Did you read the title of this article and think, “Single-visit endodontics? Of course, I’ve been doing it for years. What’s so new about that?” If you perform single-visit endodontics, you are part of the change in attitude—from never attempting a single visit to considering it common and routine. What has changed to make single-visit endodontics acceptable? Was it new techniques or was it simply driven by economics?
The fact that there is now widespread acceptance of single-visit endodontics for most vital cases represents significant progress. Until recently, this was not acceptable under any circumstances. But what about teeth with necrotic and infected pulps? In our view, single-visit endodontics is acceptable treatment in most cases, both vital and nonvital. This position is becoming more widely accepted and will continue. After all, when a canal is well cleaned at the first appointment, what more is there to do?
This article discusses the consideration of single-visit endodontics as the norm and not the exception. It also addresses (1) the economics of single visits, (2) when it is not wise to attempt single-visit treatment, (3) what research tells us about single visits, and (4) what an instrumentation technique must do to predictably improve the chances of success.
THE ECONOMICS OF SINGLE-VISIT ENDODONTICS
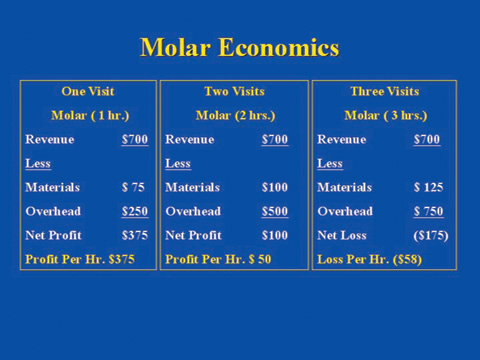 |
| Table 1. Molar economics showing the net profit per hour when treatment is completed in 1, 2, and 3 appointments. |
Based on economics, it is no surprise that single-visit treatment is becoming more widely accepted. Table 1 shows the economics of molar root canal treatment. With the fee remaining constant, regardless of the number of visits, there is a significant financial benefit for completing treatment in a single 1-hour visit because additional visits increase expenses, thereby reducing profits. A very profitable one-visit, 1-hour procedure becomes a loss when stretched to 3 visits. Assuming similar treatment results, patients also benefit. Dental visits, especially if not absolutely necessary, add an additional burden to their busy schedules.
THE BASICS OF SINGLE-VISIT ENDODONTICS
The basics of single visits were given to us in ENDO 101 and they are simple: make a correct diagnosis, clean the canal, and obturate it 3-dimensionally to prevent reinfection by the ever-present oral bacteria. We learned that the most important part of root canal treatment is to clean and disinfect the canal as well as possible. The basics have not changed at all.
To treat a tooth in one visit requires optimal cleaning and disinfection of the root canal system. Research tells us that this is accomplished most predictably when canal enlargement exceeds the diameter of the uninstrumented canal (mechanical cleaning), aided by the antimicrobial action of an irrigant (chemical cleaning). Infected tissue and bacteria located on canal walls and the superficial layer of dentinal tubules are removed by cutting away a thin layer of dentin. Any bacteria remaining deeper in the tubules are isolated by gutta-percha and sealer on the canal side and impervious cementum on the PDL side. Under these conditions, bacteria become inactive or die.
We disagree with the notion that single visits are not acceptable in infected cases and that medicaments must be used between appointments to kill all bacteria. There is a problem with this position because committing ourselves to removing all bacteria all of the time puts us in an untenable situation. We would have to remove an excessive amount of dentin to deal with bacteria deep in the tubules and find ways to deal with those located in lateral canals, apical deltas, fins, and isthmuses. Realistically, this is not possible in a clinical setting. This leaves medicaments the task of doing what is impossible to do with instrumentation, but we have no assurances that they will be effective in these “hard-to-get-to” places either. We advocate cleaning the main canal as best we can during the first visit and forgoing trying to do what is often impossible. If a thorough cleaning and canal sealing can be completed in the first visit, additional appointments don’t seem justified without clear evidence that patients will benefit.
APICAL DIAMETER AND APICAL ENLARGEMENT
To best clean the most important part of the canal (the apical part), instrumenting to the correct size is required. The size should not be determined by canal curvature nor should it be kept as small as possible. Additionally, it should not be based on what a root canal instrumentation system can or cannot do. Ideally, the apical part of the main canal should be prepared with instruments large enough to obtain a clean canal. Research clearly shows an inverse relationship between instrument size and the number of bacteria remaining in the canal. As instrument sizes increase, the number of bacteria decreases. Clearly, an undersized apical preparation compromises treatment.
 |
 |
| Figure 1. (a) X-ray showing a failed root canal treatment; (b) One year after re-treatment to larger apical sizes (MB, ML = 55; D = 60). The apical lesion has healed. | |
 |
 |
| Figure 2. (a) X-ray showing a failed root canal treatment. The mesial canals are ledged and the obturation is short; (b) One year after re-treatment to larger apical sizes (MB, ML = 50; D = 90). The mesial canals are still ledged and the obturation is still short, but the lesion has healed. |
To best illustrate the importance of apical diameter, let’s review 2 cases. Figures 1a and 2a show radiographs of failed root canal treatments. When one of this article’s authors (Dr. Wildey) re-treated the teeth, he found the canals underprepared apically. He re-treated them to larger sizes (using LightSpeed instruments), first gauging (sizing) the canals’ apical diameters, then using the instruments’ tactile feedback to arrive at the final apical preparation sizes. The larger sizes ensured cleaner canals and the lesions healed (Figures 1b and 2b). These 2 cases provide convincing clinical evidence that apical canal diameter and apical canal enlargement sizes are critical elements of successful endodontics.
EVALUATING QUALITY
How do we evaluate the quality of root canal treatment when it can be so subjective? We believe that the final apical preparation sizes achieved with root canal instrumentation are a major determinant of quality and should be routinely included when presenting a case. Just looking at aesthetically pleasing x-rays is not enough to conclude that a case is done well. After all, we all know that x-rays are only 2-dimensional, and that when a case looks bad, it is, but when it looks good, it may or may not be good. Having the apical preparation sizes of all canals can help us decide.
At a course sponsored by Loma Linda University (January 2003), Dr. Wildey demonstrated how instrument design can help determine the appropriate apical preparation size. He and 4 other well-known endodontists treated maxillary molars (live) while the audience watched on 3 large screens. After making straight-line access as described in an earlier article by Senia and Wildey,1 Dr. Wildey instrumented the canals using the LightSpeed technique2 and obturated them with SimpliFill.3
The final apical preparation sizes of the maxillary molar Dr. Wildey treated at Loma Linda were MB-1 and MB-2 = No. 55; DB = No. 55; and Palatal = No. 60. Obviously, all 4 sizes are larger than traditional sizes—not determined on a whim or a guess but dictated by the original canal diameter. Knowing final preparation sizes will help us evaluate the quality of treatment more objectively. We have to break the habit of evaluating quality of treatment just by looking at x-rays.
WHAT DOES THE LITERATURE SAY ABOUT CANAL SIZES?
Science and logic support the principle that larger apical preparations clean canals better, but how do we arrive at the correct size in a clinical setting? One can start by consulting the literature.4-8 Tables 2 and 3 show the data collected from various anatomical studies. Your first thought about the sizes shown in both tables may be that they are too large. However, before arriving at this conclusion, it’s important to know that the canals were not measured at the foramen or at the narrowest point. In general, they were made approximately 1 to 2 mm from the anatomic apex (coronal to the apical constriction). Compare your final apical preparation sizes with the sizes shown in the literature. If you are consistently smaller, there is a good chance you are underpreparing canals.
Since there is mounting evidence that “bigger is better,” what has been holding us back from giving apical canal diameter (the “forgotten dimension”) the importance it deserves?9 Why do we persist in believing that canals of molars can be thoroughly cleaned with instruments of size 25 or 30 when there is much evidence showing that this is not so? We believe past history provides the answer. Dentists learned that instrumenting curved canals with rigid stainless steel instruments larger than a No. 30 very often resulted in mishaps such as ledges, zips, perforations, and blocked canals. The choice was easy: instrument only with the smaller sizes or expect to have some problems.
Flexible instruments made of nickel titanium (NiTi) now make it possible to safely instrument to larger apical sizes. However, proceed with caution. NiTi instruments can still transport and ledge canals, particularly with increasing tip sizes and tapers. Instrument design that takes maximum advantage of the material is a factor that should be considered.
BIGGER IS BETTER
“Bigger is better” means instrumenting apical canals to the correct size, a size that is usually larger than traditionally accepted. It means that bigger instruments are required to clean the canal 3 to 5 mm coronal to the constriction where the canal diameter is considerably larger than that of the constriction. Bigger is better does not apply to the apical constriction. The apical constriction, when present, is the narrowest part of the canal and should be instrumented (if desired) to a size just slightly larger than its existing “natural” diameter. And finally, bigger is better certainly does not mean over-instrumenting canals and subjecting roots to possible fracture. Because most of the chewing forces are concentrated coronally, a slight over-enlargement of the apical third of the canal (if it occurs) should not be clinically significant.
 |
|
Table 2. Suggested maxillary apical preparation sizes (ISO/ADA sizes). |
 |
|
Table 3. Suggested mandibular apical preparation sizes (ISO/ADA sizes). |
Our goal is larger and cleaner canals apically without removing excessive dentin coronally. This can be accomplished by using a flexible material (NiTi), a flexible noncutting shaft, and a short blade with a noncutting pilot tip. In the authors’ opinion, this design is best suited to follow the canal. Practitioners have been conditioned to believe that apical canal sizes are small even when research shows otherwise (Tables 2 and 3). If skeptical about the sizes given, we ask you to look at the very tip of instruments, sizes 20 through 35, then ask yourself if canals are really that small. Most likely you will appreciate just how small these sizes really are and intuitively accept the fact that apical canals are larger in most cases.
BEING COMFORTABLE WITH SINGLE VISITS
We would like to make it clear that even though we believe in the concept of single-visit treatment, there are certain exceptions. We avoid single visits when the following conditions are present: (1) cellulitis, (2) acute apical abscess requiring incision and drainage, (3) severe pain when the tooth is lightly touched, (4) a weeping canal that cannot be dried, and (5) difficult cases that extend beyond our allotted time and the patient’s tolerance.
To be comfortable with single-visit treatment requires an understanding of when it is not a good idea and the manner in which the major elements of root canal treatment influence success and failure. The 2 major components of canal instrumentation are working length and final apical preparation size (canal diameter). Let’s discuss their role in single-visit endodontics.
Working Length: Must It Be Perfect or Is There a Biological Tolerance?
Let’s look at the case shown in Figure 2 again and examine how it relates to working length. The pretreatment x-ray (Figure 2a) shows both mesial canals ledged and obturated short. Upon re-treatment, Dr. Wildey was unable to bypass the ledges, resulting in a working length very similar (short) to the treatment that failed. Even though the mesial canals were re-obturated short because of the ledge, the lesion healed (Figure 2b). This strongly suggests that a “biological tolerance” exists for working length if canals are well-cleaned and sealed. Our highly effective body defense system can promote healing even when the working length is not ideal.
Let’s further discuss working length. Where is the ideal working length in relation to the apical foramen? Is the ideal length slightly beyond the foramen, flush with the foramen, or 0.5 to 1.0 mm short of the foramen? (Since the apical foramen marks the end of the root canal, working lengths can be more precisely located when referenced to the foramen rather than the apex.) What working length will ensure greater success given the same quality of canal instrumentation and obturation? There is abundant clinical and research evidence to support that there is a biological tolerance for working length. In other words, the ideal length is not always possible to achieve, but if you are a little long or a little short, there is no convincing evidence that the case will fail just because of this.
Canal Diameter: Must It Be Perfect or Is There a Biological Tolerance?
Does the same “biological tolerance” for working length also hold true for canal diameter? Before answering, it should be pointed out that canal diameter is often considered the “forgotten dimension” of a 3-dimensional root canal system. A review of the literature reveals that much has been written about length control but very little about diameter control. This implies that many believe getting the working length correct is what matters most. But, in a 3-dimensional environment, the existing (preinstrumentation) canal size is a very important factor. If canal size is not considered during instrumentation, then exactly how can one accurately determine when instrumentation has achieved a clean canal?
 |
| Figure 3. A graphic depiction showing the area instrumented by a No. 50 instrument compared with that of a No. 25 instrument and the canal enlargement objective (cross-section). |
Can the body’s defense system cope successfully with a debris-filled, infected canal resulting from a size 25 master apical instrument being used in a size 50 canal? Figure 3 compares the cross sectional area of a root canal prepared to a No. 50 file with that of a No. 25 file. While it seems intuitive that the area cleaned by a No. 50 is twice as much as a No. 25, the area of the canal cleaned is actually 4 times larger! This is why a few instrument sizes smaller than the “ideal” size result in a large amount of underpreparation and why emphasis should be placed on instrumenting to the correct size.
 |
 |
| Figure 4a. X-ray showing a failed root canal treatment. All working lengths are acceptable. | Figure 4b. Six months after re-treatment to larger apical sizes (MB, ML = 50; D = 60). The apical lesions have healed. |
Our opinion is that there is little biological tolerance for apical preparation size with necrotic cases. The molar in Figures 4a and 4b is a good example. It failed even though it had been instrumented and obturated to acceptable working lengths (Figure 4a). When re-treated with similar working lengths but with larger apical preparations (mesials = No. 50; distal = No. 60), healing of the rather extensive lesion took place (Figure 4b). Underpreparation, as demonstrated in this case, results in a continuous battle between the periradicular tissues and bacteria and their toxins. The body’s defense mechanism is now dealing with a very different situation as compared to working length. When working length is not ideal but everything else is done correctly, there is no continuous battle. The bacteria are isolated, and in a well-cleaned and sealed canal, there is no apical recontamination. Apical underpreparation results in debris and bacteria remaining in the canal, making isolation with the obturation virtually impossible.
1 OR 2 APPOINTMENTS?
When canals are cleaned and disinfected at the first appointment, why not complete treatment at that time? Is there reason to expect a higher success rate with a second visit when a biologically acceptable level of cleanliness is attained at the first one? Wouldn’t delaying completing treatment until the second visit perhaps be counterproductive given the possibility of recontamination between visits? Let’s look at the science to answer some questions and help us decide.
The Science of Single-Visit Endodontics: Apical Sizes Revisited
Recent studies support larger apical preparation sizes to remove more infected tissue and bacteria10-13 and provide more canal space for more effective irrigation.14 Simply stated, preparing canals to larger apical sizes is the right thing to do, especially if single-visit endodontics is our goal.
More than 25 years ago, Kerekes and Tronstad provided evidence that root canals are much larger than once thought.4-6 Many years have passed, yet the myth remains that apical canals are very small and that instrumentation need only be to sizes No. 20 to 35 in most canals. More recent studies show otherwise.7,8,15 There are always exceptions, but they are the exception, not the rule.
Shuping et al11 found that molar canals prepared to a No. 36 or No. 46 with 0.04-taper NiTi instruments rendered only 61.9% of the canals bacteria-free even after irrigation with NaOCl. Their study concluded that larger apical preparations are required for better debridement and to give irrigants better access to the apical region. The investigators also noted that if a canal is not instrumented to an appropriate size, the purpose of using an antibacterial irrigant might be negated. Their findings certainly do not make a good case for single- visit endodontics when canals are underprepared.
Siqueira et al12 found that canals prepared to a No. 20 with 0.12-taper NiTi instruments resulted in only 66.5% of the specimens being bacteria-free. They stated that large preparations incorporate more anatomical irregularities and allow the removal of a substantial number of microbial cells from the root canal. They also mentioned that effective irrigation might not occur consistently unless the canals are sufficiently enlarged and that larger preparations may enhance the effects of irrigation in the apical third.
Rollison, Barnett, and Stevens13 prepared canals to No. 35 with 0.04-taper instruments and compared them with canals prepared with No. 50 0.02-taper instruments. They concluded that the 0.02-taper No. 50 instruments removed significantly more bacteria than the 0.04-taper No. 35 instruments. This study further demonstrates that apical preparation size really does matter.
Peters and Barbakow14 concluded that a larger canal preparation enabled more effective irrigation to remove the smear layer and debris. Card et al10 theorized that instrumenting canals to larger apical sizes would result in a significant reduction of canal bacteria and their study supported this theory. Canal preparation sizes ranged from No. 80 to No. 100 in cuspid and premolar canals and No. 60 in molar canals (using the LightSpeed system). The researchers concluded that a high percentage of infected canals would no longer harbor cultivatable bacteria when instrumented to the sizes used in their study. They also stated that with many teeth, this regimen may be a substitute for a 2-stage procedure utilizing an intracanal dressing between visits.
Taken together, these studies clearly indicate that as apical enlargement increases, the number of intracanal bacteria decreases. Is a figure of 89% to 100% reduction of intracanal bacteria, as determined by Card et al,10 good enough to justify single-visit endodontics? We believe it is. After all, there are no assurances that extending treatment to 2 or more visits will ensure a higher success rate, especially when canals are not well-cleaned.
ROLE 0F OBTURATION AND IRRIGATION
Successful single-visit treatment depends on effective mechanical debridement, chemical disinfection, and proper sealing of the canal system. Obturation can only be as good as the instrumentation, since filling material cannot occupy the same space as the debris left by poor instrumentation.
Effective irrigation can only be as good as the space available allows. A narrow, confined space inhibits a free exchange of irrigant. Larger apical preparations, so essential for canal disinfection and removal of debris, also enhance the action of irrigants. Since irrigation with pressure should never be used, larger preparations allow irrigating solutions to be placed closer to working length with added safety—another benefit and another reason that supports the idea that bigger is better.
CONCLUSION
Times have changed and new technology has given us instruments with better designs and materials. Numerous studies have shown that when flexible instruments are used, instrumenting to larger apical sizes produces minimal or at least not clinically relevant canal transportation. Yes, NiTi rotary instrumentation is a welcome change, and most dentists who have made the transition successfully wouldn’t want to go back to hand filing.
The ability of new rotary systems to reduce treatment time puts single visits within reach of most practitioners and prompts us to take another look at a concept that makes a lot of sense. But just because NiTi rotary systems are faster than hand instrumentation, this alone cannot justify single-visit endodontics. In this article, we tried to give valid, scientifically supported reasons for single-visit root canal treatment. Are we there yet? Think about it—and you decide.
Acknowledgment
The authors want to thank Mr. Steven S. Senia, BSIE, MBA, for his contributions to this article.
References
1. Senia ES, Wildey WL. “Straight-line” access: a must for faster and better endodontics. Dent Today. 2003;22:40-45.
2. The LightSpeed and SimpliFill Technique Guide. San Antonio, Texas: LightSpeed Technology Inc; October 2002.
3. Wildey WL, Senia ES. Simple, precise, and predictable root canal obturation. Dent Today. 2002;21:60-65.
4. Kerekes K, Tronstad L. Morphometric observations on root canals of human anterior teeth. J Endod. 1977;3:24-29.
5. Kerekes K, Tronstad L. Morphometric observations on root canals of human premolars. J Endod. 1977;3:74-79.
6. Kerekes K, Tronstad L. Morphometric observations on the root canals of human molars. J Endod. 1977;3:114-118.
7. Gani O, Visvisian C. Apical canal diameter in the first upper molar at various ages. J Endod. 1999;25:689-691.
8. Sabala CL, Biggs JT. A standard predetermined endodontic preparation concept. Compendium. 1991;12:656-663.
9. Senia ES, Wildey WL. Canal Diameter: The Forgotten Dimension. Dent Today. 2001; 20: 58-62.
10. Card SJ, Sigurdsson A, Orstavik D, et al. The effectiveness of increased apical enlargement in reducing intracanal bacteria. J Endod. 2002;28:779-783.
11. Shuping GB, Orstavik D, Sigurdsson A, et al. Reduction of intracanal bacteria using nickel-titanium rotary instrumentation and various medications. J Endod. 2000;26:751-755.
12. Siqueira JF Jr, Rjcas IN, Santos SR, et al. Efficacy of instrumentation techniques and irrigation regimens in reducing the bacterial population within root canals. J Endod. 2002;28:181-184.
13. Rollison S, Barnett F, Stevens RH. Efficacy of bacterial removal from instrumented root canals in vitro related to instrumentation technique and size. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94:366-371.
14. Peters OA, Barbakow F. Effects of irrigation on debris and smear layer on canal walls prepared by two rotary techniques: a scanning electron microscopic study. J Endod. 2000;26:6-10.
15. Wu MK, R’oris A, Barkis D, et al. Prevalence and extent of long oval canals in the apical third. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:739-743.
Dr. Senia has been published in national and international journals. He is a diplomate of the American Board of Endodontics, a former member of The Journal of Endodontics editorial board and a consultant for the NASA space program. After receiving both his BS and DDS degree from Marquette University in 1963, he reentered the US Air Force (he had prior service as a pilot) to take a GPR residency program at Chanute Air Force Hospital. In 1969, he received a certificate in endodontics and a master of science degree from The Ohio State University. He retired from the US Air Force in 1981 as a colonel and as chairman of endodontics at Wilford Hall Medical Center and accepted the position of director of the endodontic postdoctoral program at the University of Texas Dental School at San Antonio. He retired in 1992 as a professor and presently holds the title of clinical professor at the university.
Disclosure: Dr. Senia is the co-inventor of the LightSpeed root canal instrumentation and SimpliFill obturation systems.
Dr. Wildey is presently in an endodontic practice in the Dallas/Ft. Worth area. He earned his DDS degree from Georgetown University in 1976 and after graduation served 4 years as a general dentist in the US Air Force. In 1988, he received a certificate in endodontics from the University of Texas Dental School at San Antonio. He can be reached at docwild@aol.com.
Disclosure: Dr. Wildey is the co-inventor of the LightSpeed root canal instrument and SimpliFill obturation systems.











