To set up the premise and discussion points for this article we will begin simply with a description of 2 cases involving orofacial pain, and then describe the condition known as burning mouth syndrome (BMS).
CASE 1
Mrs. F was seen at our university’s orofacial pain clinic with complaints of facial pain following a routine endodontic procedure. She explained that soon after root canal therapy on a lower molar, she began to experience tingling and then aching and burning pain in and around the tooth. It spread over her entire lower jaw and face. After retreatment of the en-dodontia, an extraction, then 2 more endodontic procedures, followed by one more extraction, she was finally referred for an orofacial pain evaluation. After 2 years of suffering and multiple procedures, she was diagnosed with a neuropathic pain disorder and treated successfully with medications.
CASE 2
Ms. S is a 43-year-old woman suffering from fibromyalgia and what she told us was TMJ. She presented with a headache that she was sure could be relieved by a new “TMJ appliance.” The 3 devices she brought with her to the examination, carefully wrapped in a plastic sandwich bag, no longer were working. She was told by her physician to get a new one. After an extensive history and physical examination in our postdoctoral orofacial pain clinic, it was determined that her pain was not of dental or masticatory origin, but had characteristics of a new-onset headache disorder of a possibly ominous nature. A referral for brain imaging disclosed an intracranial lesion as the source of her complaints. She was immediately referred for medical management. Treating her for a temporomandibular disorder would have been inappropriate and dangerous, and would delay her from obtaining relief from her symptoms. An accurate diagnosis was required, and in this case could have been life saving.
BURNING MOUTH SYNDROME
 |
 |
| Figure 1. (A. left) The innervation of the tongue is supplied by the trigeminal (lingual) nerve (CN-V3), which is responsible for touch, temperature, and pain. Taste is mediated by the facial (chorda tympani) nerve (CN-VII). Normally these nerves act together for a balanced sensation of nonpainful stimuli and taste. (B. right) In one form of burning mouth syndrome, dysfunction or diminished activity of the chorda tympani, possibly associated with altered taste, may allow an increased perception of lingual nerve activity. This results in a sense of burning in the absence of any observable intraoral lesions. In this case the intraoral burning, or burning mouth syndrome, is considered a neuropathic pain disorder. |
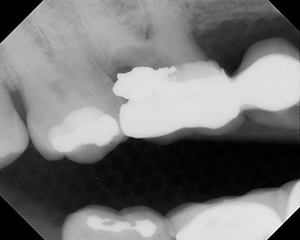
Another, and occasionally disabling, orofacial pain complaint is burning mouth syndrome (Figure 1). Affecting approximately 40% of premenopausal and perimeno-pausal women, this condition is characterized by a sense of intraoral burning, and persists in the absence of any local pathology (Figure 2) or systemic illness. Now perceived to be due to a dysfunction of the innervation regulating taste sensations, this perplexing disorder is under study by orofacial pain researchers around the world. Fortunately, although we are not clear on the mechanism of this disorder, there are effective treatments for managing BMS. Unfortunately, this knowledge is not widespread among clinicians who tend to see this population of patients.
The most important factor in effective treatment of BMS, or any other orofacial pain condition, is an accurate diagnosis. All too often we see BMS patients who tell us, “I was told I was depressed,” “I was told to learn to live with it,” or the worst, “There is nothing wrong with you. It’s all in your head.” These unfortunate misstatements by physicians and dentists not trained in orofacial pain take the last bit of hope from the suffering patient.
We can, however, offer these patients hope, as effective treatments are well-represented in the literature, even if mechanisms of BMS remain obscure. Of course, you can’t find what you don’t look for. Dr. Matthew Lark, president of the American Academy of Orofacial Pain, encourages dentists to seek the help of an orofacial pain practitioner when confronted with patients with unusual orofacial pain conditions.
DISCUSSION
Studies of chronic orofacial pain patients such as these find that these patients, prior to seeing an orofacial pain dentist, have seen an average of more than 5 other healthcare providers and have suffered their pain complaints for more than 4 years. The failure to diagnose and treat these patients results in substantial disability and suffering. In these, and countless other similar cases, we are often asked, “Why didn’t someone tell me this before? Why didn’t my physician or dentist know where to refer me?” We don’t have answers to these questions despite the fact that there are hundreds of orofacial pain dentists throughout the United States, as well as specialties in orofacial pain in many countries around the world.
Orofacial pain is a collective term used for a number of complex orofacial pain and dysfunction disorders, which include neuropathic pain, nonodontogenic tooth pain, musculoskeletal pain, neurovascular pain, referred pain, headache, oromotor dysfunction, and mandibular behavioral disorders, resulting in symptoms of chronic head, neck, and orofacial pain. The most common orofacial pain disorder involves temporomandibular disorders, but is commonly overlaid by other chronic complex pain conditions
 |
| Figure 2. Even patients with a normal-appearing tongue may complain of BMS. |
Historically, patients with complex chronic orofacial pain have not received adequate treatment by any medical or dental discipline, and these patients are often confused about whom to see for their pain. These patients often fall into the gray area where dentistry ends and medical disciplines begin. Generally, healthcare providers do not know who has the qualifications to treat these patients effectively. Although most dentists and physicians see orofacial pain patients, many will enlist the expertise of someone with additional training in orofacial pain. A survey of 405 dentists found 95% refer these patients to an orofacial pain expert. They also support orofacial pain becoming an ADA specialty by a ratio of 6:1.1 Another survey found that 55% of dentists usually refer orofacial pain patients for treatment to a practitioner with expertise in this field, and 55% feel that orofacial pain should become an ADA-recognized specialty.2 This broad support to recognize orofacial pain as a specialty may in part be due to orofacial pain diagnoses and therapies now being taught in most predoctoral and postdoctoral dental schools’ programs.3 Numerous other countries, including Brazil, Sweden, Korea, Costa Rica, and Thailand, have already designated orofacial pain as a dental specialty.1
In the United States alone, 7% of the US population (more than 13 million individuals) suffer from chronic orofacial pain.1 More than 3 million people annually seek treatment for chronic orofacial pain, with over 30% of them having a persistent complex pain disorder that warrants evaluation and treatment by a healthcare provider with additional orofacial pain training.4
Fortunately, dentistry has taken the lead in providing care for patients suffering from these conditions by developing the field of orofacial pain in the United States. Dental universities have responded to this critical need by developing 13 advanced orofacial pain training programs in the United States and Canada, from which many orofacial pain experts graduate each year. Universities have established orofacial pain clinics in nearly every dental school and created 2-year advanced programs in 11 dental schools. Major dental organizations, such as the American Association of Dental Schools, recognize orofacial pain, and the United States Armed Forces has established orofacial pain as an advanced field of dentistry.
Scientific advances are progressing at a rapid pace due to our improved understanding of orofacial pain, its epidemiology, and its treatment. The American Board of Orofacial Pain (ABOP) has established a rigorous examination and credentialing process for orofacial pain dentists to certify their knowledge and capabilities. More than 300 dentists in the United States and abroad have obtained their ABOP Diplomate in Orofacial Pain status and are focusing their careers on orofacial pain.
If orofacial pain were to become an ADA-recognized specialty, then providers and patients would be able to identify a qualified orofacial pain specialist to utilize the broad-based diagnoses and interdisciplinary treatment necessary for these chronic, complex orofacial pain patients. As these providers demonstrate the ability to provide cost-effective therapy, insurers are more likely to offer policies that provide coverage for orofacial pain.
CONCLUSION
Strategies and educational programs are in place to provide clinicians with a basis for providing scientifically based diagnosis and management of orofacial pain disorders. With recognition of this emerging field in dentistry we can ensure the quality of care provided by properly trained clinicians, improve patient therapeutic outcomes, enhance patients’ quality of life, and reduce inappropriate recommendations and treatment.
FURTHER READING AND RESOURCES
The fourth edition of Guidelines for the Assessment, Diagnosis, and Management of Orofacial Pain, published by the American Academy of Orofacial Pain (AAOP), is now available from Quintessence Publishing (quintpub.com). If you would like to learn more about this emerging specialty, or for a list of ABOP Diplomates in your area, visit the AAOP (aaop.org) or ABOP (abop.net) Web sites, or contact the AAOP by calling (856) 423-3629.
References
- Fricton JR, Okeson JP. Broad support evident for the emerging specialty of orofacial pain. Tex Dent J. 2000;117:22-25.
- Simmons HC III, Kilpatrick SR. A survey of dentists in the United States regarding a specialty in craniofacial pain. Cranio. 2004;22:72-76.
- Okeson JP. Growing into a new specialty: one person’s perspective. Cranio. 2007;25:229-231.
- Fricton JR. The field of orofacial pain: should it be a specialty? Cranio. 1997;15:183-184.
Dr. Heir is a past president and a Fellow of the American Academy of Orofacial Pain, and immediate past president and a Diplomate of the American Board of Orofacial Pain. He received his DMD from the University of Medicine and Dentistry of New Jersey (UMDNJ), where he is currently a clinical professor in its Department of Diagnostic Sciences and Division of Orofacial Pain. He is a co-director of the orofacial pain graduate program and is director of the Orofacial Pain Clinic. He is the director of the oral biology postgraduate core module on orofacial pain and director of the second-year undergraduate orofacial pain lecture series. He can be reached at (973) 972-3418 or by e-mailing heirgm@umdnj.edu.
Dr. Wright is an assistant professor at the University of Texas Health Science Center, San Antonio (UTHSCSA). He completed a 1-year general dentistry residency, a 2-year TMD fellowship, and a 2-year TMD research fellowship. He is UTHSCSA’s course director for their courses on TMD, occlusion and TMD, and dental anatomy and occlusion, and the module director for the stabilization appliance rotation. He is the primary author of 24 journal articles as well as the textbook Manual of Temporomandibular Disorders. He can be reached at (210) 567-3255.