External resorption often creates severe bone loss that can affect prosthetic treatment planning. This is especially problematic when the area involved is in the anterior maxilla, because of its aesthetic prominence. The aesthetic concerns are further exacerbated when the lip line is high.
This article reviews a case where tooth No. 9 in a female patient had external resorption, with subsequent loss of the tooth. Bone grafting utilizing a demineralized freeze-dried bone allograft (DFDBA) putty was performed to augment tooth loss for the pontic area under a fixed partial prosthesis for ideal aesthetics and hygiene.
CASE REPORT
 |
| Figure 1. Periapical radiograph revealing external resorption on tooth No. 9. |
A 38-year-old female presented with pain and a fistula above her left central incisor, tooth No. 9. The medical history was unremarkable, and the patient appeared to be in good overall health. The patient was not taking any medications. Periapical radiographs revealed advanced external resorption associated with tooth No. 9 (Figure 1). The tooth had been re-implanted after trauma caused its removal 2 years previously. The patient had individual PFM crowns on teeth Nos. 7 through 10.
TREATMENT PLANNING
The options available for treatment of tooth No. 9 were discussed with the patient. These options included root canal therapy with a questionable prognosis, extraction with bone grafting for a dental implant, extraction with replacement with a removable prosthesis, or extraction and replacement with a fixed partial prosthesis with bone grafting for the area around tooth No. 9. The option chosen by the patient was to have tooth No. 9 extracted, the bone grafted, and a fixed partial prosthesis constructed for teeth Nos. 6 through 11. This option would stabilize the adjacent teeth and offer ideal aesthetics with minimal surgical intervention. The fact that the adjacent teeth already had fixed restorations played a large part in the treatment planning decision.
PRESURGICAL CONSIDERATIONS
In order to successfully graft bone for aesthetics and function, the author routinely utilizes the “keys” to bone grafting as published by Misch.1 The keys utilized in this case were: (1) utilization of an aseptic surgical protocol; (2) creating adequate soft tissue closure; (3) assessing the grafting defect size; (4) maintaining the space in a graft site; (5) allowing enough healing time; (6) creating a regional acceleratory phenomenon; and (7) allowing sufficient blood supply from the host bone and soft tissue.
TREATMENT PROTOCOL
The patient presented for treatment of a bone graft to follow extraction of tooth No. 9. A temporary prosthesis was also planned for teeth Nos. 6 through 11. Surgical draping of the patient was accomplished, and a strict aseptic protocol was adhered to throughout the procedure. Through utilization of an aseptic technique, exogenous bacteria are eliminated from the surgical site.
Blood pressure was recorded at 120/60 and the pulse was 65 bpm. Premedication consisted of dexamethasone 9 mg orally (this was taken the morning of the procedure to coincide with the body’s peak steroid level). The dexamethasone would continue for 2 more days with dosages of 6 mg and then 3 mg, respectively. A 2-g dose of amoxicillin was taken 1 hour prior to the appointment, subsequently followed by 500 mg tid for 7 days. Also, 800 mg of ibuprofin was taken 1 hour prior to the appointment. Three carpules of lidocaine 1/100,000 were administered via infiltration from teeth Nos. 6 through 11. The exising crowns were removed from teeth Nos. 7, 8, and 10, then teeth Nos. 6 through 11 were prepared for new crowns.
 |
| Figure 2. Atraumatic nonsurgical extraction, tooth No. 9. |
Tooth No. 9 was removed in a nonsurgical manner utilizing an atraumatic technique (Figure 2). The atraumatic extraction ensured that any adjacent walls of bone would not be removed unnecessarily. Inspection using an explorer revealed that extensive buccal plate was missing, as expected facial to tooth No. 9. Once a tooth is removed from its socket, the first step to successfully graft bone in its place is to evaluate the remaining walls of bone. The walls of bone that remain affect many subsequent decisions. Determination of the remaining walls of bone can be done through either flap surgery or simply examining the site with an explorer and/or a light.
Atraumatic extraction techniques include the use of periotomes, sectioning a tooth, orthodontic extraction, and forcep rotation. When all the walls of bone around a tooth are left intact, the grafting material is better contained, osteoprogenitor cells are more readily available, and immobilization of the graft is obtained more easily. These factors affect choice of grafting material, membrane necessity, provisionalization options for the graft area, and healing time. Factors that determine the remaining walls of bone are severity of infection present, anatomic variability, and the extraction technique utilized. Evaluation of the remaining walls of bone is the starting point to successfully graft an extraction site.
 |
| Figure 3. Papilla sparing incisions, offering a broad base flap with increased blood supply. |
Incisions for the flap were made using a No. 11 surgical blade utilizing a broad flap base (Figure 3). This flap design affords adequate blood supply to the reflected flap.
 |
 |
| Figure 4. Flap reflection revealing extensive destruction of the buccal plate from external resorption. | Figure 5. Decortication of surgical site to induce bleeding and growth factors. |
Flap reflection utilizing a Molt curette revealed extensive destruction of the buccal plate (Figure 4). In order to offer osteogenic pleuripotential cells via a blood supply to the graft site, the graft site was contoured using a Brassler H71 Bur with sterile saline irrigation (Figure 5). This bur-induced decortication offers improved graft integration. The graft site was further decorticated with a straight bur to enhance the regional acceleratory phenomenon (RAP).1 The RAP improves integration of the graft blood supply. The recipient graft site is ready to receive the grafting material of choice.
DFDBA putty (Grafton, Osteotech, Inc) was chosen after discussion with the patient revealed that she did not want a second site surgery. It was explained to the patient that autogenous bone via a block graft was more predictable. The DFDBA putty was the next best choice because it offers osteoconductive, osteoinductive, and space-maintaining potential without the necessity of a second site surgery. The DFDBA putty also offers ease of handling and reduced migration of material compared with particulate materials.2 Osteoconduction is bone growth from surrounding bone. Osteoconductive materials are biocompatible, but will not grow bone without adjacent bone cells to assist. Osteoconductive materials act as a biocompatible scaffold. Osteoinductive grafting materials create bone growth from osteoprogenitor cells under the influence of inducing agents from the host bone matrix.1 Figure 6 shows the extraction site preparation after recontouring with the Brassler H71 and the RAP.
 |
 |
| Figure 6. Extraction site condition after decortication with adequate bleeding observed. | Figure 7. Checking flap for tension-free closure after scoring the periosteum and expansion with Metzenbaum scissors. |
 |
 |
| Figure 8. Collagen membrane being placed for cell exclusion and graft containment. DFDBA putty can be seen under the collagen membrane. | Figure 9. PTFE interrupted sutures placed. |
 |
 |
| Figure 10. Healing of graft at 4 weeks. | Figure 11. Metal frame try-in of fixed partial denture at 3 months post graft. |
 |
 |
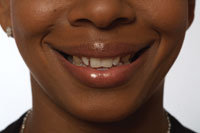
| Figure 12. Delivery of final prosthesis, prior to bleaching of remaining teeth and replacement of restoration on tooth No. 12. | Figure 13. Lingual view of final prosthesis showing close adaptation of final prosthesis to ridge. |
Primary closure of the surgical site both maintains the graft material and protects the site from exogenous bacteria. Primary closure was obtained through scoring of the periosteum and subsequent expansion with Metzenbaum scissors. Figure 7 shows checking of the flap for closure without tension. A collagen membrane (Biomend-Extend, Sulzer Dental) was utilized for exclusion of non-osteogenic cells from the graft site. The advantages of a membrane also include containment of the graft material and protection of the graft site in the case of incision line opening. A collagen resorbable membrane was chosen because of its handling characteristics, kindness to adjacent tissue, and avoidance of a second surgery. Further advantages of the collagen membranes are the chemotaxis offered for fibroblasts, the barrier effect for migrating epithelial cells, and the platelet aggregation they offer.3 Figure 8 shows the collagen membrane being placed. Gortex (polytetrafluoroethylene) sutures were utilized in an interrupted manner (Figure 9) to obtain primary closure. An acrylic temporary prosthesis was constructed, with consideration to creating an ovate pontic form.
Figure 10 shows healing of the grafted area at 4 weeks. Figure 11 shows the metal frame try-in and the close approximation of the fixed partial prosthesis for aesthetics and hygiene. The final prosthesis was delivered 3 months post grafting (Figures 12 and 13). A waiting period of 3 months allowed the grafted ridge to heal and stabilize.
CONCLUSION
External resorption can create tooth loss that can be especially troubling in the aesthetic zone. Through observing many of the keys to bone grafting, as published by Misch,1 bone in the anterior maxilla can be grafted to allow ideal function and aesthetics under a pontic area. Utilization of a DFDBA putty offers specific advantages as a graft material. The advantages of DFDBA putty are its osteoinductive and osteoconductive properties, ease of handling, and lack of migration of material from the graft site.
References
1. Misch CE. Contemporary Implant Dentistry. 2nd ed. St Louis, Mo: Mosby Inc; 1999:452-464.
2. Callan DP, Salkeld SL, Scarborough N. Histological analysis of implant sites after grafting with demineralized bone matrix putty and sheets. Implant Dent. 2000;9:36-40.
3. Owens KW, Yukna RA. Collagen membrane resorption in dogs: a comparative study. Implant Dent. 2001;10:49-50.
Dr. Tischler maintains a private practice in Woodstock, NY.He is a diplomate of the International Congress of Oral Implantologists, a fellow of the Misch International Implant Institute, a fellow of the Academy of General Dentistry, and an associate fellow of the American Academy of Implant Dentistry. He can be contacted at (845) 679-3706, or visit www.tischlerdental.com.