“Black hairy tongue” (BHT), also known as lingua villosa nigra, hyperkeratosis of the tongue, nigrities linguae, keratomycosis linguae, and melanotrichia linguae, is a benign disorder characterized by hypertrophy of the filiform papillae. Lusitanus, who is credited with the original description of black hairy tongue, reported this condition in 1557. He reported finding hairs of the tongue which would regrow upon being removed.1-8 There are a number of precipitating factors. The etiology of this condition is most commonly due to the side effects of certain drugs, including antibiotics, antihypertensives, psychotropics, and oxygenating oral mouth rinses. Oxidizing agents include sodium perborate, sodium peroxide, and hydrogen peroxide. Tobacco use, poor oral hygiene, and various stains related to certain foods and beverages have also been related to the occurrence of BHT, but not in regard to the case report described in this article.5-8
When patients are using multiple medications, it is necessary for the clinician to investigate the potential causes by gathering an accurate history and using that information to gain an understanding of this condition. A case is presented in which a patient developed black hairy tongue following exposure to multiple pharmacological agents.
 |
|
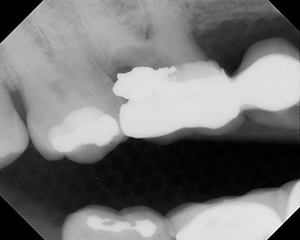
Figure 1. Appearance of patient’s tongue on initial presentation. |
 |
|
Figure 2. Appearance of patient’s tongue after 2 weeks of therapy. |
ETIOLOGY, DIAGNOSIS, AND TREATMENT
Even though the cause of BHT is unknown, several precipitating factors have been implicated in the pathogenesis of the disease entity. The hairy appearance is due to the elongation of keratinized filiform papillae, which may have different colors varying from white, yellow, brown, to black depending upon the involved extrinsic factors (ie, tobacco, coffee, tea, or food) and intrinsic factors (ie, chromogenic organisms in the normal flora).2,3 In 1925, Prinz4 suggested that BHT results from a predisposition of the surface of the tongue to irritation by specific substances. Accordingly, the irritation leads to hypertrophy of the filiform papillae, and the enlarged papillae become easily stained with available pigments. Prinz opined that the main source of the pigments was a local reaction between the decomposition products of food and iron (secondary to blood within the mouth). In verifying his hypothesis, he applied an irritant twice daily to the tongues of 6 students. Within a week, one student showed a slight enlargement of the filiform papillae of the tongue. The student then intentionally slightly injured his gingiva with a toothpick to allow blood to contaminate the elongated tongue papillae. A marked enlargement of the papillae with a deep brown stain was noted. Since 1925, knowledge of the etiology of BHT has not improved markedly.1,5 Several authors have suggested that black discolorations result from the growth of pigment-producing organisms in the oral cavity.6,7
BHT is not difficult to diagnose. However, the etiology of this condition is poorly understood, and successful therapy may prove challenging. Powell8 suggested that it is necessary to distinguish between true hairy tongue and “pseudo-hairy tongue” in the sense that in the latter there is brownish-black discoloration of the tongue without the exaggerated elongation of the filiform papillae.
Marabe, et al9 suggested that the condition seems to be related to either increased keratin deposition or delayed shedding of the cornified layer. The discoloration may vary from yellow to brown to black. The discoloration and elongation of the filiform papillae usually involves the anterior and middle thirds of the dorsal tongue. Factors associated with BHT include drugs such as antibiotics (penicillin, cephalosporin, chloramphenicol, streptomycin, and tetracycline), corticosteroids, oxygenating mouth rinses, nonsteroidal anti-inflammatory drugs and psychotropics, as well as tobacco, vegetable dyes, radiation, and most importantly, poor oral hygiene.10-12 BHT is also observed with much greater frequency in drug addicts, alcoholics, and patients infected with the human immunodeficiency virus.11
The medications noted above also have other oral side effects, which can include xerostomia, stomatitis, sublingual adenitis, and parotid swelling.13 Other contributing factors include antacids, toothpaste containing neomycin, and radiation therapy.9-12 The discontinuation of smoking, oxygenating mouth rinses, and antibiotics will usually result in resolution of the condition.10 According to various studies,13-16 the incidence of BHT ranges from 0.5% in the United States to 12.8% reported in a population of Israel male geriatric patients, and up to 57% within a population of imprisoned Greek drug addicts. There is no racial predilection to BHT, and even though it is reported more often in males, it is not uncommon in females, especially those who drink coffee or tea, and/or those who use tobacco. Also, the incidence and the prevalence of hairy tongue increases with age, possibly because a higher percentage of the population engage in activities (eg, using tobacco, drinking coffee or tea) that predispose to the condition.16
Sarti, et al5 noted that certain suggested treatments for BHT have been mentioned as possible causative agents. They suggest that all predisposing factors should be eliminated and the dorsum of the tongue should be brushed twice daily using 3% hydrogen peroxide or baking soda. Other authors have suggested topical triamcinolone acetonide (ie, Kenalog, Aristocort) twice daily after wiping the tongue dry, while others have recommended topical antifungal agents.5-8
CASE REPORT
A 68-year-old male presented to a dental specialty clinic with chief complaint of “black tongue.” The condition was observed first by the patient’s otolaryngologist approximately 9 months previously. The patient was being treated for a sinus infection and was taking several antibiotics at the time. The physician prescribed an over-the-counter mouth rinse which was not effective in decreasing or eliminating the condition. The patient was referred to another physician who recommended a probiotic (a dietary supplement containing potentially beneficial bacteria, acidophilus, or yeast, which is also found in yogurt), which did not help. On his own, the patient attempted a combination of mouth scraping and baking soda, but also to no avail. The condition persisted for 6 months after antibiotic therapy had been discontinued. The condition waxed and waned but never completely resolved.
The medical history appeared to be contributory, due to the probability that one or more of the patient’s medications may have influenced the condition. The medical history was positive for atrial tachycardia, for which the patient was taking cou-madin, irbesartan, labetalol, digoxin, and simvastatin. The patient was also taking flunisolide and loratadine for nasal congestion, and providone-iodine, hydrogen peroxide, and a commercial mouth rinse with essential oils and alcohol for oral hygiene, in conjunction with brushing and flossing. He had prostate cancer surgery 4 years previously, for which he was being monitored. Further, there was a history of penicillin and pollen allergy. The patient did not smoke but noted moderate drinking of alcohol, particularly red and white wines.
Clinical examination revealed no regional lympha-denopathy. The posterior and middle dorsal tongue was noted for a black hairy tongue appearance (Figure 1). The posterior and middle thirds had black staining of the filiform papillae. The left parotid salivary gland did not demonstrate function, while the right parotid gland dem-onstrated limited function. The submandibular salivary glands and minor salivary glands of the lips demonstrated normal function. The remaining oral tissues appeared to be within normal limits. The patient was presently utilizing a tongue scraping device.
A diagnosis of “black hairy tongue” and “relative xerostomia” was made, and treatment recommendations were offered in the following order. The recommended therapy was to discontinue the commercial mouth rinse and periodontal antibacterial therapy, use the tongue scraper twice a day (rather than only once a day), and to begin dry mouth therapy which consisted of forcing fluids, drinking and sipping water, and the utilization of dry mouth products such as a salivary replacement gel. Furthermore, it was suggested to discontinue the use of toothpastes with additives such as triclosan and whiteners, as these additives can be caustic.17,18
The patient returned for a follow up appointment 2 weeks later. The condition had improved remarkably (Figure 2). It was the patient’s opinion that the improvement was mainly due to discontinuing the use of the oral rinses.
DISCUSSION
The antibiotics utilized for the treatment of the patient’s sinusitis may well have been one of the initiating factors of the BHT. Since the use of antibiotics had stopped 6 months earlier, these drugs could be eliminated as a continuation factor. It is likely that the concomitant use of oral rinses may well have compounded the pre-existing condition. Prolonged use of oxidizing agents such as sodium perborate, sodium peroxide, and hydrogen peroxide commonly contained in mouth washes have been associated with BHT.5,7,12 The efficacy of tongue scraping to remove black hairy tongue and other coatings has been reported,12,14 and may have helped resolve the condition, although this activity was increased and not initiated. The treatment of the patient’s relative xerostomia may have been beneficial with regard to his BHT.
The approach to treatment of BHT can vary. Of course, smoking cessation and attention to oral hygiene are advocated, but these were not factors in this case. Other investigators19,20 have suggested such therapies as topical podophyllin and tretinoin. However, both of these topical treatments have problematic side effects. The patient was advised to discontinue oxygenating mouth rinses, and the patient believed that discontinuing the mouth rinses was particularly helpful.
CONCLUSION
There are many possible causes of BHT. It is important for the clinician to take an accurate and detailed history in order to determine the most likely causal agents. The treatment should be individualized, based on the clinician’s assessment of the etiologic agents. Treatment should emphasize gentle debridement and discontinuing the drugs and rinses which may be precipitating factors. As the use of an oxygenating mouth rinse is a known causative and continuation factor, its discontinuation was strongly suggested. This case demonstrated successful resolution of the condition in a patient with a relatively complex history.
References
- Waggoner WC, Volpe AR. Lingua villosa nigra: a review of black hairy tongue. J Oral Med. 1967;22:18-21.
- Haring JI. Case #10. RDH Magazine. Nov 2004;24:62-70.
- Tinbos G. Oral changes associated with tobacco use. Am J Med Sci. 2003;326:179-182.
- Prinz H. Black tongue. Br Dent J. 1925;46:1265-1274.
- Sarti GM, Haddy RI, Schaffer D, et al. Black hairy tongue. Am Fam Physician. 1990;41:1751-1755.
- Pindberg JJ. Disorders of the oral cavity and lips. In: Rook A, ed. Textbook of Dermatology. 4th ed. Vol 3. St Louis, MO: Mosby-Year Book; 1986:2117-2120.
- Van der Waal I, Pindberg JJ, eds. Diseases of the Tongue. Chicago, IL: Quintessence; 1986:39-55.
- Powell FC. Glossodynia and other disorders of the tongue. Dermatol Clin. 1987;5:687-693.
- Manabe M, Lim HW, Winzer M, et al. Architectural organization of filiform papillae in normal and black hairy tongue epithelium: dissection of differentiation pathways in a complex human epithelium according to their patterns of keratin expression. Arch Dermatol. 1999;135:177-181.
- Hommes M, Hoskam JA. Diagnostic image (189). A man with a tongue disorder. Black hairy tongue [in Dutch]. Ned Tijdschr Geneeskd. 2004;148:984.
- Tamam L, Annagur BB. Black hairy tongue associated with olanzapine treatment: a case report. Mt Sinai J Med. 2006;73:891-894.
- Abdollahi M, Radfar M. A review of drug-induced oral reactions. J Contemp Dent Pract. 2003;4:10-31.
- American Dental Association. A-Z Topics: Chronic Fatigue Syndrome. Table 2. Dental-related side effects of medications commonly prescribed for chronic fatigue syndrome. http://www.ada.org/prof/resources/topics/chronicfatique/index.asp. Accessed November 19, 2007.
- Regezi JA, Sciubba JJ, Jordan RCK, eds. Oral Pathology: Clinical Pathologic Correlations. 4th ed. Philadelphia, PA: Saunders; 2002:85-108.
- Greenberg MS, Glick M, eds. Burket’s Oral Medicine: Diagnosis and Treatment. 10th ed. Hamilton, Ontario, Canada: BC Decker; 2002:116-125.
- Lynch D. Hairy tongue. eMedicine Web site. http://www.emedicine.com/derm/topic639.htm. Updated December 16, 2006. Accessed August 9, 2007.
- Kowitz G, Jacobson J, Meng Z, et al. The effects of tartar-control toothpaste on the oral soft tissues. Oral Surg Oral Med Oral Pathol. 1990;70:529-536.
- Skaare A, Kjaerheim V, Barkvoll P, et al. Skin reactions and irritation potential of four commercial toothpastes. Acta Odontol Scand. 1997;55:133-136.
- McGregor JM, Hay RJ. Oral retinoids to treat black hairy tongue. Clin Exp Dermatol. 1993;18:291.
- Langtry JAA, Carr MM, Steele MC, et al. Topical tretinoin: a new treatment for black hairy tongue (lingua villosa nigra). Clin Exp Dermatol. 1992;17:163-164.
Dr. Lawoyin is an associate professor within the Department of Oral & Maxillofacial Surgery at Howard University College of Dentistry, Washington, DC. He can be reached at dlawoyin@howard.edu.
Dr. Brown is a professor within the Department of Oral Diagnostic Services at Howard University College of Dentistry and an associate clinical professor within the department of Otolaryngology at Georgetown University Medical Center, Washington, DC. He can be reached at (202) 806-0349 or rbrown@howard.edu.