INTRODUCTION
As a field, surgical periodontics has seen many incarnations during the decades, beginning with resections of gingiva and bone and then progressing to flap surgery, with osseous resection and recontouring, and, finally, regenerative procedures. All had the same goal in mind: pocket reduction/elimination and the restoration of periodontal health. While the first 2 left something to be desired with regard to patient comfort, all of these techniques achieved their desired outcomes with regeneration surgery being the obvious “Holy Grail.” This was due to its ability to reclaim lost periodontal structure, both bone and connective tissue. So what’s the “Holy Grail” of the “Holy Grail?” In my opinion, it is laser-assisted new attachment procedure (LANAP).
In my previous article, “Advancing the Standard of Care With the LANAP Protocol,” published in the April 2013 issue of Dentistry Today, a summary of the procedure and several cases were shown. To reiterate, LANAP (Millennium Dental Technologies) utilizes the free running pulsed Nd:YAG laser as a part of its protocol. The outright benefits of LANAP for achieving regeneration cannot be overlooked or ignored when presenting a treatment plan to a patient. LANAP is a less invasive procedure, eliminating the need for the cutting and suturing that is part of the traditional and regenerative osseous surgical procedures. It initiates and stimulates the patient’s own cellular and tissue response to restore lost bone and connective tissue attachment without the introduction of foreign substances, whether they are bone, membranes, or growth factors. This was proven histologically by Dr. Ray Yukna’s study1 that clearly demonstrated regeneration of the supporting periodontal apparatus in human specimens. In my office, we have seen undeniable clinical and radiographic proof of LANAP’s capabilities in many cases, several of which will be presented here.
CASE REPORTS
Case 1
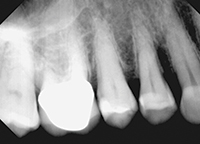
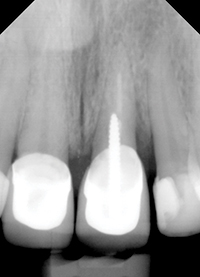
Findings—A 57-year-old female was referred to our office by her general dentist for evaluation and treatment of the maxillary right first premolar. Clinical examination indicated pocketing of 8.0 mm along the entire palatal aspect of the tooth, extending into the mesial interproximal area. This corresponded to 5.0 mm of attachment loss. The defect could be easily seen on the radiograph (Figure 1), matching the clinical impression. The problem was further compounded by secondary trauma from occlusion in both centric relation and lateral excursions, causing a mobility of 2+.
| CASE 1 | ||||
|
Treatment and Results—A procedure was performed for the maxillary right first premolar utilizing the PerioLase MVP-7 and the LANAP protocol under local anesthetic (Mepivacaine HCl 3% without vasoconstrictor). Postoperatively, the patient was placed on Clindamycin 150 mg (No. 28, 4 times a day for one week) and chlorhexidine rinse 0.12% (Periogard [Colgate]) (30 seconds, twice a day for 2 weeks).
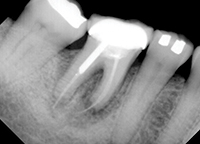
At the 2-week postoperative visit, the mobility of the premolar was already reduced to a +, and it was completely immobile at the 4-week postoperative visit. Clinical probing was not done until the 6-month evaluation, at which time a radiograph was also taken (Figure 2). Complete bone fill of the defect was evident, with corresponding probing depths of 2 mm at the former diseased sites equating to a clinical attachment gain of 6.0 mm.
Case 2
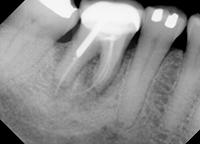
Findings—A 53-year-old female was referred to our office by her general dentist for treatment of generalized severe periodontitis. Of particular concern was a large intrabony defect present on the mandibular right third molar. This defect extended from the mesial aspect of the tooth to the mid-lingual aspect of the tooth (Figure 3). This tooth served as a terminal abutment for a long-span fixed bridge, so its retention was imperative.
Treatment and Results—The tooth was treated as part of the LANAP protocol for the entire dentition. The PerioLase MVP-7 was utilized with the LANAP protocol under local anesthetic (Lidocaine HCl 2% with 1:100,000 epinephrine). During the procedure, the actual condition of the molar was found to be worse than expected. Bone loss was found to be extending beyond the apex of the mesial root, and from the mesial interproximal to the midlingual aspect of the tooth. Postoperatively, the patient was placed on penicillin VK 500 mg (No. 28, 4 times a day for one week) and Periogard rinse 0.12% (30 seconds, twice a day for 2 weeks).
| CASE 2 | ||||
|
The patient returned in 8 months for a postoperative clinical and radiographic examination of the molar. Complete bone fill of the osseous defect was seen on the radiograph (Figure 4) with corresponding pocket depths of 4.0 to 7.0 mm. This was a significant improvement over the original, nearly hopeless clinical presentation.
Case 3
Findings—A 61-year-old female was referred to our office by her general dentist for evaluation and treatment of a periodontal abscess on the maxillary left central incisor (Figures 5 and 6). Clinical examination revealed a mobility of 2 on the tooth along with pocketing of 9.0 mm along its palatal aspect, extending through the distal interproximal to the distofacial line angle. A fracture was suspected, but every effort was to be made to salvage the tooth.
 |
 |
| Figure 5. Pre-op photo showing tooth No. 9. | Figure 6. Pre-op radiograph showing tooth No. 9. |
 |
 |
| Figure 7. During LANAP on tooth No. 9 (facial). | Figure 8. During LANAP on tooth No. 9 (lingual). |
 |
 |
| Figure 9. One-month post-op photo (facial). | Figure 10. One-month post-op photo (lingual). |
 |
| Figure 11. One-month post-op radiograph. |
Treatment and Results—A procedure was performed for the maxillary left central incisor utilizing the PerioLase MVP-7 and the LANAP protocol under local anesthetic (Lidocaine HCl 2% and 1:100,000 epinephrine) (Figures 7 and 8). Postoperatively, the patient was placed on penicillin VK 500 mg (No. 28, 4 times a day for one week) and Periogard rinse 0.12% (30 seconds, twice a day for 2 weeks).
The patient returned in one month for both clinical and early radiographic evaluation. The gingival condition had already resolved and returned to a state of health with mobility on the tooth reduced to + (Figures 9 and 10), and there even appeared to be some bone fill of the defect (Figure 11), although no probing could be done at this time in order not to disturb the regenerative process.
Case 4
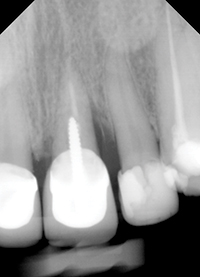
Findings—A 62-year-old female was referred to our office by her general dentist for extraction of the mandibular right first molar and bone grafting. This was to be followed by implant placement in 6 months. Clinically, the tooth was depressible in the socket with a fistula emanating from its buccal aspect. A large area of infection and root resorption was evident in the radiograph (Figure 12). After discussion with the patient, it was decided to attempt to save the tooth using the LANAP protocol since an extraction, followed by bone grafting and implant placement, could always be done if the treatment failed.
| CASE 4 | ||||
|
Treatment and Results—A procedure was performed for the molar utilizing the PerioLase MVP-7 and the LANAP protocol under local anesthetic (Articaine HCl 4% and 1:100,000 epinephrine). Postoperatively, the patient was placed on penicillin VK 500 mg (No. 28, 4 times a day for one week) and Periogard rinse 0.12% (30 seconds, twice a day for 2 weeks).
The patient returned at 5 weeks for clinical and an early radiographic evaluation. The fistula was no longer present and the radiograph showed that some bone fill had already occurred (Figure 13); completely unexpected at such an early stage. The tooth has been retained since then.
CLOSING COMMENTS
The PerioLase MVP-7-assisted LANAP protocol is a proven and invaluable tool for the treatment of all case types of periodontitis. It is particularly effective when other treatment modalities are impractical or virtually impossible. It should be, and is in my office, considered the standard of care for the treatment of periodontal disease due to its combination of outstanding results and unparalleled patient comfort.
Reference
- Yukna RA, Carr RL, Evans GH. Histologic evaluation of an Nd:YAG laser-assisted new attachment procedure in humans. Int J Periodontics Restorative Dent. 2007;27:577-587.
Dr. Mangot has maintained a practice limited to periodontics and implants in Clifton, NJ, for the past 23 years. He received his doctor of dental medicine in 1987 and his certificate in periodontics in 1990 from UMDNJ-New Jersey Dental School and is a Diplomate of the American Board of Periodontics. He can be reached at healthygumsnj@gmail.com.
Disclosure: Dr. Mangot reports no disclosures.