INTRODUCTION
In this time of uncertainty and fear due to the COVID-19 pandemic, the need for practice preservation and practice modification in the aftermath of this pandemic is critical to everyone’s future.1 After discussions with Dr. Damon Adams, editor-in-chief of Dentistry Today, we were invited to share our efforts and experiences to date as we navigate our way through these uncharted times. Our profession has respected the state and federal requests for closure of our offices to mitigate the spread of the virus. We closed our offices on March 16 and are still only caring for emergency patients at the time of this writing on April 13. Our thoughts expressed in this article reflect this time frame, and we know that the situation is still fluid with an ever-growing body of knowledge related to the SARS-CoV-2 virus being reported almost daily. What we know for certain at this time is that the abrupt stop to patient care created a twofold challenge going forward: How do we keep everyone safe as we re-enter patient care, and how do we restore financial stability to our practices?
Our Initial Actions
Like many of you, our efforts during the first 2 weeks of office closure were focused on establishing lines of credit with our banking institutions and applying for U.S. Small Business Administration (SBA) loans (the Paycheck Protection Program and Economic Injury Disaster Loan). Our entire office staff was placed on “leave of absence” so that our employees could receive short-term unemployment benefits from our office unemployment account rather than utilizing their personal unemployment insurance (UI) accounts. It was going to be a race between receiving SBA benefits or unemployment benefits. Anxiety levels were high. Each employee was assured that his or her position within the team was secure. Letters from our labor attorney verified their statuses for their applications to the UI state office.
 |
We kept in touch with our patients and staff through text messages, phone calls, and “weekly update emails,” which outlined protocols for emergency treatment and provided preventive strategies against the COVID-19 virus. Additionally, the patients were given preventive oral health recommendations during their interrupted oral care. The weekly updates proved to be reassuring for all and assured our patients and staff that we were there for them.
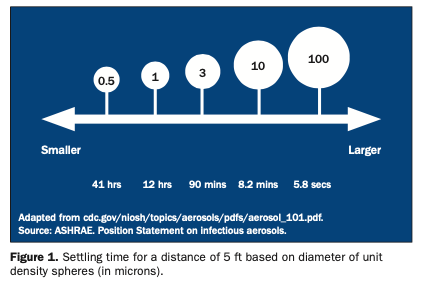
Once we were comforted that our team and financial needs were managed, we shifted our focus to the practice. A skeleton crew was established to assist in patient communication and emergency care management. Key members from each department were identified for their leadership within the practice and their ability to maintain social distancing when not in the practice. The ADA algorithm provided a good framework for the emergency triage of patients requesting care2 (Figure 1). We reconfigured job descriptions to allow appropriate tasks to be done from home with new online access. Entire weeks turned into months of patient care that were either canceled, postponed, or rescheduled for the future. Seeing the entire office schedule go blank was utterly shocking.
As time passed, the reality of this “new normal” became clearer. We needed to determine immediate appropriate levels of infection control to keep everyone safe and establish guidelines for the future. The calls for emergency needs were increasing, further augmented with emergencies from interrupted care. Everyone needed to be treated as if they were a COVID-19 carrier because we knew that asymptomatic patients could still carry the virus and be infectious. Therefore, we needed to place additional barriers of protection between all patients and health providers to protect against transmission in both directions. The ADA issued interim recommendations for dental offices, which provided some direction and illustrated the high-risk position that all dental professionals occupied.3
 |
 |
| Figure 2. Before: dental supplies storage area prior to space reallocation. | Figure 3. After: new personal protective equipment (PPE) changing area after space and supply reallocation. |
 |
 |
| Figure 4. A clinical setting with additional protective barriers. | Figure 5. An operator with PPE, including an N95 mask, overlaid with a surgical mask and facial shield. |
 |
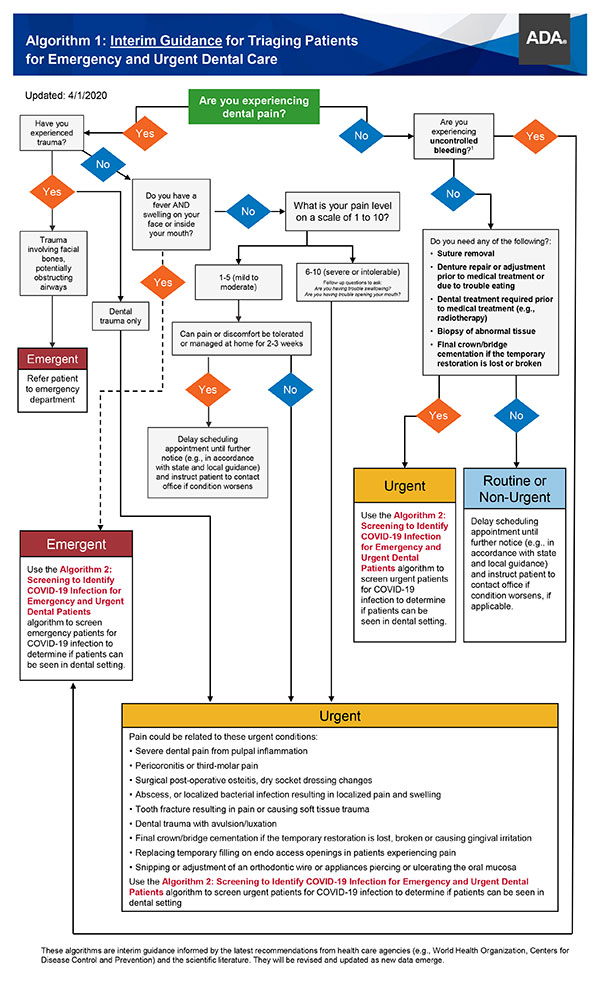
| Figure 6. Aerosol diagram of coughing and sneezing.10 |
Our Protocols for Emergency and Urgent Care
It became clear that, as healthcare workers, dentistry is a high-risk profession, primarily due to our proximity to the patients and the aerosols that are routinely created with our work.4 Until there is a sure way to protect everyone from this highly transmittable virus, we needed to upgrade the “Universal Precautions” to “Transmittable Disease Standards” as described by the CDC.5 The following are the protocols that have been established for our office for emergency and urgent patient care. We utilized information from numerous sources3,5 as well as our own opinions.
 |
| Figure 7. Utilizing the clinical microscope allows sitting 10 in farther from the patient, decreasing the aerosol volume by a factor of 8. The extra plastic drape extending behind the patient provides additional aerosol and splatter protection. (Plastic drape recommendation courtesy of Wayne Remington, DDS.) |
1. Patients are screened for medical history, current symptoms, travel history, and compliance to social distancing recommendations for a minimum of 14 days.2
2. An entrance to the building that minimizes exposure to other patients was identified.
3. Patient appointments are coordinated to eliminate patient overlap.
4. Upon arrival, patient temperatures are taken, and health and travel histories are reconfirmed. Patients are provided with a face mask to be worn during their time in the office and when exiting after treatment.2
5. All patient magazines and books have been removed from all operatories.
6. Patients are provided with a long, disposable drape in the operatory, rather than the smaller, traditional bib.
7. Patients pre-rinse for 60 seconds with 1.5% hydrogen peroxide, as advised by the ADA, to decrease viral and bacterial loads.3
8. A patient mask/eye shield is used, whenever possible, during treatment.
9. All surfaces are routinely disinfected before and after patient contact (door handles, counter tops, pens, etc).6
10. Hallways and open spaces are regularly sprayed with a disinfectant aerosol or fogged with disinfectants such as hypochlorous acid (ie, Dentaqua).7
11. Air purifiers are placed in all rooms and open spaces.6,8
12. Newly established personal protective equipment guidelines are used for all team members3,6:
a. The staff has a designated entry point leading directly to a changing station to remove street clothes and replace them with the new clinical attire (Figures 2 and 3).
b. Scrubs are worn by all clinical and laboratory staff, along with a clinical jacket covered by an additional disposable gown to be discarded between patients (Figure 4).
c. Facial protection includes an N95 mask overlaid with a customary surgical mask and covered by a plastic facial shield (Figure 5). The coverage of the N95 mask allows for repeated use by the clinician if N95 masks are in short supply. Head protection is augmented with a surgical cap.
13. Oral isolation and suction devices are utilized for all aerosol-producing procedures (eg, rubber dams, Isolite 3 [Zyris], and Nu-Bird).9 Currently, hand instrumentation is recommended over ultrasonic instrumentation for hygiene procedures (Figure 6).
14. Clinical microscopes are protected with a plastic barrier, along with an additional plastic drape extending from the oculars to protect the operator from aerosols. The use of the clinical microscope minimizes the spherical volume of aerosol spray (Figure 7).
15. Additional methods to control cross contamination include:
a. All paper documents are left out of the operatory as viruses can remain viable on surfaces for 3 to 72 hours.11
b. All exposed ancillary clinical equipment (eg, loupes/headlamps, intraoral scanners, keyboards, etc) are disinfected after contact.6,11
c. All efforts are made to pre-dispense materials to minimize cross contamination (eg, cement, composite, and impression materials). Additionally, a secondary assistant may be utilized to maintain sterility.
16. All post-treatment activities and transactions are done in the patient’s operatory.
17. Laboratory dental technicians follow the same protocols as the clinical staff when entering and leaving an operatory while also maintaining strict infection protocols within the laboratory.
CLOSING COMMENTS
One thing is for certain: As the future continues to evolve and our profession identifies new issues to be addressed, the impact of COVID-19 will have long-lasting effects on the dental practice. The positive outcome is that these new protocols for sterilization and aerosol control will better protect us, our dental office and treatment teams, and our patients into the next decades. A sense of responsibility needs to be established within each patient as to his or her need for excellent biofilm control; proper use of fluorides; and optimal lifestyle choices in food, exercise, and habits.
When faced with adversity, it is critical that we take ownership of the issues facing us. Our profession and community are experiencing new challenges as a direct result of the COVID-19 pandemic, forcing us to critically examine our best practices and evolve them into a superior standard of care.
References
- World Health Organization (WHO). Coronavirus Disease 2019 (COVID-19) Situation Report 32. February 21, 2020.
- American Dental Association. ADA Interim Guidance for Management of Emergency and Urgent Dental Care. Updated April 1, 2020.
- American Dental Association. ADA Interim Guidance for Minimizing Risk of COVID-19 Transmission. Updated April 1, 2020.
- Sabino-Silva R, Jardim ACG, Siqueira WL. Coronavirus COVID-19 impacts to dentistry and potential salivary diagnosis. Clin Oral Investig. 2020;24:1619-1621.
- Centers for Disease Control and Prevention. Coronavirus disease 2019 (COVID-19). Dental settings. Revised April 7, 2020. Accessed April 16, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/dental-settings.html.
- US Department of Labor, Occupational Safety and Health Administration. Guidance on Preparing Workplaces for COVID-19. OSHA 3990-03 2020. Accessed April 16, 2020. https://www.osha.gov/Publications/OSHA3990.pdf.
- US Environmental Protection Agency. List N: Disinfectants for use against SARS-CoV-2. Accessed April 16, 2020. https://www.epa.gov/pesticide-registration/list-n-disinfectants-use-against-sars-cov-2.
- Peng X, Xu X, Li Y, et al. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci. 2020;12:9.
- Dahlke WO, Cottam MR, Herring MC, et al. Evaluation of the spatter-reduction effectiveness of two dry-field isolation techniques. J Am Dent Assoc. 2012;143:1199-1204.
- Froum S, Strange M. COVID-19 and the problem with dental aerosols. Perio-Implant Advisory. April 7, 2020.
- van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564-1567.
Dr. Paquette is a past president of the American Academy of Esthetic Dentistry and the Pacific Coast Society of Prosthodontics (PCSP). She is recognized nationally and internationally as a leader in aesthetic dentistry, prosthodontics, and implant dentistry. She is a Diplomate of the American Board of Prosthodontics and a Fellow of the American College of Prosthodontists. She holds fellowships in the International College of Dentists (ICD), the American College of Dentists (ACD), and the Pierre Fauchard Academy (PFA). She is also a member of the Academy of Osseointegration. Dr. Paquette has authored numerous research and clinical articles on her areas of expertise and co-authored several textbook chapters. She is co-executive director of the Newport Coast Oral Facial Institute (NCOFI). Dr. Paquette can be reached at jmpaquette@ncofi.org.
Dr. Sheets maintains a full-time private practice in Newport Beach, Calif, for aesthetic rehabilitative dentistry. She is an international educator, a clinician, an author, and a researcher. She is a Fellow of the AGD, ACD, ICD, PFA, and the Academy of Dentistry International. Dr. Sheets is founder and co-executive director of the NCOFI, a non-profit international teaching and research center for dentists and dental technicians, in Newport Beach, Calif. She and James C. Earthman, PhD, professor of material science & engineering and biomedical engineering at the University of California, Irvine, are leading research on quantitative percussion diagnostics for teeth and implants. They hold numerous US and international patents on this groundbreaking technology. Dr. Sheets can be reached at cgsheets@ncofi.org.
Dr. Wu is on the executive council for the PCSP and a past president of the Academy of Microscope Enhanced Dentistry. She is also a member of the ADA, the California Dental Association, and the Orange County Dental Society (OCDS). She was a board member of the OCDS in 2011 and a senior delegate in 2012. Currently, Dr. Wu is a partner in the Sheets, Paquette and Wu Dental Practice and co-executive director with NCOFI, a non-profit international teaching and research center. She is also actively involved with several research projects on dental implants and materials and has published articles in several dental journals. Dr. Wu can be reached at jcwu@ncofi.org.
Disclosure: The authors report no disclosures.
Related Articles
Tennessee Reopens Practices While Massachusetts Waits
COVID-19 Is Changing Dentistry, and Our Office Is Changing With It
AGD Releases Guidance for Returning to Work