With my great denture techniques, my patients don’t need adhesives, right? As a dentist, recommending denture adhesives is a cop-out, isn’t it? If my dentures aren’t right, denture adhesives can mask an imperfect fit, can’t they? Wrong on all counts. Proper use of a denture adhesive can and does improve the function and retention of even a well-fitting denture. It also helps maintain a patient’s self-confidence as well as his or her ability to wear the prosthesis. Further, the use of a denture adhesive can help patients increase their bite force significantly, which in turn allows them to chew more challenging foods. As clinicians, we should recommend adhesives because they help our patients.
It is important to realize, however, that adhesives or soft denture liners should not be used as a replacement for ill-fitting or improperly made dentures. As will be detailed throughout this article, use of adhesives in even well-fitting dentures can help increase your patients’ confidence level and overall quality of life.
ENSURING FIT AND FUNCTION
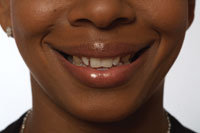
 |
| Figure 1. Lower denture with anterior teeth set outside the neutral zone. Notice that the probe is located at the center of the ridge. These dentures are not functional; accordingly, the patient will not be aided through the use of adhesives, relines, pads, or pastes. |
Before recommending a denture adhesive, determine proper fit and function of both the upper and lower denture bases and check that the denture flanges are not overextended or underextended, with appropriate ridge coverage. Remember, dentures over good ridges should have retention on their own. Besides extension problems, if the base of the new denture (out of occlusion) is nonretentive, your impression, model pouring, or processing may have caused the problem. Flange overextensions, pressure buildup on the tissue during impressions, and impression tray bleed-through during impressions can all compromise retention. Another element that can compromise retention is setting the denture teeth with too much lip support. No amount of adhesive or reline material will fix retention problems caused by denture teeth being placed outside of the neutral zone (Figure 1).
Denture occlusion also must be checked. Occlusal schemes that place excessive lateral forces on the ridges can cause pain, discomfort, and multiple adjustment appointments. Note that it is geometrically impossible to ensure proper occlusion of anatomical teeth without taking face bow records and a check bite—remounting the dentures. Most clinicians would never attempt full-mouth crown and bridge without face bow and lateral excursive records, yet many dentures are fabricated with 33o teeth and no such records. It is the opinion of this author that denture teeth with cusp angles of 15o or greater should not be used unless a face bow record is taken or the anatomical teeth are set against nonanatomical teeth in a flat plane. It also is impossible to set curves of Spee or Wilson accurately without face bow and lateral records. However, proper occlusion can be achieved without a face bow by using flat plane occlusion, which minimizes lateral forces on the ridges and decreases sore spots and many other problems.
DEFINING OBJECTIVES
When recommending the use of adhesives, have clearly stated objectives in mind so your patient will know what to expect. This author uses a percentage system for communication. Three scenarios follow:
Scenario 1: A patient presents with good ridges and well-fitting dentures. Tell this patient, “Your dentures are working at about 95%. This adhesive may bring you to 100%.”
Scenario 2: A patient presents with well-constructed dentures but poor retention because there is not enough connective tissue on the ridge or skeletal structure. In this case, explain to the patient that retention and function could improve from a 60% level to an 80% or even 90% level through the utilization of denture adhesives.
Scenario 3: A patient pre-sents with poor ridges and old, ill-fitting dentures (because of too much lip support, for ex-ample). This patient starts out at 40%. First, address the lack of ridge support by showing ridge resorption diagrams. Then give the patient a mirror (or take digital photos) to show him or her the ridges. Next, explain the qualities of properly constructed dentures and how denture fit and function would be improved to 70 or 80% with new dentures. At delivery, I would recommend adhesive that hopefully will help the patient achieve 90% fit and function.
TYPES OF ADHESIVES
Many types of adhesives are available. Powders, pads, creams, pastes, and cushions all find their way into our patients’ mouths with varying degrees of success.
Pads or cushions are thick, require a high level of manual dexterity, and can alter the vertical dimension of occlusion (VDO) and the occlusion of dentures. They also can put pressure on the tissue. If the denture fits well, and a 1- to 2-mm pad is placed inside of it, then something has to give: the tissue usually loses. These products should be avoided.
Powders work well, but many geriatric patients don’t have the dexterity to place the powder into their dentures properly. They also may not be able to see the powder, which makes using the correct amount difficult. Pastes or creams work best in this author’s geriatric practice. They are more visible and easier to place.
APPLICATION OF DENTURE ADHESIVE
It is important to teach each patient how to apply adhesive and how much to use. I recommend the following instructions:
 |
| Figure 2. Large upper denture with adhesive applied. |
(1) Apply denture adhesive in 4 to 6 small areas on the upper denture in amounts about the size of a pencil in diameter—one in the incisive papilla, one in each max-illary tuberosity depression, and one at one-half inch anterior to the posterior palatal seal. Super PoliGrip (GlaxoSmithKline), for ex-ample, works well, and this product’s Ooze-Control Tip pro-vides more control over the application of the adhesive to the denture surface, making smaller amounts easier to apply (Figure 2).
 |
| Figure 3. Lower denture with adhesive applied. |
(2) On the lower denture, place a total of 3 similarly sized formations—one in the midline and one on both sides of the denture—one inch anterior to the retromolar pads (Figure 3).
(3) It is beneficial to apply the adhesive to one denture at a time. Place the first denture with adhesive in the patient’s mouth and have the patient bite down against the empty denture to secure the denture before moving on to the next denture. If adhesive is added to both dentures, and they are placed in the mouth at the same time, when the patient occludes the first time, the dentures can then assume an incorrect and painful position over the ridges. However, if the patient can bite down on one denture with adhesive while the other denture is firmly sitting on the ridge, the correct denture position can be more easily maintained.
REMOVAL OF DENTURE ADHESIVE
In addition to proper use, the correct removal of a denture adhesive can make a significant difference in denture maintenance and care as well as the patient’s overall comfort level. Ideally, dentures should be removed, cleaned, and the adhesive replaced after every meal. Many patients do not or cannot comply with this ideal. Poorly retentive dentures may require continual refreshing of the denture adhesive. If a caregiver or a patient is refreshing the denture adhesive often, it may be a signal that relines or new dentures should be explored as options. Lack of proper adhesive removal or excessive refreshing of adhesive may result in the formation of a thick, hard layer of adhesive that is difficult to clean off of the denture base. This is exacerbated when dentures are exposed to air (ie, when they are left out and not placed in a denture bath with water). In those instances, as well as others where adhesive is used correctly, adhesive removal can be accomplished via the following steps:
(1) Using a denture brush and warm water, brush the dentures thoroughly. Wernet makes a good denture brush.
(2) Place the dentures in a denture bath and submerge in a mixture of warm water and denture cleanser. Polident cleanser (GlaxoSmith
Kline), for example, works well.
(3) Remove from bath, brush, and redeliver.
(4) If adhesive still re-mains on the dentures, brush them again before resubmerging in a new warm water-cleanser mix. Rinse and repeat this process until the adhesive is thoroughly removed.
THE IMPORTANCE OF COMMUNICATING WITH CAREGIVERS
With elderly edentulous patients, a clinician is very likely working with patients who are cognitively im-paired, whether from a stroke, Alzheimer’s disease, Parkin-son’s disease, or a host of other diseases and disorders. In this author’s geriatric practice, 47% of the patients have cognitive impairment. These instances may mandate direct communication with the caregiver, who is directly responsible for proper denture care, including use and removal of the denture adhesive. It is important to be especially watchful of these patients. Upon every visit they make to your office, ask yourself, “Are the dentures properly cleaned?” Improper cleaning results in a buildup of food, plaque, and adhesive that not only is unpleasant for the patient, but may be a significant health risk.
Many cognitively impaired patients also have swallowing and respiratory problems. Breathing through a mouth full of bacteria and old food adds to the risk of pneumonia, which can be deadly in the geriatric population. If and when improper cleaning is consistently noted, I do not recommend using adhesive and will in fact suggest its discontinuance. Placing more adhesive over old, unclean adhesive will result in more buildup and possibly more collected food and harmful bacteria.
Remember, caregivers can be husbands, wives, children, friends, nurses, or aides from nursing facilities or hospitals. Because these in-dividuals possess varying levels of traditional and dental education, it is important to communicate instructions clearly, offering clarification wherever possible. These instructions will play a large role in both the patient’s comfort and the caregiver’s comfort level.
CONCLUSION
While not intended as an enhancer for an ill-fitting denture, the proper utilization and removal of a denture adhesive can largely impact a patient’s comfort level, not to mention his or her confidence in wearing the prostheses. Prior to working directly with the adhesive, however, it is important to determine ex-isting denture fit and function, as this may dictate what a practitioner, caregiver, and/or patient can hope to accomplish through utilization of the adhesive. Further, whether communicating directly with a patient or his or her caregiver, taking the time to detail proper denture care clearly and provide appropriate tools for proper usage will benefit all involved.
Additional Reading
Ghani F, Picton DC, Likeman PR. Some factors affecting retention forces with the use of denture fixtures in vivo. Br Dent J. 1991;171:15-21.
Benson D, Rothman RS, Sims TN. The effect of a denture adhesive on the oral mucosa and vertical dimension of complete denture patients. J South Calif Dent Assoc. 1972;40:468-473.
Grasso JE. Denture adhesives: changing attitudes. J Am Dent Assoc. 1996;127:90-96.
Shay K. Denture adhesives. Choosing the right powders and pastes. J Am Dent Assoc. 1991;122:70-76.
Roessler D. Complete denture success for patients and dentists. Int Dent J. 2003;53(5 suppl):340-345.
Dr. Folse, a 1989 LSU Dental School graduate, has a mobile geriatric dental practice in Lafayette, La. He is a recognized national and international speaker on functional and efficient denture care, geriatric dentistry, dentistry for aged, blind, and disabled special needs patients, and oral health advocacy. He completed the Geriatric Dental Fellowship Program at Baylor in 1999 and is currently working with the United States Senate’s Special Aging Committee, Centers for Medicare and Medicaid Services, as well as the American Dental Association and Special Care Dentistry to nationally improve oral healthcare access and infrastructure for aged, blind, and disabled US citizens. In 2003 Dr. Folse co-testified with US Surgeon General Richard H. Carmona, MD, MPH, FACS, in a US Senate forum on the oral health of the nation’s seniors and continuously serves as an advocate for the United States’ most vulnerable populations. He can be reached at (337) 235-1333.