Fracture of the overlaying porcelain on a porcelain-fused-to-metal (PFM) prosthesis can be a challenging problem. Ideally, replacing the PFM prosthesis is the best treatment, but this may not be financially within the patient’s means.1 This becomes more costly with long-span prostheses. Repair of the damaged prosthesis may be the next best treatment and allows further function of the prosthesis until a more permanent solution can be rendered.
 |
 |
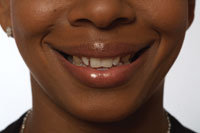
| Figure 1. The patient presented with a fracture of the cervical porcelain on a multiunit PFM removable prosthesis. (All photos provided by Dr. Allen L. Schneider.) |
Figure 2. Removable portion of the PFM prosthesis has been removed intraorally, showing the fixed metal copings on the abutment teeth used to retain the removable portion. |
Loss of a portion of the porcelain from the prosthesis creates an aesthetic issue that may be corrected at chairside using adhesive materials.2 Surface damage to the PFM may be broken into 2 categories, depending on which type of material is exposed. The first category is porcelain chipping. This is identified by a piece of missing porcelain with no exposure of the underlying metal substructure. The second category is porcelain debonding, where the porcelain fracture has exposed an area of metal substructure (Figures 1 and 2). The category of damage determines how the surface to be repaired is treated to increase retention of the overlaying material.3
PORCELAIN CHIPPING
This type of repair requires bonding to the remaining porcelain and is more difficult to achieve if the area comes into occlusal contact. Small chips at the cervical area are easier to repair and less likely to debond due to lower loading forces being placed on this area during mastication. When the chip involves the incisal edge, preparation extending onto the lingual surface will provide more bulk for the repair in the area where mastication forces work to debond it. These can prove challenging, as incisal chips may have occurred due to the occlusal scheme and excursive contacts.
Repairs when the damage is confined within porcelain are initiated by roughening with a coarse diamond to create some mechanical retention.4 A silane agent has been recommended to activate the porcelain surface and increase bondability between the porcelain and adhesive.
PORCELAIN DEBONDING
 |
 |
| Figure 3. Exposed metal has been roughened with a diamond in a high-speed handpiece to increase mechanical retention. | Figure 4. Further mechanical retention is achieved by sandblasting the exposed metal and surrounding porcelain margins. |
These types of repairs require bonding to 2 different surfaces—metal and porcelain. As with porcelain chipping, repair is initiated by roughening both the metal and porcelain surfaces. A coarse diamond is moved over both the porcelain and metal to receive the repair (Figure 3). A carbide bur may be used to create small, retentive dimples in the metal. If necessary, penetration of the metal to the underlying tooth structure may be done to increase retention. Application of aluminum oxide in an air-abrasion micro-etcher will create micro retention to augment the macro retention placed by the diamonds and carbides (Figure 4).
 |
| Figure 5. Metal Primer II is applied to the exposed metal to increase bond strength of the resin used to repair the missing porcelain. |
Exposed metal is treated with Metal Primer II (GC America), applying 2 coats and allowing each coat to dry for a few seconds (Figure 5). Metal Primer II contains a special monomer (MEPS thiophosphoric methacrylate), which promotes bonding by penetrating the metal alloy and co-polymerizing with the overlying resin to produce both a mechanical and chemical resin-to-metal bond. The improved tensile bond strength from alkane thiol molecule absorption significantly enhances the normal mechanical bond of the overlying resin. This primer can be used with either nonprecious or precious alloys, eliminating the need to tin plate exposed metal prior to bonding.
 |
| Figure 6. Ceramic Primer is applied to the porcelain margins surrounding the exposed metal to increase resin bond strength. |
Next, Ceramic Primer (GC America) is mixed (a drop from bottles A and B mixed together prior to application) and applied to the porcelain margins to receive bonding (Figure 6). This is allowed to dry for several seconds prior to the next step in the repair process. The Ceramic Primer activates the porcelain surface, silanating the porcelain and depositing methyl-methacrylate, which will increase bond strength to the ceramic surface. Contact of Ceramic Primer with metal will not hamper the bond to the pretreated metal surface.
 |
| Figure 7. A thin layer of flowable composite resin is applied over the exposed metal and porcelain margins, then cured. |
A flowable composite resin (Unifil Flow, GC America) is flowed in a thin layer over the treated metal/ceramic surfaces and cured with a hand-held curing light (Figure 7). Use of a flowable resin allows locking into the mechanical retention previously created and will permit some masking of the metal’s gray color. Use of a white opaque shade rather than a tooth color may be more beneficial to masking. Because the layer of flowable is very thin, the brightness of the white opaque flowable will not be difficult to neutralize with the overlying composite.
 |
 |
| Figure 8. A microhybrid composite resin is incrementally placed to cover the exposed metal and porcelain margins. | Figure 9. Composite instruments are used to achieve a normal contour. |
Next, a microhybrid composite (Gradia Direct, GC America) in a shade to match the adjacent porcelain is applied and sculpted to full contour of the desired final result (Figures 8 and 9). Because the layer of microhybrid will be less than 2 mm in thickness, it can be placed in bulk; incremental layering is not necessary. Thorough curing with a hand-held curing light is performed.
 |
 |
| Figure 10. Following final shaping with rotary instruments, flowable resin is applied to the repaired surface. | Figure 11. Completed repair of the fractured removable prosthesis. |
 |
| Figure 12. Repaired prosthesis intraorally. |
Finishing is accomplished using diamonds and finishing carbides in a high-speed handpiece. A final coat of flowable composite is applied over the repair to provide a smooth, aesthetic surface (Figures 10 to 12). Occlusion should be checked, specifically contact with the incisal edge during both centric and lateral excursions. All occlusal contacts should be removed from the repair material and kept on sound crown surface.
DISCUSSION
Damage to PFM prostheses may be multicausal.5 Porcelain chipping may be the result of contact with a harder substance loaded at an angle to the porcelain surface (shearing forces), causing micro cracks to spread, and leading to visible loss of porcelain. Porcelain debonding also may result from shearing loads. Another possible cause of chipping and debonding in fixed bridges is torque placed on the prosthesis under function. Since porcelain is a stiff material, these torquing forces twist the cast framework microscopically, leading to failure either within the porcelain (through micro cracks) or at the porcelain-to-metal interface (due to their dissimilar properties). A repair made from composite resin, which has more flexural strength than porcelain, may tolerate these micro torsional strains and remain in function.
Occlusion plays a part in how successful the repair will be and how long it will last. Centric contacts should be kept off the repair material or its junction with the porcelain or metal when possible. Care should be taken to adjust lateral excursion contacts so that shear load can be minimized on the resin repair and a decrease in “pop-off” can be achieved.
CONCLUSION
References
1. Rosen H. Chairside repair of ceramo-metallic restorations. J Can Dent Assoc. 1990;56:1029-1033.
2. Galiatsatos AA. An indirect repair technique for fractured metal-ceramic restorations: a clinical report. J Prosthet Dent. 2005;93:321-333.
3. Yanikoglu N. The repair methods for fractured metal-porcelain restorations: a review of the literature. Eur J Prosthodont Restor Dent. 2004;12:161-165.
4. Burke FJ, Grey NJ. Repair of fractured porcelain units: alternative approaches. Br Dent J. 1994;176:251-256.
5. Ahmad I. Salvaging fractured porcelain crowns with a direct composite repair technique. Pract Proced Aesthet Dent. 2002;14:233-238.
Dr. Kurtzman is in private practice in Silver Spring, Md, and is an assistant clinical professor at the University of Maryland-Baltimore School of Dentistry, Department of Endodontics, Prosthetics, and Operative Dentistry. He has lectured both nationally and internationally on the topics of restorative dentistry, endodontics, dental implant surgery, and prosthetics, and has had numerous journal articles published in peer-reviewed publications. He can be contacted at dr_kurtzman@maryland-implants.com.
Dr. Schneider is in private practice in Springfield, Va, and is an adjunct instructor of the Restorative Department, Tufts University School of Dental Medicine. He lectures nationally and internationally and has had numerous articles published in peer-reviewed publications. He is a consultant to the VA in Martinsburg, WVa, as well as various major manufacturers in the field of restorative and implant dentistry. He can be reached at aldds@aol.com.
Disclosure: Dr. Schneider is a paid lecturer for GC America.
To comment on this article, visit the discussion board at dentistrytoday.com.