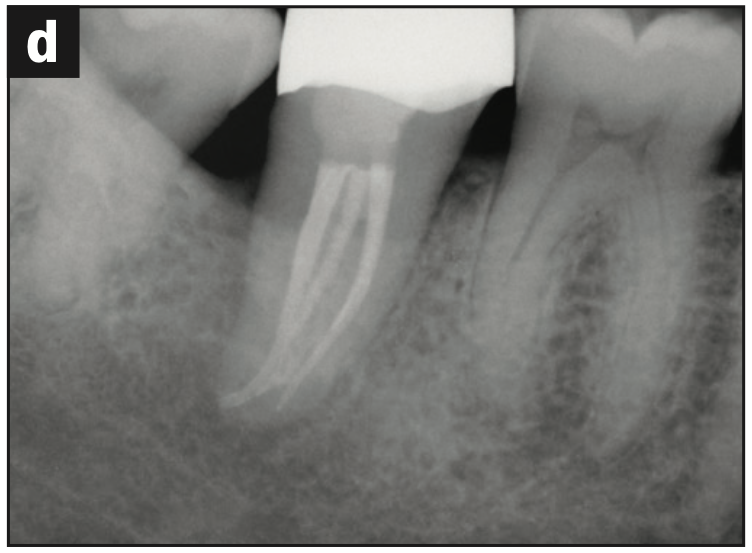
Figure 1d. One-year recall radiograph of tooth No. 31.
And at 2 years postoperatively, there was even more bone deposition and maturation (Figure 1e).
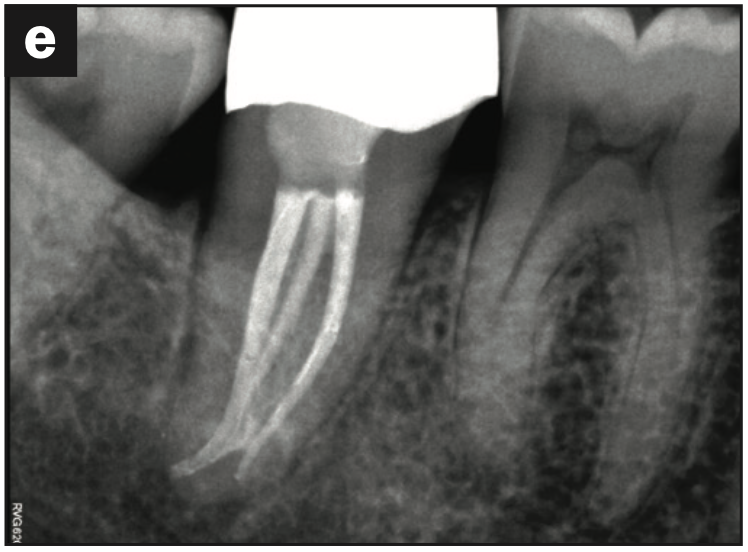
Figure 1e. Two-year recall radiograph of tooth No. 31.
All of this occurred with root canal therapy only. There was no other dental intervention.
This is not a one-off success story. It can happen time and time again in any practice—so long as we relax into what our bodies are capable of, like regrowing bone, given enough time and healing.
In sharing this case, I intend for us to understand and trust our diagnosis to save teeth. When we understand the etiology of the disease process, we can make a more effective and meaningful treatment plan that we can be confident will serve our patients.
But if we were taught that big lesions don’t heal, and we impose that belief on our patients, it may lead them in the wrong direction. So many other dentists would have extracted this tooth.
I believe that when we, the providers, can reframe our dental beliefs to trust that lesions can heal with endodontic treatment—no matter their size—we can serve our patients to the fullest extent possible.
Tooth-saving belief No. 1: Lesions can heal with endodontic treatment, no matter their size.
COMMON BELIEF NO. 2: THE J-SHAPED RADIOLUCENCY MEANS THE TOOTH IS FRACTURED
The J-shaped radiolucency most certainly gets a bad reputation when making an endodontic diagnosis. And despite having more than a decade of endodontic experience as a specialist, it still makes me second-guess my own diagnoses when I see them.
However, we now know and accept that the human body will look for the pathway of least resistance to drain an infection, and this may just happen to look like a J-shaped radiolucency, meaning that the tooth is not cracked at all.
If there is one thing I could change about endodontic education within dental school, it would be to emphasize the fact that J-shaped radiolucencies are not synonymous with root fractures.
If you are questioning the probing on the mid-buccal because you, like me, were taught that a probing equates to a root fracture—and, therefore, a non-restorable tooth—I want to address your concern. It is also not true that an area that probes is always associated with a root fracture. A probing can simply mean that the body found the pathway of least resistance to drain the infection and created a sinus tract (hence the diagnosis of a chronic apical abscess).
This sinus tract can drain through the sulcus and does not need to look like a pimple on the gingiva. Unfortunately, this sinus tract clinically looks just like a probing that is associated with a root fracture, so it most definitely complicates the endodontic diagnosis and creates a layer of uncertainty.
Let’s explore an example to illustrate this point.
A J-Shaped Radiolucency Tooth Story
A 38-year-old woman had a previous root canal that appeared to be failing. When I looked at her preoperative radiographs, I could see that notorious J-shaped radiolucency around the mesial root and even some bone loss around the distal root (Figures 2a and 2b).
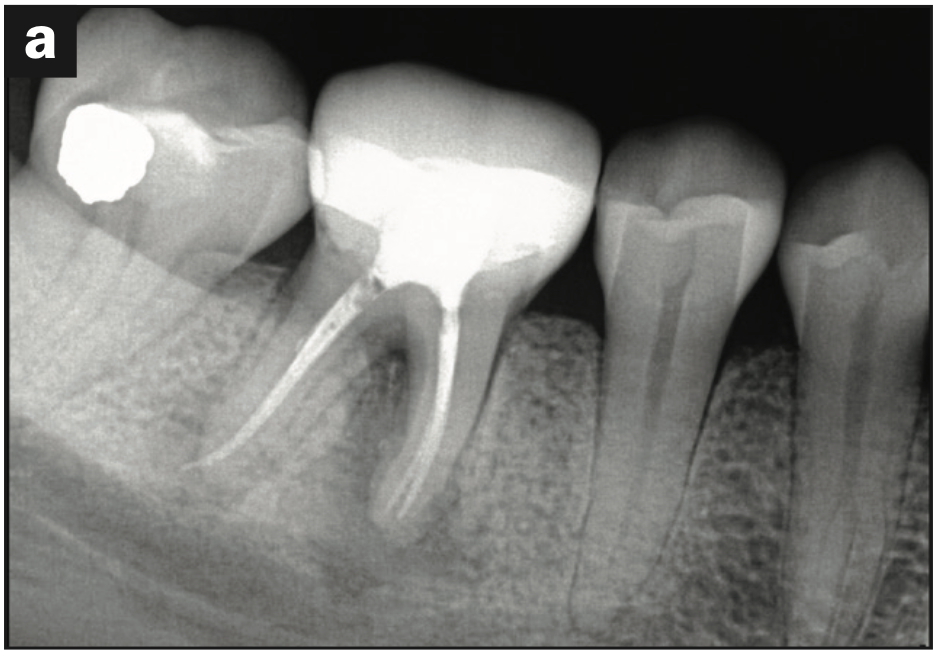
Figure 2a. Pre-op periapical radiograph of tooth No. 30.
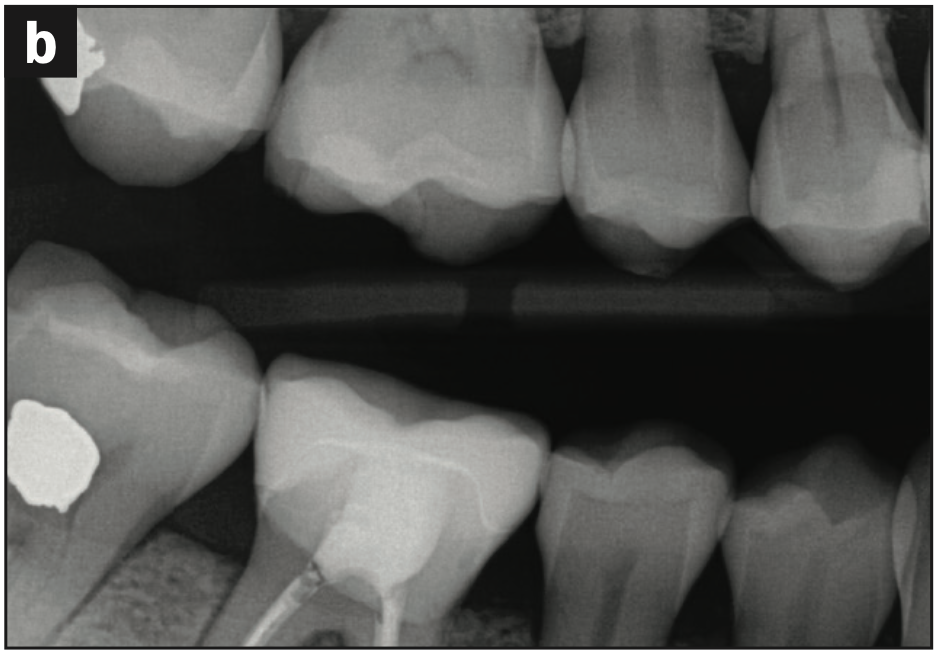
Figure 2b. Pre-op bite-wing radiograph of tooth No. 30.
My diagnostic tests showed that there was some moderate tenderness to percussion and obviously no response to cold. All other findings were within normal limits, except that there was a 9-mm mid-buccal probing. The diagnosis was a previously treated and chronic apical abscess on No. 30.
I also obtained a pre-op cone beam, which more clearly delineated the classic J-shaped radiolucency (Figures 2c to 2f).
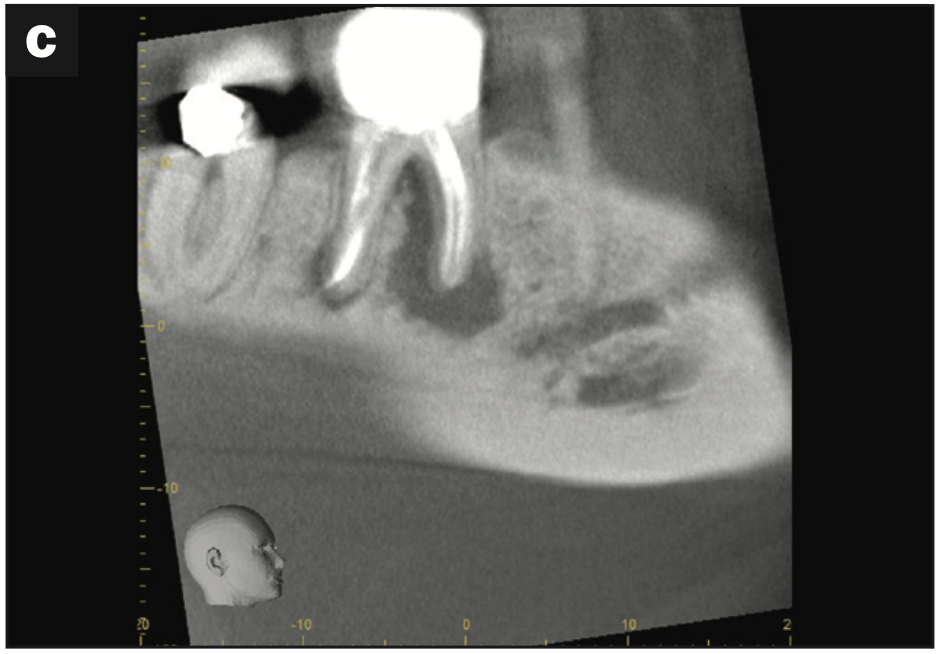
Figure 2c. Pre-op sagittal CBCT view of tooth No. 30.
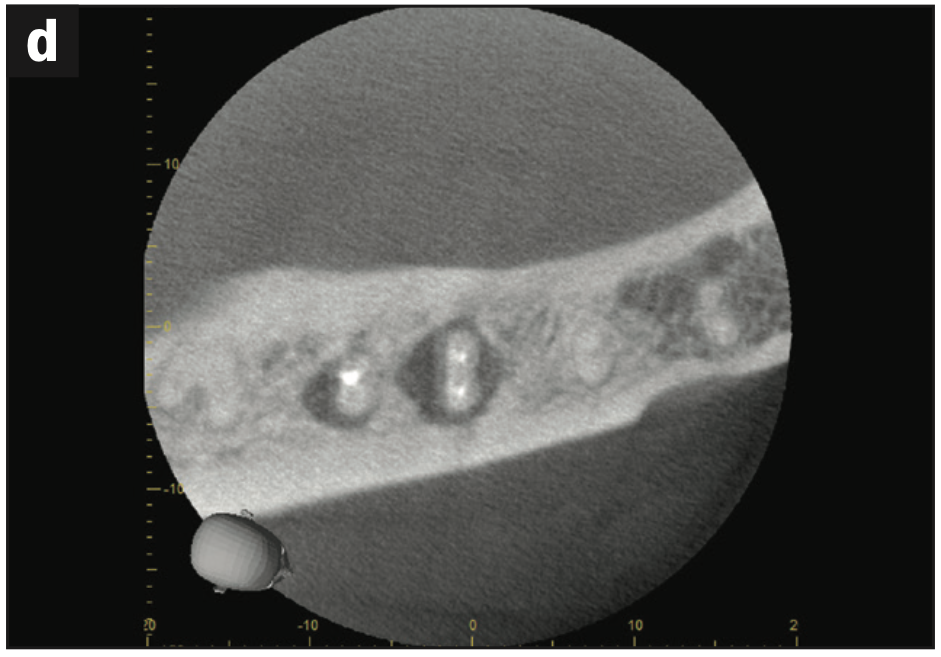
Figure 2d. Pre-op axial CBCT view of tooth No. 30.
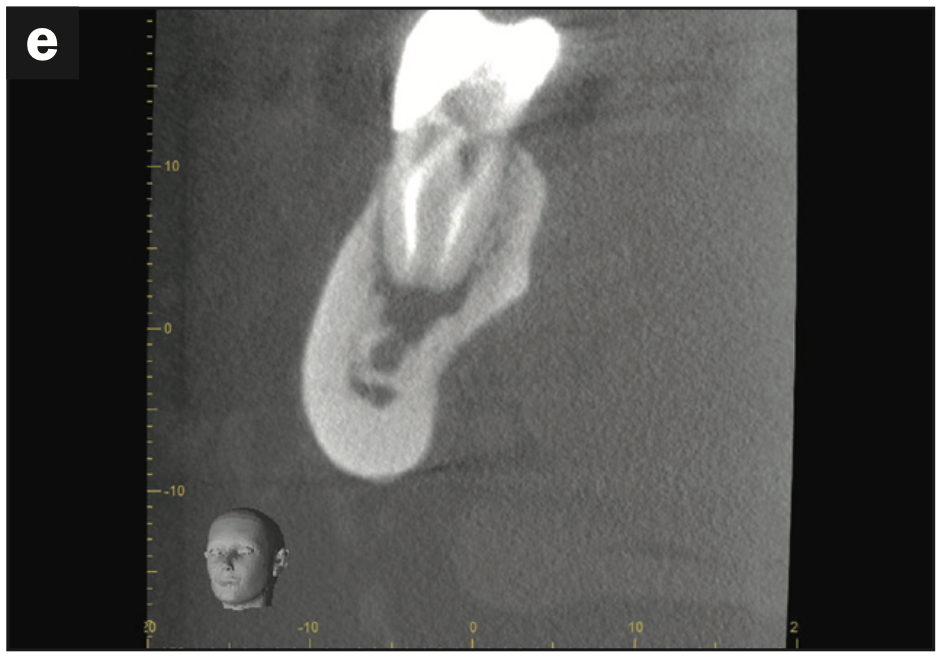
Figure 2e. Pre-op coronal CBCT view of the mesial root of tooth No. 30.
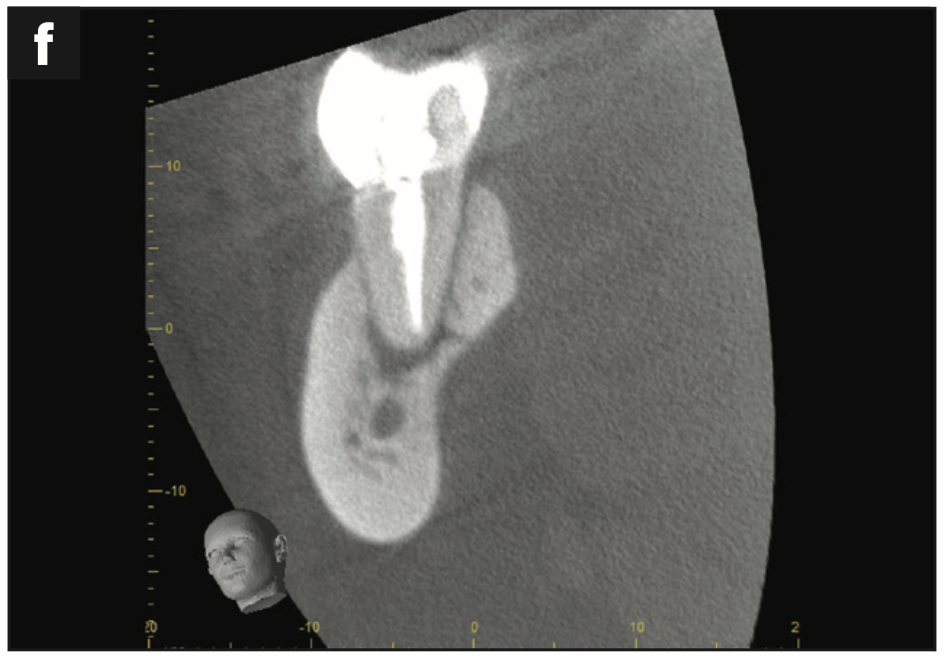
Figure 2f. Pre-op coronal CBCT view of the distal root of tooth No. 30.
I had a long discussion with the patient to present all of her treatment options, including endodontic re-treatment vs extraction. This is because I always want to empower my patients with knowledge so that they can make the best choices for their health.
We decided together that we both felt comfortable attempting the re-treatment to see if we could save the tooth. I told her that if I located an internal fracture under magnification, I would have to refer her for the extraction.
The patient, however, wanted to do whatever it took to save her tooth, which meant giving treatment a try. I was on board with this plan because, over the years, giving teeth a chance has allowed me to see what magic our bodies are truly capable of.
Upon removing the gutta-percha and carefully inspecting the internal walls of the tooth, I didn’t see any sign of a fracture, so I continued to obturate the tooth (Figures 2g and 2h).
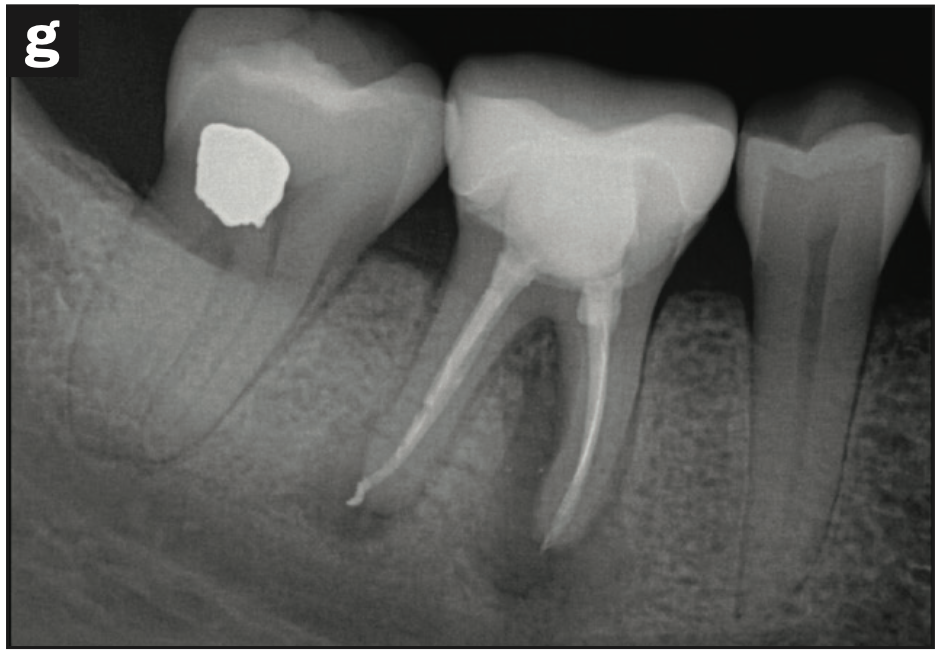
Figure 2g. Immediate post-op radiograph of tooth No. 30.
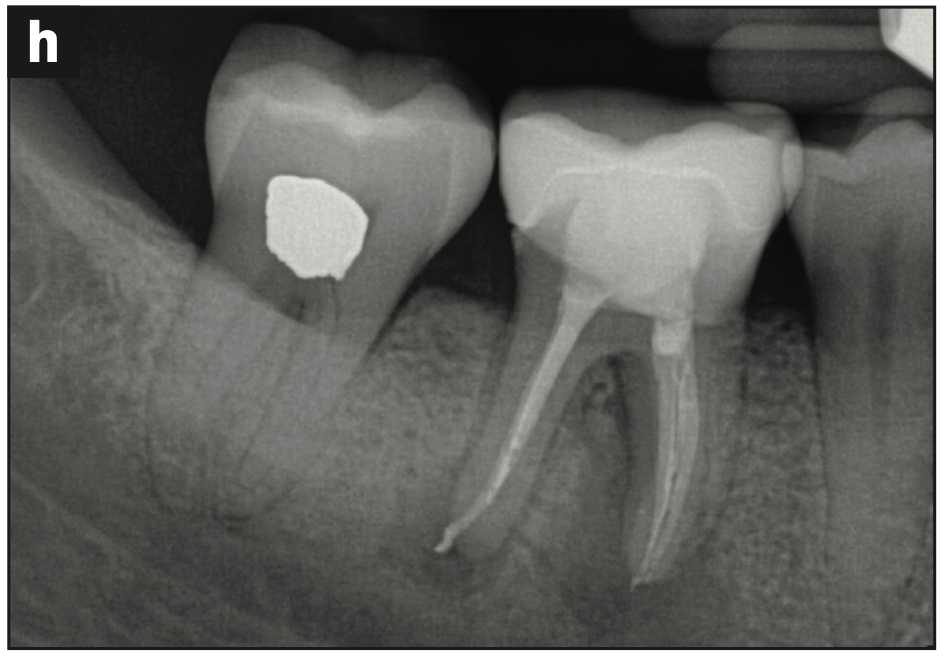
Figure 2h. Immediate post-op off-angle radiograph of tooth No. 30.
As stated earlier, followup is the key to understanding the healing process in endodontics. I saw her back in my chair at her one-year post-op. She had almost completely regenerated all of her bone (Figure 2i).

Figure 2i. One-year recall radiograph.
This patient does have a bit more healing to do, but this will continue to happen with more time. She has made remarkable progress for a lesion of this size, which extended into the furcal area. All that means is that it may take a bit longer to heal. Bone is slow to grow, so when you see a lesion of this magnitude and shape, it may take a few years to fully reconstitute with bone. “Bone can grow” is another empowering belief that I encourage each of us to embody in our practices in order to fully serve our patients.
Tooth-saving belief No. 2: J-shaped radiolucencies may be restorable.
COMMON BELIEF NO. 3: WHEN A CANAL CAN’T BE SEEN ON a CBCT, IT MEANS IT’S NOT THERE
It is generally accepted that the MB2 canal of a maxillary first molar is one of the hardest canals to find and treat in the world of endodontics. Cone-beam technology has no doubt been a game-changer for me with respect to this canal. But it can also be a trap if we are not prepared to read the scans correctly.
Finding the proper support in reading these scans can also be a challenge after we have invested in CBCT technology, so I want to share a few secrets that I have learned, hoping you will have an easier time succeeding.
An MB2 Canal Tooth Story
This 42-year-old male patient was in need of a root canal due to a high level of pain. His pre-op radiographs showed a deep composite restoration on tooth No. 2 (Figures 3a and 3b). His endodontic diagnostic tests revealed that he had lingering pain to cold and tenderness to percussion. All other testing was within normal limits. I diagnosed tooth No. 2 with symptomatic irreversible pulpitis and symptomatic apical periodontitis.

Figure 3a. Pre-op periapical radiograph of tooth No. 2.
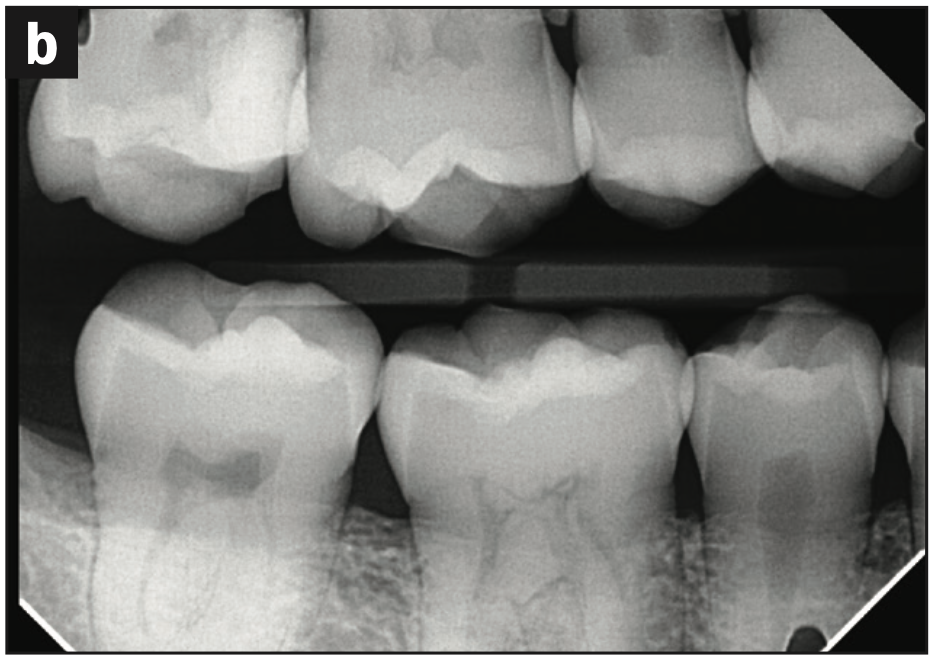
Figure 3b. Pre-op bite-wing radiograph of tooth No. 2.
Before I start any root canal, I always like to understand the internal canal anatomy of a tooth prior to the procedure. Therefore, I took a cone-beam scan (Figures 3c to 3e).
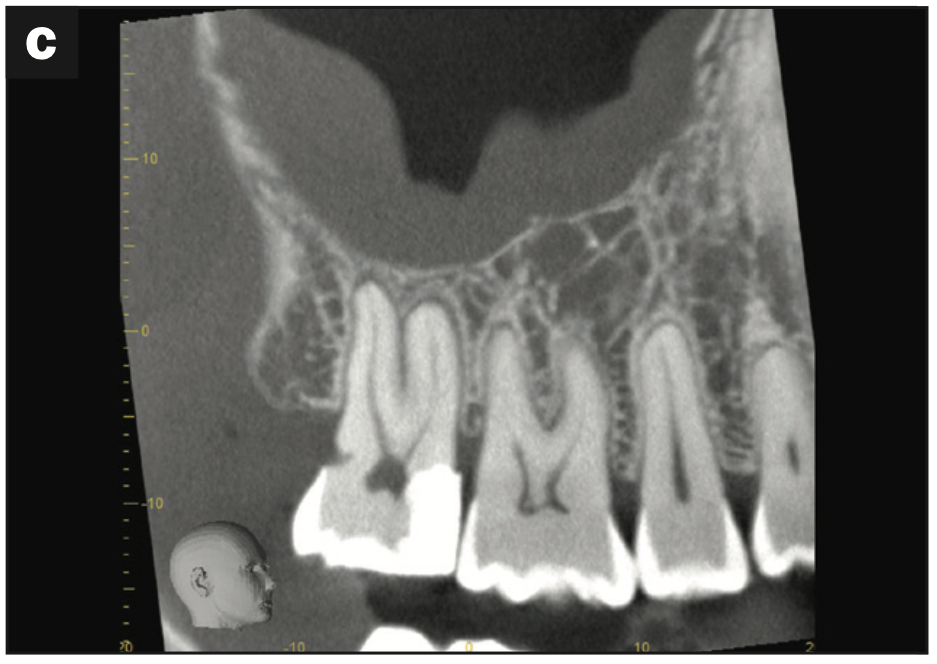
Figure 3c. Pre-op sagittal CBCT view of tooth No. 2.

Figure 3d. Pre-op axial CBCT view of tooth No. 2.
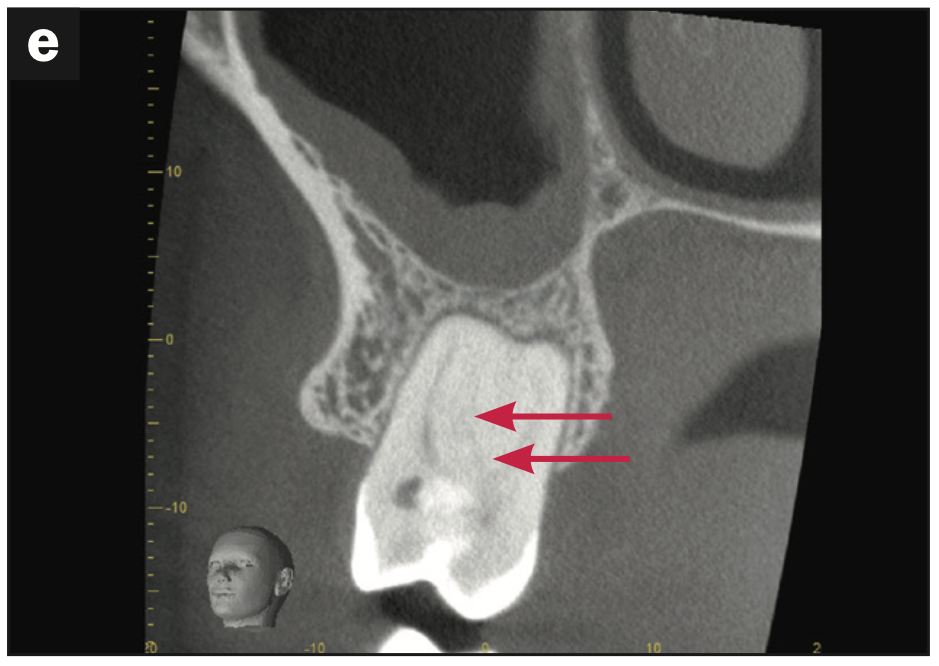
Figure 3e. Pre-op coronal CBCT view of tooth No. 2.
The axial view of the CBCT scan is where a dentist could easily get stumped (Figure 3d). When looking at tooth No. 2, it appears as if there are only 3 canals: the MB, DB, and P canals. However, when we look at the connecting root of the MB canal to the P canal, there is definitely more space that could house a teeny, tiny canal—even though you can’t actually see a fourth canal on the scan.
It is really important to look at your cone-beam scan in all of its planes. In these situations, I particularly like to look at the tooth in the coronal view (Figure 3e).
Imagine a line going through the MB orifice and the P orifice (from the axial slice). This creates the coronal slice that you are seeing (Figure 3e). And now we can see that there is an MB2 canal that could not be seen as clearly in the axial view (Figure 3d).
What did this tell me about this case, even before I accessed the tooth? It told me that this MB2 was going to be a tough one to find.
If we look at the axial view alone, it would be so easy to believe that there is no MB2 at all in this case. Unfortunately, that would have resulted in a root canal failure in the future, which neither the dentist nor the patient would want to happen! That’s why the thought that canals that can’t be seen on a CBCT scan simply aren’t there is ultimately a false belief that each of us needs to examine.
Remember the 2 cardinal rules of root canals: Root canals only work when we (1) find all the canals and (2) get to the end of every canal.
As a side note, this may be a great way to perform a risk assessment and see if this is a case that you want to take on in your practice or refer to a specialist. In my opinion, this type of canal configuration is one of the hardest to treat.
I am incredibly grateful that, thanks to my CBCT scanner, I can understand the difficulty level of the canal’s anatomy before I even get inside. This allows me to have a more meaningful conversation with my patients, and it also manages their expectations throughout the process of their treatment.
With all of this additional information and guidance from my cone-beam scan, I was able to take this case to completion with confidence that I was addressing the entire tooth (Figures 3f to 3h).
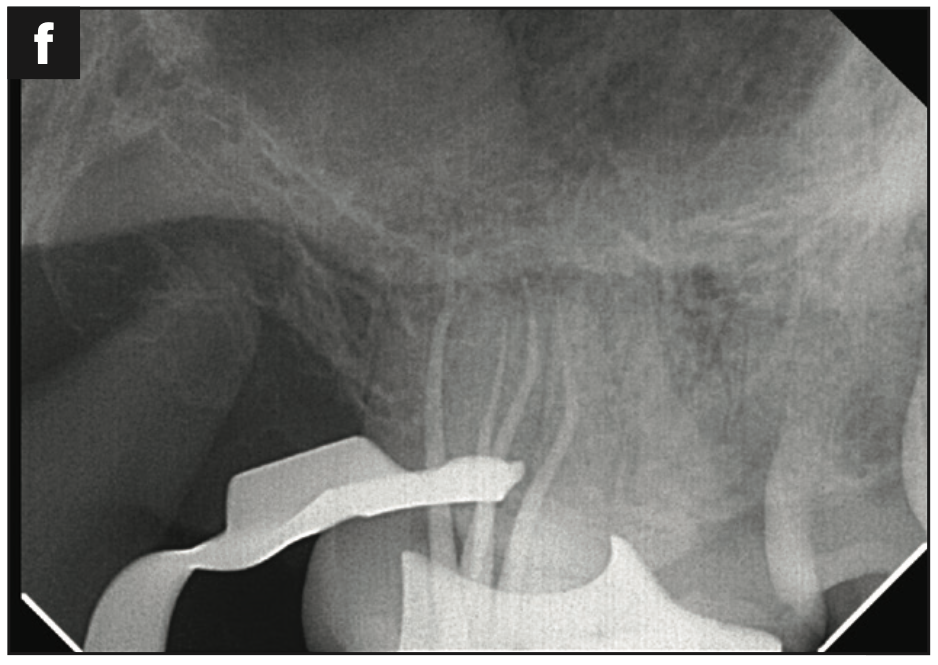
Figure 3f. Conefit radiograph of tooth No. 2.
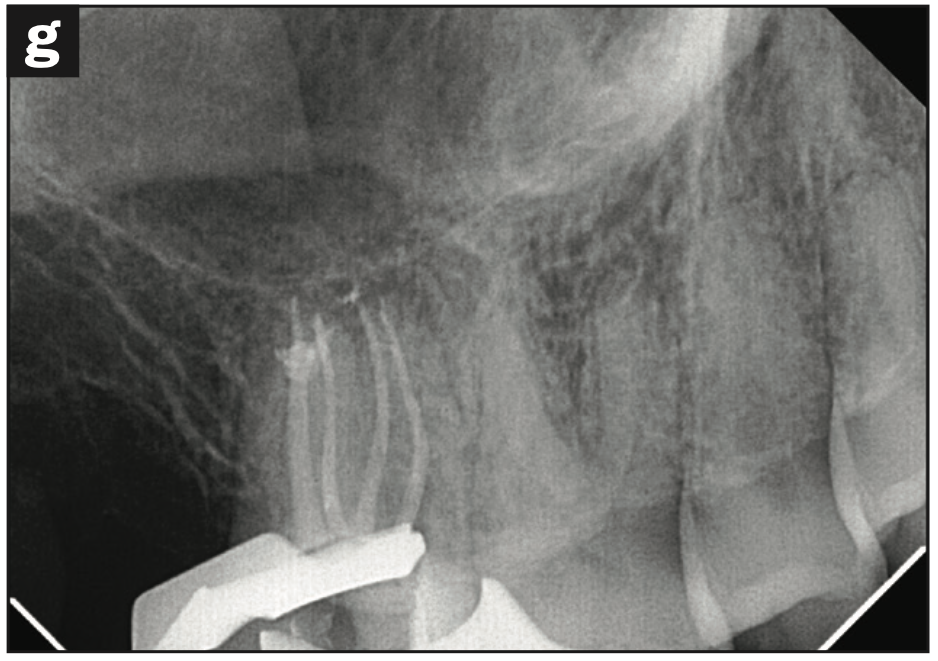
Figure 3g. Backfill radiograph of tooth No. 2.
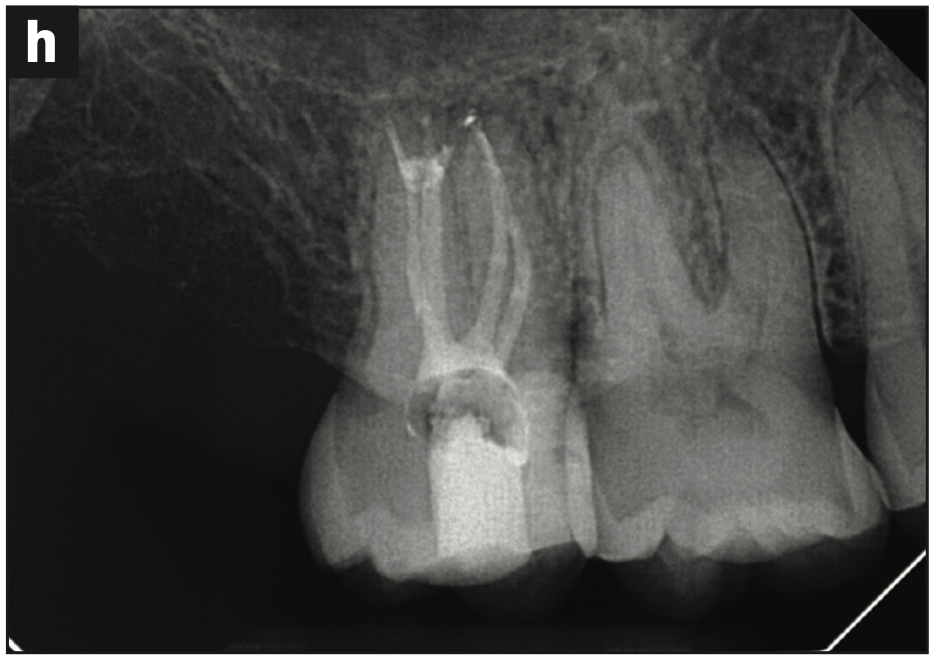
Figure 3h. Immediate post-op radiograph of tooth No. 2.
I hope that we’ll collectively adopt a new empowering belief that can lead to saved teeth: that the MB2 canal is almost always there, even if it isn’t easy to see. It’s better to assume it is than to risk a failed root canal and re-treatment.
Tooth-saving belief No. 3: The MB2 canal is almost always there, even if it isn’t easy to see.
COMMON BELIEF NO. 4: WHEN A TOOTH IS STILL SYMPTOMATIC AFTER ROOT CANAL THERAPY, THE TOOTH MUST BE CRACKED
One of the most frustrating aspects of being an endodontist is when you complete a picture-perfect root canal and that tooth still bothers the patient afterward. It doesn’t happen very often, but when it does, it can feel so defeating.
The uncertainty as to why that tooth is still giving our patients some pain can be frustrating. The typical explanation I have heard dentists give patients is that the tooth is cracked and now needs to be extracted.
But if we really think about it, this determination doesn’t ultimately serve our patients. Most of the time in these scenarios, the tooth is not cracked, but rather there is still some bacterial contamination in the tooth. So, my recommendation is to re-treat the root canal before we condemn the tooth. Consider this—would you extract your own tooth or your child’s tooth, or would you give it another chance?
This same clinical scenario has happened to me in my own practice, and my first instinct is to redo my own work. When the patient still feels something when he or she taps on that tooth, I always offer to try again to see if re-disinfecting the tooth’s canals helps the patient. Happily, it works about 80% of the time and the patient feels better.
The key is not to give up on your patient’s tooth when it’s savable. It’s totally okay to try again. Re-treating my own root canals has taught me many lessons, has changed my tooth beliefs permanently through years of evidence, and has made me a better clinician. I now understand root canal anatomy better than ever before, and I appreciate that the internal anatomy can really limit what we can do with traditional root canal therapy.
This has encouraged me to invest in additional technology, such as the GentleWave System (Sonendo), which can elevate my current root canal experiences and outcomes.
Examples of Root Canal Re-treatment Success Stories
Figure 4 shows a few post-op radiographs of tooth stories that demonstrate what I mean about root canal anatomy.
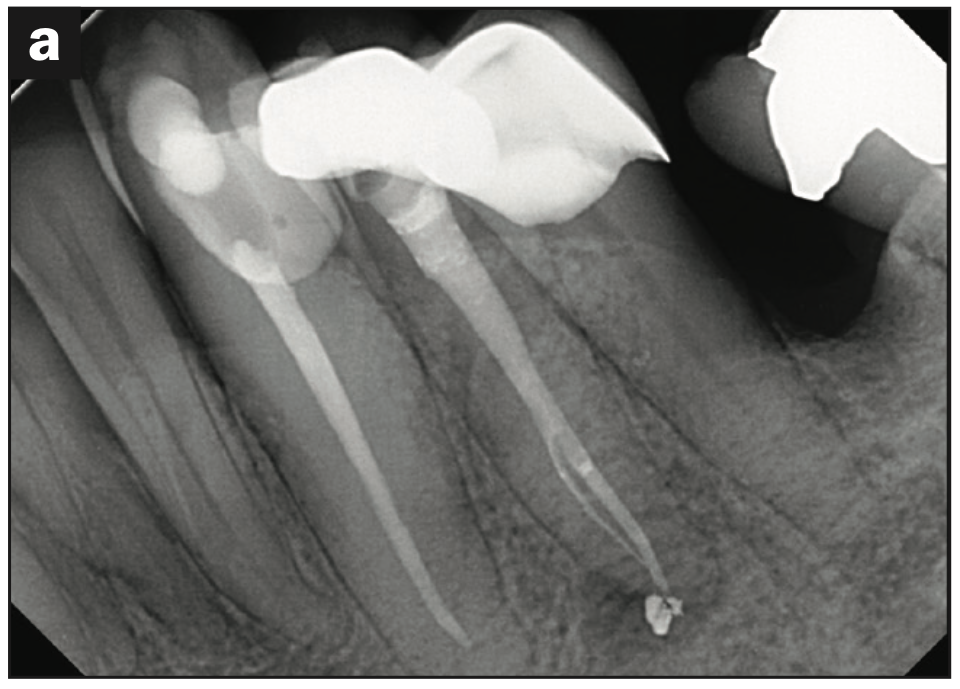
Figure 4a. Post-op radiograph of tooth No. 21 (the smaller canal was not instru- mented with a rotary file, only activated irrigation via the GentleWave System [Sonendo]).
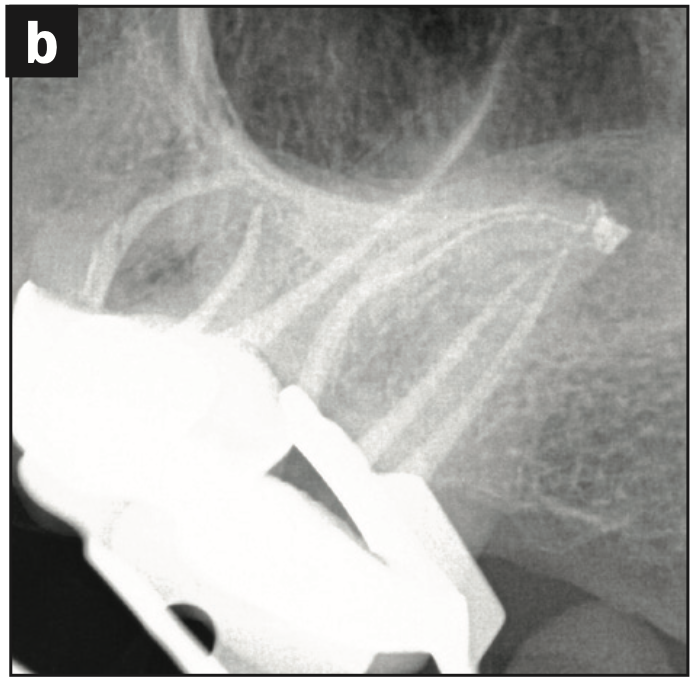
Figure 4b. Immediate post-op radiograph of tooth No. 15 (the smaller MB2 canal was not instrumented with a rotary file, only activated irrigation via the GentleWave System).
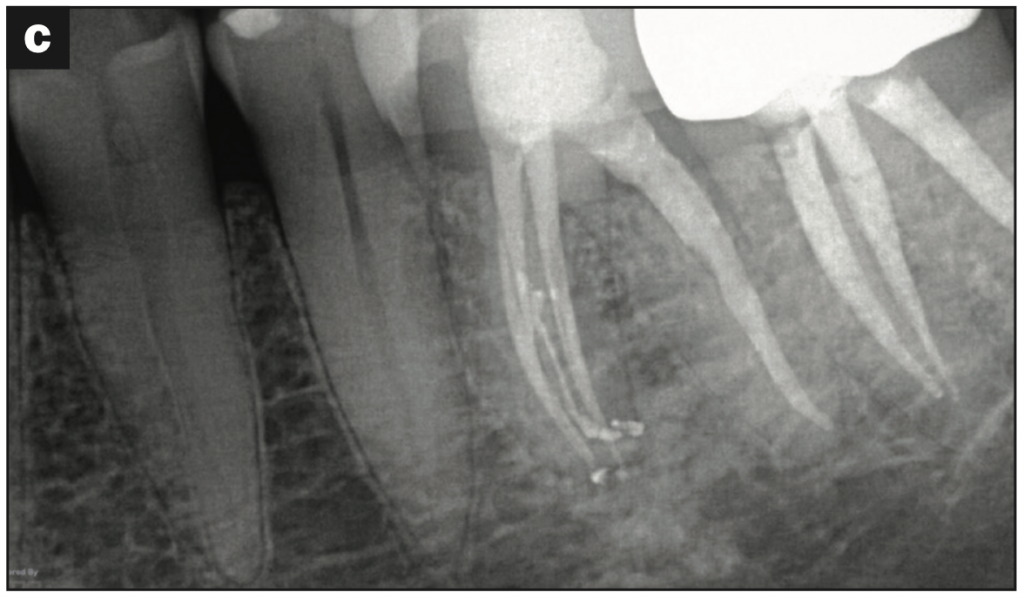
Figure 4c. Immediate post-op radiograph of tooth No. 19 (the smaller middle mesial canal was not instrumented with a rotary file, only activated irrigation via the GentleWave System).
These teeny tiny canals are areas where no rotary file can go—and they didn’t in these cases—which makes mechanical instrumentation difficult.
I treated all of these cases with GentleWave technology. This has solidified my belief that irrigation is instrumentation, and that makes it a crucial part of the endodontic future. It’s a huge paradigm shift, and it’s time to believe in it.
So, when we are in this situation, remember the new belief that teeth that are symptomatic after a root canal may not be cracked but just need re-treatment. That is because there could be a tiny canal somewhere that is still harboring a little bit of bacteria.
It’s okay if you don’t have the same technology at your disposal, but my purpose is to bring awareness into your life so you know where to turn to take the next step to help your patients. Maybe this means you treat the tooth, or maybe this means you refer to a specialist with that technology for re-treatment before you extract the tooth. Remember, it’s all about saving the tooth, and that only happens if we give it a chance.
Tooth-saving belief No. 4: Symptomatic teeth after root canals may not be cracked and may need re-treatment.
OLD BELIEFS GIVE WAY TO NEW, EMPOWERING, TOOTH-SAVING BELIEFS
My intention with these tooth stories has been to bring all of us hope that we can save more teeth and to inspire us to think and evaluate carefully before we extract.
I encourage us to think twice before taking a tooth out and to embrace my motto in life, which is #GiveTeethAChance.
When we do, we’ll find that:
- “Big lesions don’t heal” becomes “lesion size is not a determinant of healing ability.”
- “The J-shaped radiolucency means the tooth is fractured and needs to be extracted” becomes “the J-shaped radiolucency is not synonymous with a root fracture.”
- “A probing equates to a root fracture and, therefore, a non-restorable tooth” becomes “a probing can simply mean that the body has found the pathway of least resistance, and that tooth can be saved.”
- “Bone doesn’t grow back” becomes “bone can regrow, but it is slow, so have patience.”
- “When a canal can’t be seen on a CBCT scan, it’s not there” becomes “look at your cone-beam scan in all of its planes, and assume that the MB2 is almost always there.”
- “When a tooth is still symptomatic after root canal therapy, it must be cracked” becomes “when a tooth is still symptomatic after root canal therapy, some of the infection may have been missed, and a re-treatment will lead to a good outcome.”
These are not the only situations where teeth that are typically extracted can be saved. I’ve shared specific situations because they’re very common and because I also want us to start seeing a pattern. If there’s one message I hope dentists take away from this article, it’s this final tooth-saving belief: You are a tooth saver and a tooth healer if you allow yourself to be. You have the ability to save teeth, even in scenarios in which you didn’t think it was possible. It only requires your belief.
I hope you are feeling excited and that you are already starting to believe in the ability of teeth to be saved. Most of all, I hope you are ready to take on the identity of a tooth saver.
I promise that the more we start to cultivate these new, empowering, tooth-saving beliefs and truly understand the power of our human bodies to heal, the more we can create better outcomes that lead to better lives for patients around the world.
ABOUT THE AUTHOR
Dr. Chopra is a board-certified endodontist, TEDx speaker, Forbes contributor, author, endodontic instructor, and founder of Ballantyne Endodontics in Charlotte, NC. Through her award-winning endodontic CE course, E-School, she teaches tangible lessons to make root canals simple. She can be reached at soniachopradds.com or soniachopradds.com/e-school, or via the Instagram handle
@soniachopradds.
Disclosure: Dr. Chopra is a KOL for Sonendo. She did not receive compensation for writing this article.












