Oral Health America (OHA) has published a national report examining the factors impacting the oral health of older adults. With an expected 72.1 million seniors living in the United States by 2030, OHA’s A State of Decay, Volume IV illustrates progress in some areas and the need for continued action to ensure America’s rapidly growing population of seniors age healthily and independently, OHA reports. Its findings include:
- 33% of older adults have lost six or more teeth.
- 25 US states received a poor overall score based on six key performance measures.
- Minnesota, Wisconsin, Iowa, Connecticut, and Colorado all earned an “Excellent” composite score.
- Iowa and California jumped from 23 and 30 on the list of states with the best oral health, respectively, in 2016 to 3 and 9 in 2018.
- Wyoming, Delaware, West Virginia, New Jersey, Arkansas, Texas, Oklahoma, Louisiana, and Tennessee have the lowest overall scores, with Mississippi’s score being the least favorable.
- Alabama improved from 50 in 2016 to 29 in 2018.
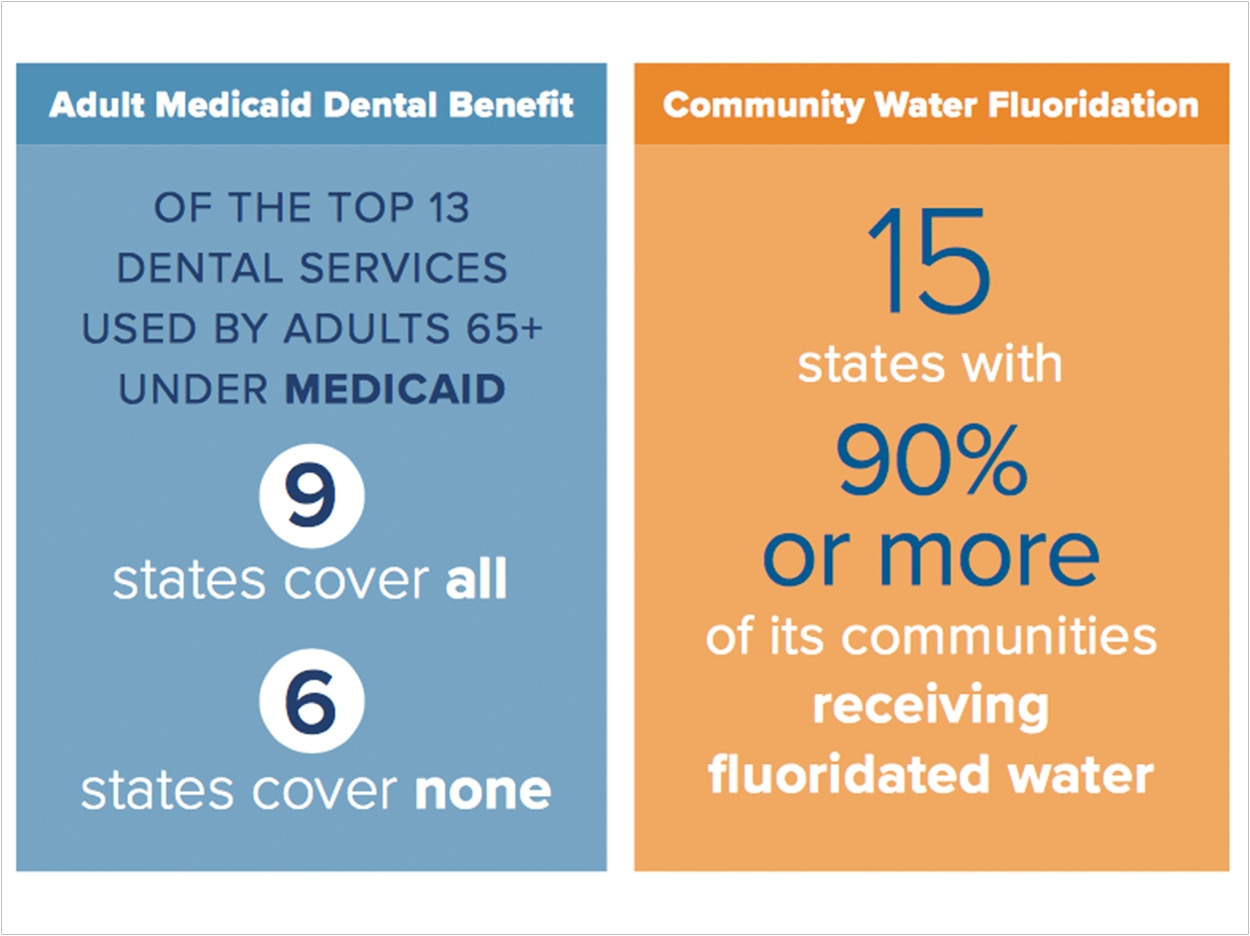
- Community water fluoridation increased from a state average of 71.9% in 2016 to 72.6% in 2018, which is a national increase of about 2.2 million people.
- Medicaid coverage of oral health benefits increased.
- Delaware and South Dakota provided no Medicaid benefits in 2016 but added some of the 13 services measured in the 2018 survey.
- More state oral health officials are including older adults in state oral health plans (SOHPs) and administering basic screening surveys that include seniors.
- 34 states have SOHPs, and 31 include older adults.
The report also shows that sociodemographic factors such as income, race, gender, and education play a critical role in oral health outcomes, OHA says. The data on severe tooth loss and recent dental visits, analyzed individually on a national basis, showed an association with household income. Low household income directly correlates with predicted measures of poor oral health. And as income levels rise, so does the probability of good oral health.
“Oral health for older adults is in fragile condition,” said Caswell Evans, DDS, MPH, associate dean for prevention and public health sciences at the University of Illinois at Chicago College of Dentistry. “Oral health for seniors is important for their diet, nutrition, self-esteem, socialization, and freedom from pain, among many other benefits.”
The report rates states as poor, fair, good, or excellent based on state-level data analyzing six variables impacting older adult oral health: severe tooth loss (loss of six or more teeth), dental visits, adult Medicaid dental benefits, community water fluoridation, state oral health plans, and basic screening surveys.
For the first time, the report has added a national analysis of the Centers for Disease Control and Prevention’s individual data on severe tooth loss and recent dental visits by considering associations with sociodemographic factors such as income, education, age, and gender.
Since the last report in 2016, state advocates have implemented action based on A State of Decay findings. More states are now taking steps to advance the oral health of older adults in their communities. Also, more states have commissioned surveys to measure the state of older adults’ oral health, added goals for older adults to SOHPs, increased community water fluoridation, and covered more adult dental services under Medicaid.
“Tooth loss and poor oral health are not inevitable during the aging process,” said Karen Tracy, vice president of strategic alliances and integrated communications at the Gerontological Society of America. “The Gerontological Society of America is pleased to see the growth in the number of states taking positive steps to advance their oral health services for older adults. And, through coordinated strategies in the education, practice, policy, and research arenas, millions of older adults can maintain their oral health for a lifetime and enjoy the far-reaching benefits of overall better health and quality of life.”
OHA ranked each state based on the health of its older adult population as measured by an overall state score. The 10 states with the highest scores were Minnesota, Wisconsin, Iowa, Connecticut, Colorado, North Dakota, Rhode Island, Michigan, California, and Vermont. The states with the lowest scores were Wyoming, Delaware, West Virginia, New Jersey, Arkansas, Texas, Oklahoma, Louisiana, and Tennessee, with Mississippi’s the least favorable.
To address the oral health needs of older adults, many states have created coalitions of stakeholders in aging, oral health, and public health to device specific strategies to address those needs.
For example, Iowa added an SOHP with SMART (specific, measurable, achievable, realistic, and time-related) objectives for older adults. It also completed a statewide older adult basic screening survey. It maintained support for all 13 common dental benefits for Medicaid beneficiaries age 65 and older and expanded its I-Smile Silver pilot, which helps older adults find providers, afford care, receive transportation to dental appointments, and overcome barriers related to medical problems or mobility.
California also restored the full set of 13 Medicaid services and created an SOHP with SMART objectives for older adults to carry the state through 2028.
The University of Alabama at Birmingham School of Dentistry is changing access, attitudes, and assumptions among the state’s residents and expanding its programs statewide, including more of its rural and vulnerable areas. The Alabama Department of Public Health created a new SOHP with SMART objectives for older adults as well.
And though it dropped from 46 in 2016 to 50 in 2018, Mississippi developed an SOHP to help establish a “culture of health that includes oral health.” Goals and objectives are guiding the efforts of state officials and stakeholders through 2021. And, the Office of Oral Health is creating a toolkit to educate leaders and residents about the importance of community water fluoridation.
“With half of the United States receiving a fair or poor rating relative to meeting minimal standards for the oral health of older adults, we must identify and address the steps needed to ensure the health of our burgeoning senior population,” said Beth Truett, president and CEO of Oral Health America.
“As depicted in this report, even with improvements by certain states, millions of older adults are still at a disadvantage when it comes to oral healthcare. Access to and utilization of care and to the coverage needed to pay for care is critical to increasing the overall health and wellness of America’s seniors,” said Truett.
According to OHA, federal and state policies are needed to address the underlying, systemic variables that prohibit older adults from achieving good oral health outcomes. The report recommends actions to promote healthy aging and independence for this rapidly growing cohort of America’s population, OHA says, including:
- Reinstate, establish, or maintain a comprehensive adult Medicaid dental benefit. If Medicaid does not provide the dental benefit these low-income older adults need, they are at risk of tooth decay, other serious medical problems, and unaffordable out-of-pocket expenses.
- Integrate comprehensive dental coverage in Medicare. Currently, Medicare does not cover routine or preventive dental services.
- Sustain or expand community water fluoridation. Community water fluoridation is the simplest, most equitable, and most cost-effective way for millions of Americans to protect their teeth and receive preventive oral healthcare.
- Include specific objectives for older adults in all SOHPs. An SOHP is key to establishing a vision for improving the oral health and well-being of the citizens of a state and its local communities, developing policies, and targeting actions.
- Conduct basic screening surveys of older adults in all states. Data from a public health surveillance system can be used to measure the burden of a disease, identify populations at high risk, and identify new or emerging health concerns, allowing states to make informed decisions regarding the oral health of their older adults.
“A State of Decay allows us to remain committed to ensuring oral health equity among all older adults, leveling the field to improve the quality of life for all,” said Michael Monopoli, DMD, MPH, MS, executive director of the DentaQuest Foundation.
“Everyone deserves the right to oral health screenings, diagnoses, and, most importantly, access to care,” Monopoli said. “This report provides a gauge of where we are and where we need to go to meet the unmet dental needs of older adults.”
Related Articles
Recommendations Aim to Improve Oral Health for Older Adults
Strategies Aim to Improve Oral Health for Older Adults
Older Americans Still Face Barriers in Oral Healthcare












