Occlusal disease (OD) is a far more destructive disease than most people realize. Dr. Peter Dawson considers OD the main cause of tooth loss.1 If we accept that statement, it would mean that OD is more destructive than caries and periodontal disease! Historically dentists are very good at diagnosing caries, and are getting better at diagnosing periodontal disease.
Although OD is such destructive disease, it is sad to see that very few dentists actually diagnose OD on every patient during a comprehensive evaluation. One reason this happens is because most dentists are not experts in occlusion; this is despite the fact that dentists alter occlusion every day when they restore or replace teeth. The primary reason dentist are not experts in occlusion is because most available occlusion courses, although good and comprehensive, make occlusion to complicated and the occlusal diagnosis to burdensome and difficult to implement for a busy clinician. The purpose of this article is to present a very simple and methodic system to implement occlusal diagnosis using and understanding the 7 signs and symptoms of OD.
 |
|
Figure 1. This patient was aware of grinding and wore a night guard. However, he reported that teeth continue to wear away. He had many symptoms of occlusal disease (OD). |
 |
| Figure 2. The same patient, after an expensive full-mouth rehabilitation. |
 |
| Figure 3. The patient was surprised that he was never informed he had a pathological occlusal condition, despite the fact he had severe OD symptoms. |
 |
| Figure 4. Abfractions were previously repaired. Note the typical lack of canine guidance. |
 |
| Figure 5. Patient had abfractions and tooth sensitivity. Observe the group function. |
 |
| Figure 6. Right maxillary molar with severe bone loss associated with secondary occlusal trauma. |
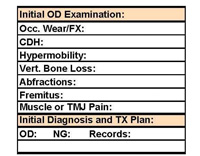 |
| Figure 7. A simple section dedicated to the recording of the 7 signs and symptoms of occlusal disease. |
EFFECTS OF OCCLUSAL DISEASE
Every single day that we practice dentistry we treat patients who have signs and symptoms of OD, and in many cases this disease has mutilated our patients’ teeth to the point which requires restorations or extensive rehabilitation (Figures 1 and 2). In some cases, the signs and symptoms of OD are more chronic in nature. OD can also be extremely debilitating for our patients. For example, patients can have teeth that are so cold sensitive they have to use warm water to brush their teeth, or they must avoid cold foods and beverages. Also, some patients wakeup every day with tired facial muscles, and/or in pain. It is no surprise to any dentist to know that most restorative failures are caused by OD2,3 and most postoperative sensitivity problems are also related to OD.
When understanding how important OD diagnosis and management is to the long-term health of our patient’s dentition and the longevity of restorative work, it is surprising that only a small number of clinicians actually diagnose and educate their patients about OD at every single comprehensive examination. We always diagnose periodontal disease at each examination, and we must diagnose and educate our patient about OD, or the harm can be just as devastating.
OCCLUSION: MAKING IT EASIER
The main reason we do not address OD is because most dentists have a void in their education with regard to OD, as expressed by Dr. Christensen.4 Furthermore, he suggests that many of the available courses and institutes “are so far into nonpractical procedures” complicating and confusing a simple subject. Yes, Dr. Christensen believes it to be a simple subject. I also believe that occlusion is not such a complicated subject. Most courses and institutes tend to have excessively large curricula, which make it expensive and time consuming to get an education on occlusion. Their teachings also tend to be very impractical, especially in regards to the implementation of an occlusal diagnosis.5
The Occlusial Disease Management System was developed by the author to implement diagnosis and treatment of OD using methodic and incremental stages. This system is based on levels of severity and takes into account a patient’s willingness to accept responsibility in treating their own occlusal/tempromandibular disorder pathology. This allows even a busy dentist to be able to implement occlusal diagnosis and therapy on all patients.6
The first stage of the system is a basic occlusal and tempromandibular joint disease (TMJ) screening performed during every comprehensive examination to screen for signs and/or symptoms of OD. A brief dental history form is filled out by the patient to allow for self-disclosure of conditions which may be related to OD, such as headaches or migraines, grinding or clenching, and/or jaw pain. (For a free copy of the form, contact Dr. Ruiz.) With the above information, the dentist can easily add the ability to diagnose OD to the comprehensive examination on every patient. This can be done without adding more than 3 to 5 minutes to the normal examination protocol.
The key to occlusal diagnosis implementation is a methodic and uncomplicated initial differential diagnosis; knowing and using the 7 signs and symptoms of OD.
THE SEVEN SIGNS AND SYMPTOMS OF OCCLUSAL DISEASE
Assessing if the patient has OD is much simpler than most people think. If the patient presents with any one or more of the 7 signs and symptoms of OD, then we can assume the patient has a pathological occlusion (or OD), regardless of the etiology. If the patient does not have any of these signs, then we can assume the patient is well adapted to his or her occlusion, has no pathology, and is not in need of any occlusal therapy.
The 7 signs and symptoms of OD are:
- Pathological occlusal wear and fractures of teeth/restorations—Although controversial, most occlusal wear is multifactorial, a combination of attrition, erosion and abrasion, and tooth paste abuse.7,8 Nevertheless when ever we see excessive occlusal wear, independent of its etiology, we should suspect OD. Also, during our observation, if we see multiple chips on teeth, or small and large fractures of teeth and restorations, this should also make us suspect a pathological occlusion, regardless of it etiology. The etiology of any of these signs can only be determined after a comprehensive occlusal examination with mounted casts, which is part of phase 2 diagnosis. At this point during phase 1, it is sufficient to know that the patient has this sign of OD (Figure 3).
- Cervical dentin hypersensitivity (CDH)—It is absolutely eye opening to understand that most cervical dentin hypersensitivity is caused by occlusal trauma, and the most reliable modality of treatment to get rid of sensitivity is an occlusal equilibration.9 A high percentage of our patients suffer from CDH and are completely unaware that their occlusion is most likely the cause of the problem. In my private practice, I treat all CDH patients with occlusal therapy with an absolute certainty of success. It is also my personal experience that this can be extrapolated to the fact that most postoperative sensitivity is caused by induced occlusal trauma, and that proper occlusal adjustment after a restoration will eliminate most postoperative sensitivity.
- Tooth hypermobility—How often do we find (during our comprehensive examination) molars, especially second molars, that although radiographically appear to have sufficient bone support, have tremendous mobility? This is a clear sign of OD—an unbalanced occlusion which is overloading some teeth. How sad would it be if because of this great mobility we would consider extracting these teeth? Especially if proper occlusal therapy will most likely bring these teeth back to stability?
- Fremitus—Fremitus is the vibration we feel in teeth when the patient “chop-chops” on their natural bite or in maximum intercuspal occlusion. In anterior teeth, this is usually caused by a pathological occlusion, often an envelop-of-function violation. Like hypermobility, it is another sign of a pathological bite.
- Abfractions10-12—These very controversial noncarious lesions are usually caused by pathological lateral forces but, like most diseases processes, these lesions are multifactorial.
They cannot occur in the absence of an acidic environment. Of course, the teeth are often attacked by acidic substances like, sodas, energy drinks, fruit juices, coffee, etc. Whenever I see this lesion, I immediately look for the occlusal etiology and in most cases it is easy to find (Figures 4 and 5). - Vertical bone loss or localized bone destruction (secondary to periodontal disease)13,14—It is well established in the literature that tooth mobility accelerates bone loss on periodontally compromised patients. So, whenever I see a radiographic series which shows generalized periodontal disease, but also shows some teeth with accelerated bone loss, it is usually traceable to teeth with occlusal trauma—one more sign of OD (Figure 6).
- Pain and tired facial and masticatory muscles or TMJ pain15—Pain is the most common symptom dentist associates with a diagnosis of OD. Sore and tired facial and masticatory muscles (that can often trigger headaches) are extremely common complaints, when patients are asked. Often, dentists do not know about these symptoms because patients rarely report them. Patients are often not aware that OD can create such symptoms. (I have intentionally placed this symptom of OD in the last place. This is not because it is not important, but because there are the other 6 symptoms often overlooked and equally as important.)
RECORDING THE OBSERVATIONS: DEALING WITH THE PATIENT
A small and simple section for the diagnosis and recording of OD should be added to any clinical examination sheet. It should list the 7 signs and symptoms, and include space to record any needed follow-up examinations or preventative treatment (Figure 7). (For a free copy of the form, contact Dr. Ruiz.) This should serve as a permanent flag for the clinician who treats the patient, making it obvious that any treatment will be compromised unless occlusal therapy is initiated.
Once any of these signs and symptoms are identified, the dentist will do well to try to connect the patient’s initial complaints with the signs and symptoms discovered. This will help the patient acknowledge their disease. Proper education and motivation is a crucial part of stage 1 diagnosis and is a primary factor in attaining treatment acceptance and clinical success for both restorative and aesthetic treatment. After a presentation of the initial findings, the patient is informed that OD can only be properly treated after a more comprehensive examination and diagnosis is performed. These comprehensive steps will include mounted casts and an advanced clinical occlusal and TMJ diagnosis (phase 2 diagnosis in the OD management system). If the patient refuses phase 2 diagnosis, then one would continue with nonelective procedures and avoid extensive restorative work, which would be compromised by the OD. The patient may also be offered a protective night guard as a basic preventive measure to decrease the damage being caused by OD.
CONCLUSION
By knowing and recognizing the 7 signs and symptoms of OD, spending the few additional minutes necessary to evaluate the presence of them, and adding a small section to record these findings into our examination and diagnosis form, we can easily implement OD diagnosis in any busy practice. As clinicians, we have the obligation to diagnose this destructive disease, which is as costly as caries or periodontal disease. Using this simple method of diagnosing OD, will open our eyes to the widespread prevalence of OD and help us improve care for our patients.
References
- Dawson PE. In: Functional Occlusion: From TMJ to Smile Design. St. Louis, Mo: Mosby; 2007:27-32.
- Ruiz JL. Achieving longevity in esthetic dentistry by proper diagnosis and management of occlusal disease. Contemporary Esthetics. 2007;11:24-27.
- Ruiz JL. Occlusal disease: restorative consequences and patient education. Dent Today. 2007;26:90-95.
- Christensen GJ. Abnormal occlusion conditions: a forgotten part of dentistry. J Am Dent Assoc. 1995;126:1667-1668.
- Christensen GJ, Ruiz JL. Restorative dentistry: current developments and a look to the future. Dent Today. 2008;27:98-102.
- Ruiz JL, Coleman TA. Occlusal disease management system: the diagnosis process. Compend Contin Educ Dent. 2008;29:148-158.
- Grippo JO, Simring M, Schreiner S. Attrition, abrasion, corrosion and abfraction revisited: a new perspective on tooth surface lesions. J Am Dent Assoc. 2004;135:1109-1118.
- Abrahamsen TC. The worn dentition—pathognomonic patterns of abrasion and erosion. Int Dent J. 2005;55:268-276.
- Coleman TA, Grippo JO, Kinderknecht KE. Cervical dentin hypersensitivity. Part III: resolution following occlusal equilibration. Quintessence Int. 2003;34:427-434.
- Telles D, Pegoraro LF, Pereira JC, et al. Incidence of noncarious cervical lesions and their relation to the presence of wear facets. J Esthet Restor Dent. 2006;18:178-183.
- Grippo JO. Abfractions: A new classification of hard tissue lesions of teeth. J Esthet Dent. 1991;3:14-19.
- Ichim I, Schmidlin PR, Kieser JA, et al. Mechanical evaluation of cervical glass-ionomer restorations: 3D finite element study. J Dent. 2007;35:28-35.
- Harrel SK, Nunn ME, Hallmon WW. Is there an association between occlusion and periodontal destruction? Yes—occlusal forces can contribute to periodontal destruction. J Am Dent Assoc. 2006;137:1380-1384.
- Greenstein G, Greenstein B, Cavallaro J. Prerequisite for treatment planning implant dentistry: periodontal prognostication of compromised teeth. Compend Contin Educ Dent. 2007;28:436-447.
- Gremillion HA. The relationship between occlusion and TMD: an evidence-based discussion. J Evid Based Dent Pract. 2006;6:43-47.
Dr. Ruiz is course director of the USC Advanced Esthetic Dentistry Continuum and clinical instructor at USC. Associate instructor and mentor at PCC in Utah, teaching with Dr. Gordon Christensen, and an independent evaluator of dental products for CR. Dr. Ruiz is a Fellow of the AGD and practices General Dentistry in the Studio District of Los Angeles, where he treats many stars and entertainers. He lectures both nationally and internationally on aesthetic dentistry and leadership. He can be reached at (818) 558-4332 or via e-mail at ruiz@drruiz.com.
Disclosure: Dr. Ruiz reports no conflict of interest.











